Central venous pressure (CVP) monitoring is used to measure the pressure from the right atrium or superior vena cava, normally via a central venous catheter (CVC) usually known as a central line. CVP monitoring is helpful in determining the adequacy of circulating blood volume and cardiac preload (Shah and Louis, 2020).
The insertion of a CVC to measure CVP is an invasive method of assessing patients' fluid status in critical care settings (Hill, 2018). A CVC is a catheter with a tip that lies within the proximal third of the superior vena cava, the right atrium or the inferior vena cava. These catheters can be inserted through a peripheral vein or a proximal central vein (Hill, 2018). The CVP can then be monitored electronically by connecting the CVC to a cardiac monitor, allowing a transduced waveform to be seen alongside a regularly updated numerical value. This is often practicable in critical care because patients in these settings frequently have a CVC in situ, which can be easily connected to a cardiac monitor to measure CVP. CVP can also be measured manually using a water manometer; however, this method is rarely used in clinical practice now.
CVP monitoring should be undertaken only by healthcare practitioners who have the knowledge and skills to do so. The Nursing and Midwifery Council's Code stipulates that nurses must always work within their scope of practice (NMC, 2018). Therefore, if nurses are expected to undertake CVP monitoring, they must have the necessary skills, knowledge, and clinical competence to do so, and practise in accordance with best available evidence.
Normal CVP for self-ventilating patients is 0–8 mmHg (Woodrow, 2019). Ideally, pressure should be measured as close to the atrium as possible, in the distal lumen of the CVC.
CVP monitoring in the critically unwell patient is established practice in critical care units; however, the traditional belief that it identifies ventricular preload and predicts fluid responsiveness has been challenged. Marik and Cavallazzi (2013) and Marik and Lemson (2014) identify that CVP is a poor predictor of haemodynamic responsiveness. However, others believe CVP provides important physiologic information for the evaluation of haemodynamic instability, especially in relation to venous return and the Frank-Starling law (Box 1) of the heart (Berlin and Bakker, 2015). Consequently, CVP monitoring is frequently carried out in patients receiving critical care and is very much common practice.
Rationale and considerations for CVP monitoring
CVP is used to assess adequacy of blood volume and is an indicator of right ventricular and, to a lesser extent, left ventricular preload. CVP also reflects the limit to venous return and informs about right ventricular function. As such, CVP measurements may be helpful to support and guide fluid management.
Nevertheless, CVP is also affected by thoracic, pericardial and abdominal pressures, which makes its interpretation complicated. When these pressures are high, transmural CVP is overestimated so may not reflect the true loading conditions of the right ventricle (De Backer and Vincent, 2018); however, it does indicate the limit to venous return and the back pressure of all extrathoracic organs. In particular, the risk of peripheral oedema, ascites, and renal and liver impairment is related to the absolute CVP value.
Shojaee et al (2017) completed a quasi-experimental study based on patients on mechanical ventilation who were evaluated with the aim of assessing the effect of positive-end expiratory pressure (PEEP) change on CVP and found there was a direct relationship between PEEP and CVP. It seems that sex, history of cardiac failure, baseline CVP level and hypertension do not have a significant effect on this.
Limitations of CVP
CVP is used routinely in critical care to guide decision-making on whether to administer intravenous (IV) fluid therapy. A systematic review indicated there were insufficient data to support CVP monitoring in critical care and concluded that CVP monitoring was not an accurate predictor of fluid responsiveness (Marik and Cavallazzi, 2013).
Factors other than rising intravascular volume, such as PEEP therapy, pulmonary hypertension, cardiac tamponade and pneumothorax, may increase CVP, so measurements may be inaccurate (Kupchik and Bridges, 2012).
Abnormal right atrial pressure in cardiac and respiratory disease, such as atrial fibrillation, atrioventricular block, tricuspid regurgitation, cardiac tamponade, chronic obstructive pulmonary disease and mechanical ventilation, can impede accurate CVP measurement (Gilbert, 2018).
Chlabicz et al (2019) recognise that fluid therapy in patients with congestive acute decompensated heart failure (ADHF) might be inappropriate and worsen the prognosis. They concluded that CVP-guided intravenous fluid therapy is a common practice that might be harmful and should be avoided in high-risk ADHF ‘cold-wet’ patients.
Lower CVP seems to be related with a poorer prognosis. The Surviving Sepsis Campaign no longer targets a CVP of 8–12 mmHg as a parameter in fluid resuscitation (Bennett, 2015).
While CVP remains a valuable measure in identifying a patient with impairment from right heart failure (Kupchik and Bridges, 2012), the CVP cannot be taken as a simple measurement.
Alternative methods of CVP monitoring
Depending on where a patient is being nursed, the availability of alternative methods of monitoring CVP may vary. Staff need to be competent to use such devices and interpret their data safety. The Code is explicit about ensuring patient safety by requiring nurses to work within their limitations and scope of professional practice at all times, as well as being required to maintain proficiency by undertaking training and continued professional development to meet revalidation requirements (NMC, 2018).
Transpulmonary thermodilution (TPTD) monitoring systems can measure multiple haemodynamic parameters using the concept of thermodilution (Pudjiadi, 2020). Hill (2018) gives pulse indicator contour cardiac output (PiCCO), lithium dilution cardiac output (LiDCO) and transoesophageal Doppler as examples of TPTD. However, although clinically relevant, not all critical care environments will use all of these devices. In addition, embedding specialist equipment requires expenditure as well as staff education and training. Therefore, only specialist equipment that is appropriate for the unit's speciality (eg cardiology and cardiothoracic critical care) would use these on a day-to-day basis.
The PiCCO system is less invasive than a pulmonary artery catheter (PAC) and involves the use of a peripheral arterial thermodilution catheter and large-bore peripheral or central venous access. The LiDCO method is also less invasive than the PAC and requires an arterial line and a CVC (Adam et al, 2017). These methods, if available, will generally be the first choice for measuring cardiac output. A PAC is used only on the rare occasions when arterial access with PiCCO or LiDCO is not possible because of the risk of arrhythmias, valve damage and ventricular perforation. However, it remains the gold standard for measuring cardiac output to which all other monitoring methods are compared (Scottish Intensive Care Society, 2017). Transoesophageal Doppler ultrasound is a reliable, efficient and non-invasive method of measuring cardiac blood flow and to determine stroke volume (Pudjiadi, 2020).
PACs, which are also known as pulmonary artery flotation catheters and Swan Ganz catheters, may also be also be used to determine right ventricular output (Hill, 2018). However, studies have shown minimal survival benefit associated with their use and increased mortality from complications associated with them (Gilbert, 2018). Therefore, PACs have been replaced by less invasive alternatives—PiCCO, LiDCO and transoesophageal Doppler (Woodrow, 2019).
Haemodynamic monitoring insertion sites
A CVC has a single lumen or multiple lumens, which provide vascular access for medication, fluids and monitoring. Both Zhang et al (2018) and De Backer and Vincent (2018) identified that CVC use is one of the commonest interventions in critically ill patients.
Reasons for inserting a CVC include for rapid administration of fluids during resuscitation, monitoring haemodynamic status, administration of vasoconstrictors or venosclerotic drugs and, using large-bore catheters, haemofiltration. In addition, some drugs or fluids, such as parental nutrition (including total parenteral nutrition), potassium solution, strong vasoconstrictors and chemotherapy drugs, must be given via a dedicated line on a CVC.
CVC insertion is an invasive technique and should be managed properly to minimise potential risks. Some catastrophic complications of CVC placement include pneumothorax, artery injury, bloodstream infection, thrombosis and human errors causing problems such as air embolism and unintentional guidewire embolisation (Firstenberg et al, 2015; Hill, 2018; Lister et al, 2020). Clinicians should weigh the risks and benefits when considering whether to insert a CVC.
A Cochrane review by Lai et al (2016) identified that CVCs impregnated with various forms of antimicrobials—antiseptics or antibiotics—reduced bloodstream infections by 2% and were therefore advisable when selecting a catheter.
A CVC is inserted by a competent practitioner—usually an anaesthetist or other medical professional—and positioned in the internal jugular vein, subclavian vein or via the femoral vein (Adam et al, 2017). It is advanced inside or as close to the right atrium as possible. There is rationale for each insertion site, so this should be selected based on the individual patient and their condition.
Internal jugular veins
Bannon et al (2011) suggest the internal jugular vein is often the access site of choice for central venous cannulation. Advantages include a superficial location, easy ultrasonic visualisation and a straight course to the superior vena cava (on the right). Internal jugular cannulation avoids the risk of subclavian ‘pinch-off syndrome’. Furthermore, for patients with renal failure, it avoids potential subclavian vein stenosis; this would preclude the use of the extremity of this vessel for haemodialysis access via an arteriovenous shunt or fistula.
Subclavian veins
Tsotsolis et al (2015) recognise that this site is often chosen as there are more recognisable anatomical landmarks, making device insertion easier. Because this site is beneath the clavicle, there is a risk of pneumothorax during insertion. A subclavian CVC is generally recommended as it is more comfortable for the patient.
Femoral veins
Patel et al (2019) suggest this site provides rapid central access during an emergency such as a cardiac arrest. As the CVC is placed in a vein near the groin, there is an increased risk of infection. In addition, femoral CVCs are reported to be uncomfortable and may discourage a conscious patient from moving.
Evidence for site selection
According to Pulm CCM (2020) in their review of randomised controlled trials, the subclavian position is by far the superior site, with fewer infections and less deep vein thrombosis (DVT), with less than half the composite rate (1.5 events per 1000 catheter-days) compared to the internal jugular (3.6 events) or femoral (4.6 events). However, patients undergoing subclavian vein puncture had three times the rate of pneumothorax, which required chest tubes for drainage (1.5% versus 0.5%), than those with internal jugular vein cannulations. That works out at a number needed to harm of 100 patients with subclavian CVC placements to cause an additional pneumothorax. It is also equivalent to a one in 67 chance of pneumothorax (subclavian) compared to one in 200 (internal jugular). Rates of pneumothorax in procedures carried out by less experienced operators outside their study would be expected to be higher.
Despite the widespread reluctance to use the femoral position for central line placement, rates of central line-associated bloodstream infection (Box 2) were no higher for femoral CVCs (1.2%) than for those using the internal jugular position (1.4%). However, femoral catheters produced symptomatic DVT 1.4% of the time, compared to 0.9% for the internal jugular position and 0.5% for the subclavian position.
Method of measurement
Contemporary management of CVP involves electronic CVP readings achieved by using a pressure transducer. Both manual and electronic methods are reliable if used correctly. The latter is generally used in critical care settings; the manual measurement is rarely used in contemporary practice so will not be discussed (Hill, 2018).
Electronic CVP readings are generated using a pressure transducer and displayed on a cardiac monitor as a continuous waveform alongside a numerical CVP value.
Preparing a patient for CVP monitoring
The equipment needed to measure CVP electronically is often assembled in a prepared kit containing a disposable transducer board and fluid lines. A valve port (or a three-way tap in surgical settings) is also required.
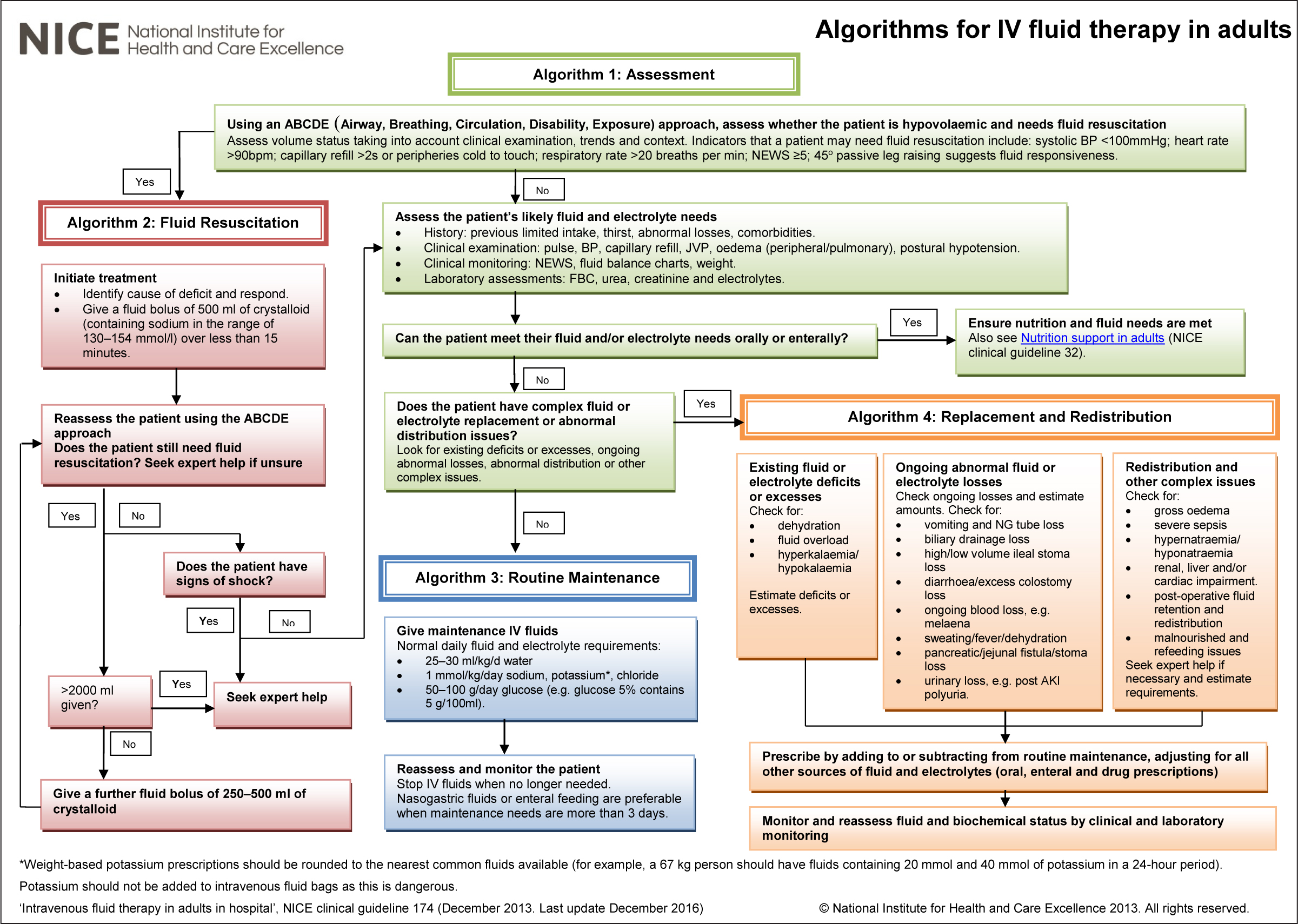
IV fluid should be administered using a pressure bag to prime the line of the transducer with fluid to ensure it contains no air and is patent. Initially, the transducer requires a pressure bag inflated up to 300 mmHg (Hill, 2018). This pressure will deliver 3-4 ml of IV fluid continuously through the transducer line to maintain catheter tip patency and prevent the development of clots in the distal lumen. Either 500 ml or 1 litre of IV fluid — usually 0.9% or 0.45% sodium chloride—should be prescribed and hung on an IV stand. It is important to consider the Intravenous Fluid Therapy in Adults in Hospital clinical guidance by the National Institute of Health and Care Excellence (NICE, 2016)(Figure 1, overleaf). The volume required will be specified on the pressure bag.
IV fluids should be maintained at more than a quarter bag full to prevent issues such as damp trace, low and/or inaccurate readings, loss of patency, air in the line and clots around the CVC tip (Hill, 2018). A ‘damp trace’ is the colloquial term for a trace that does not have the clear, characteristic elements of the CVP waveform because the transduced pressure has been disrupted.
The CVP line is then attached to the CVC and the cardiac monitor so that the CVP waveform and numerical value can be displayed. Most cardiac monitors will have a CVP block attachment; a health professional will select ‘CVP’ from the monitor menu then turn the CVP function on. A CVP line will appear on the screen.
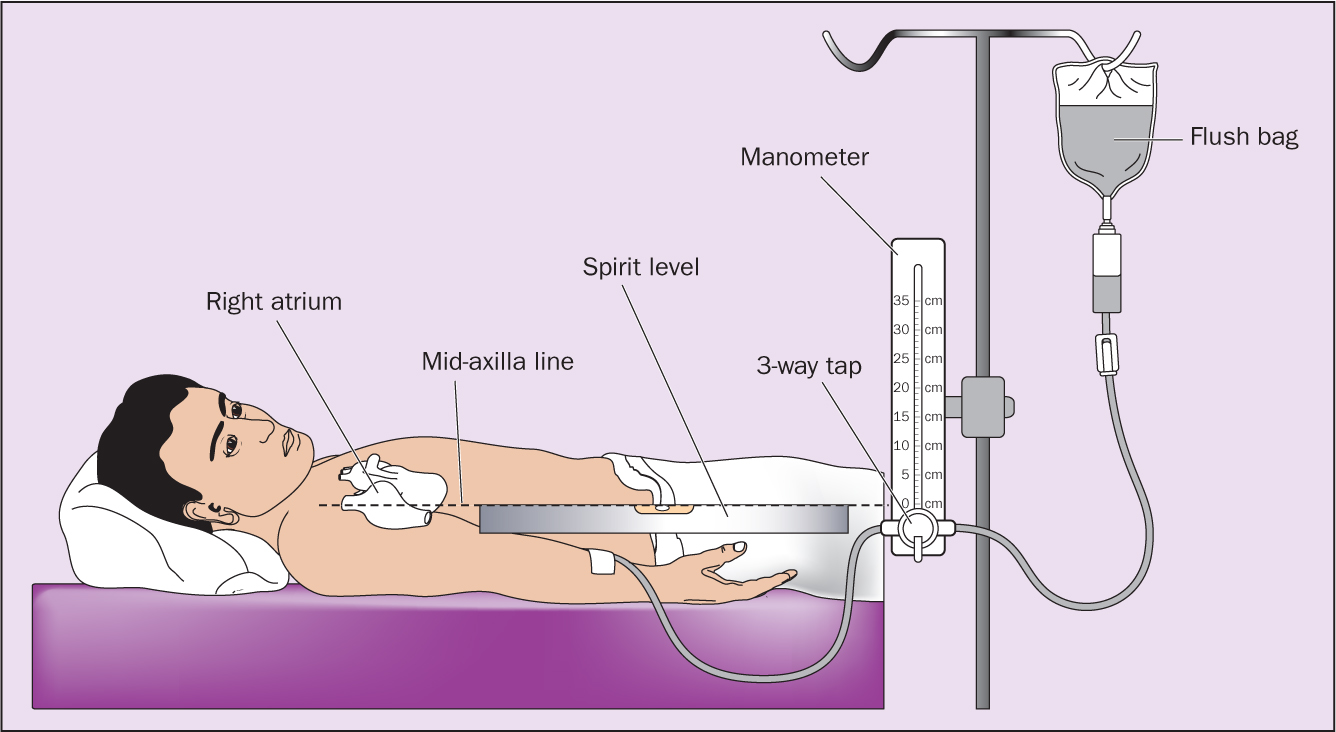
The practitioner should ensure the transducer board is positioned in line with the phlebostatic axis—this is the midaxillary line at the fourth intercostal space, and is commonly known as the midaxillary line (Figure 2). This is approximately at the level of the right atrium and is regarded as the ‘0’ point above which the CVP is measured. A spirit level is often used to ensure this is achieved.
The practitioner should then press the CVP ‘0’ button on the cardiac monitor to calibrate the equipment, thereby ensuring an accurate CVP reading. The CVP must be zeroed on the monitor before and after actions that may affect the reading, such as fluid bolus administration, altered inotrope infusions, changes in mechanical ventilation or bed position, and after repositioning the patient (Hill, 2018).
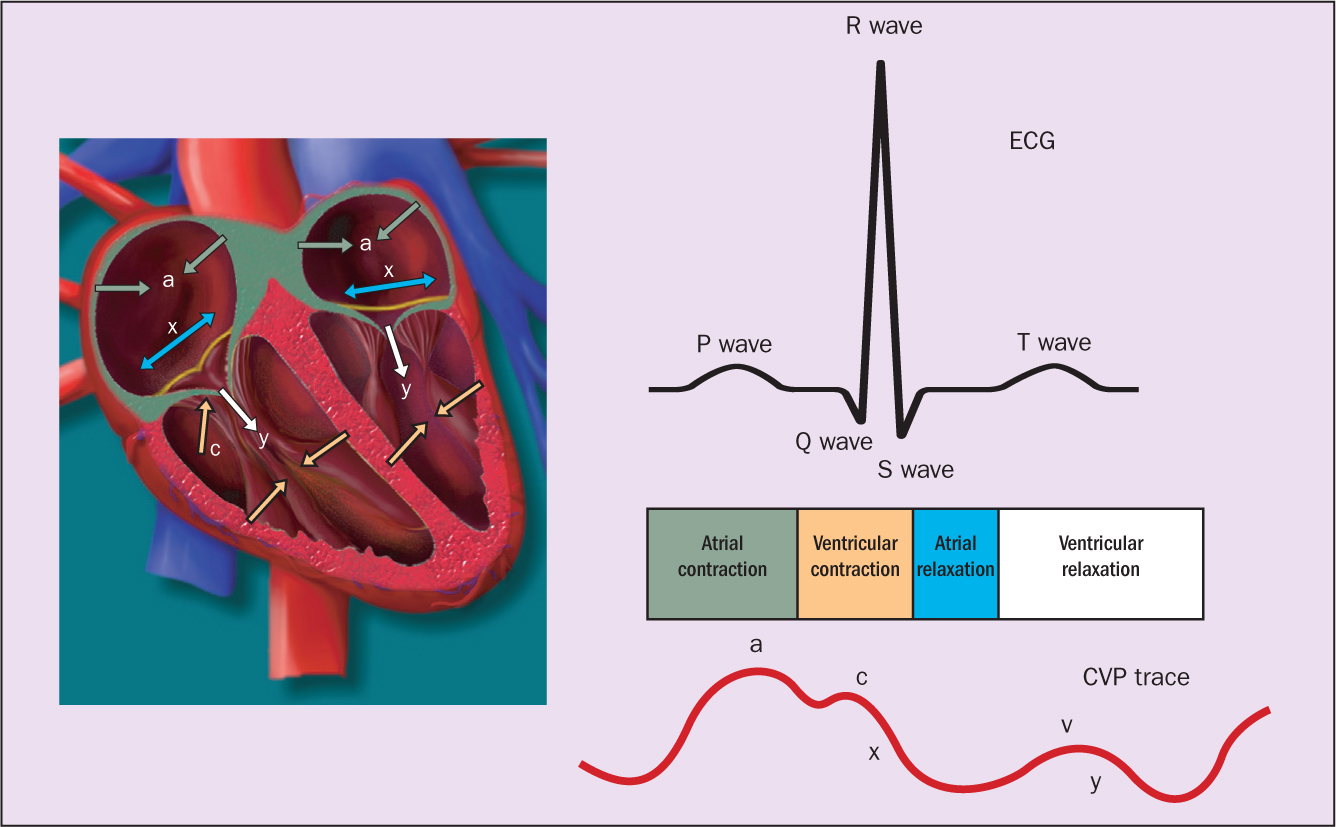
The CVP waveform can be selected and labelled on the patient's cardiac monitor, and a colour code can be applied for ease of identification in line with local policy. The CVC must be free from any kinks or obstructions for it to produce a clear and reliable waveform. Figure 3 shows a normal CVP waveform and its characteristic elements (Lister et al, 2020; Hill, 2018).
The NICE (2016) guidance includes algorithms for IV therapy in adults (available at https://tinyurl.com/hlakdmx). The algorithm for assessment is shown at Figure 1.
The most proximal lumen of the CVC should be designated as the port for the CVP line (Hill, 2018). This port should only be a dedicated CVP transducer line, which is labelled and dated in accordance with local policy and national guidelines (Loveday et al, 2014).
Administering additional fluids to the CVP transducer port will distort the reading. It is advised that the CVC should remain in situ for a maximum of 7 days, unless infection occurs or access is inadequate, in which case the CVC should be changed as soon as possible (Joint Commission, 2013; Loveday et al, 2014). This is to reduce the risks of infection, sepsis and thrombus formation. The transducer line and bag should be changed every 72–96 hours (Loveday et al, 2014) and/or in accordance with local policy and procedures.
Complications
CVP monitoring is an invasive haemodynamic procedure so requires robust compliance with strict asepsis and high-level skills (Gilbert, 2018). Recent findings suggest complications from mechanical complications affect 5–19% of all patients, with 5-26% of those experiencing catheter-associated infections and 2–26% thrombotic complications (Gilbert, 2018).
During catheter insertion, it is recommended that the nurse monitors for mechanical complications such as dysrhythmias, identify patients at risk of pulmonary artery injury (such as rupture) and infarction, as well as implement preventive actions to mitigate the risks of catheter-induced pulmonary artery injury (American Association of Critical Care Nurses (AACCN), 2020).
Nurses' responsibilities
Where possible, nurses involved in CVP monitoring should obtain informed consent from patients for the procedure and provide information about its purpose (NMC, 2018).
Nurses should ensure that the CVC line is secured neatly with tidy infusion lines to prevent accidental line removal. Clear dressings should be placed as required so skin integrity can be observed for visual infusion phlebitis (VIPscore.net, 1999).
Nurses should ensure that up to 300 mmHg pressure is maintained to the transducer pressure bag for it to deliver 3-4ml of 0.9% or 0.45% sodium chloride per hour to maintain patency and an optimised CVP waveform (Hill, 2018).
The CVP waveform (Figure 3) must be observed frequently to identify abnormal trends and, initially, to investigate possible equipment errors (Hill, 2018).
Once the chest X-ray has been examined for line placement and complications, nurses are responsible for the priming, zeroing, levelling and maintenance of the CVP monitoring circuits. Accurate pressure measurement is possible only with the correct preparation of the pressure monitoring system. Errors made during zeroing, levelling and where on the waveform to make the measurement can impede accuracy of the CVP measurement (Hill, 2018). Accuracy can be verified by performing a square waveform test at the beginning of each shift and whenever the system is interrupted (AACCN, 2016). The distal port of a multilumen catheter is used most often for monitoring CVPs in critical care. Other lumens may be used if the quality of the waveform is better.
The transducer is zeroed at each initial setup and the air-fluid interface levelled to the phlebostatic axis. The effect of atmospheric pressure on measured CVP values is eliminated by zeroing the transducer (Urden et al, 2014). The transducer level should be assessed at the beginning of each shift before CVP measurement and patient repositioning. Accurate levelling is vital, as a false reading can result if the transducer is positioned above or below the patient's heart (Shah et al, 2019).
Maintaining a closed system is vital in CVP monitoring so all stopcocks must have a dead-end or a non-vented luer lock cap. Accidental movement of a stopcock without a dead end luer lock cap can result in haemorrhage or an air embolus (Hill, 2018). Alcohol-impregnated sampling port caps should be used on all sampling ports. Using alcohol-impregnated port protectors is effective in decreasing central line-associated bloodstream infections (Martino et al, 2017). Caps with visible blood contamination should be replaced. It is recommended that haemodynamic circuits are changed with each new line or as necessary. Insertion sites must be assessed regularly for signs of infection, bleeding, thrombosis, interstitial placement and catheter migration (AACCN, 2016).
Data suggest that CVP measurements are comparable when the patient is supine with the head of the bed elevated to any angle between 0° and 60°, or when the patient is in a 20°, 30° or 90° lateral position with the head of the bed flat, as long as the reference point is consistent (AACCN, 2016). It may be useful to identify and mark the phlebostatic axis for consistency in measurement. The midaxillary line or the midanteroposterior diameter of the chest is commonly used for patients in a prone position, but not enough evidence is available to validate this (AACCN, 2016).
Conclusion
CVP is widely measured to guide intravenous fluid therapy in critical care. Knowledge and understanding of using CVP monitoring accurately is pivotal to the overall assessment of critically ill patients. The patient's overall haemodynamic status must always be considered.
CVP measurement on its own cannot be used to identify the circulatory status of a critically ill patient, so other haemodynamic monitoring should be integrated into the assessment.
Nurses play a key role in CVP monitoring, including in decreasing central line associated bloodstream infection by reducing risks during insertion, dressing changes and when accessing the invasive device.

