Aseptic Non Touch Technique (ANTT®) was the first, and is still the only, complete clinical practice framework for aseptic technique shared widely in the UK and internationally (Association for Safe Aseptic Practice (ASAP), 2019) (Box 1). Its use provides healthcare organisations and patients with the advantages afforded by a single practice standard for aseptic technique. Such advantages include less practice variability, a common practice language and shared understanding for improved education and research. Developed in the late 1990s (Rowley, 2001), ANTT is now referenced, endorsed and used extensively in many healthcare sectors around the world (Rowley and Clare, 2019). For example, it is used in Ireland (Health Service Executive, 2011), Wales (Welsh Government, 2015), and Australia (National Health and Medical Research Council (NHMRC), 2019). It is also recommended in the USA by the Association for Vascular Access (AVA) (2019).
The widespread adoption of ANTT can be explained by the previous dearth of evidence, and the confusion and myths surrounding aseptic technique. Simply, ANTT filled a void in an area of practice critical to patient safety. Concern about ambiguity of description and practice of aseptic techniques began to be documented during the 1980s (Thomlinson, 1987; Johnson, 1988). Every decade since, multiple authors internationally have researched and reiterated this ambiguity, and there has been variability in the definition of the term ‘aseptic technique’ (Bree-Williams and Waterman, 1996; Gilmour, 2000; Preston, 2005; Rowley et al, 2010). In fact, there are still authors today reporting confusion about this generic term as new findings (Gould et al, 2020).
A review of the literature of the 2000s identified that, because various terminologies for aseptic technique had been used, the term had become ambiguous. Therefore different terms had begun to be used interchangeably. Hybrid techniques evolved ad hoc, creating another layer of ambiguity, particularly in the community setting (Hallett, 2000; Unsworth and Collins, 2011). Authors such as Flores (2008) and Aziz (2009) began to express concern at the impact of this ambiguity on practice standards. The Department of Health (DH) in England demonstrated its concern by setting out standards of aseptic technique across the NHS, within the ‘Saving Lives’ initiative (DH, 2005) and, more explicitly, in the subsequent passing of the Health and Social Care Act 2008 (DH, 2015).
More specialist stakeholder organisations began to recognise these problems, but generally limited improvement to settling upon, and then simply prescribing, the generic term ‘aseptic technique’ in clinical guidance. However, such ‘prescription without description’ often provided no exact details of how aseptic technique should be applied to ensure patient safety, for example, the Healthcare Infection Control Practices Advisory Committee/Centers for Disease Control and Prevention guidelines (O'Grady et al, 2011). This lack of meaningful guidance, together with the decline of traditional aseptic assessments in healthcare training, meant that, up until around 2010, healthcare workers were arguably receiving very little support for this essential competency.
Establishing significant evidence-based change in healthcare is said to take approximately 17 years (Morris et al, 2011) and would appear to reflect the timeline of the ANTT initiative to date. Designed to address the ambiguity and in particular the confused and unhelpful terminology used, such as ‘clean’, ‘aseptic’ and ‘sterile’ techniques, the first author (Rowley, 2001), originated the ANTT Clinical Practice Framework in the late 1990s. ANTT is designed to be used for all clinical procedures from complex surgery to simple clinical procedures and maintenance of invasive medical devices. An updated version of the framework was published in 2010 (Rowley et al, 2010) and a new non-profit clinical organisation, the ASAP, was formed to help support organisations in the adoption and practice of ANTT internationally (http://antt.org/ANTT_Site/about.html). When updating a national clinical guideline for the National Institute for Health and Care Excellence (NICE) in 2012, the National Clinical Guideline Centre defined ANTT as, ‘A specific type of aseptic technique with a unique theory and practice framework’. This definition refers to the original practice concept of ‘Key-Part’ and ‘Key-Site’ protection, that more effectively defines and describes aseptic technique and has laid important foundations for improvement. Key-Parts are the critical parts of the procedure equipment that, if contaminated, are most likely to cause infection. Key-Sites are any portal of entry for micro-oganisms into the body such as open wounds and medical device access sites.
The ASAP's clinical and unbureaucratic structure has facilitated responsive and transparent working with clinical professionals. For the past 12 years, on-site support, including peer-review assessment, national conferences and numerous publications, have helped disseminate ANTT to many different countries. The association developed the ANTT Implementation Programme based upon numerous lessons learned from introducing ANTT into every kind of healthcare provider environment. It was quickly realised that the organisational dynamics of healthcare settings can make or break successful implementation of any new initiative.
ANTT is now being used, translated into many different languages, in more than 25 countries. Different models of adoption have ensued, from voluntary ground-up processes by individual organisations and clinicians, as seen in England and Scotland, to countries that have explicitly mandated or promoted ANTT at government level as a national standard, including Wales and Australia (Welsh Government, 2015; NHMRC, 2019). In addition, large specialist stakeholder organisations have often helped accelerate ANTT adoption in different countries, such as current national initiatives in the USA by organisations with international reach. For example, the Association for Vascular Access (AVA) has issued a position statement explicitly recommending ANTT (AVA, 2019) and the Infusion Nurses Society is integrating ANTT into the forthcoming edition of its Infusion Therapy Standards of Practice.
As would be expected, ANTT is most frequently used in hospital and community care settings. However, it is also widely used in many other care environments such as by emergency services, by military medical personnel, in dentistry and podiatry and, increasingly, by organisations conducting humanitarian work such as Médecins Sans Frontières (MSF). In 2018, the ASAP collaborated with MSF on site visits in South Sudan and Sierra Leone, demonstrating the use of ANTT in even the most challenging of care settings and with limited medical supplies (Treacy-Wong and Davies, 2018).
The ASAP also recognised the important role industry plays in promoting safer aseptic technique through improved product design and supply, and subsequently collaborates, without financial interest, with numerous industry partners to help ensure medical products and devices are effectively integrated with best clinical practice using ANTT.
The critical link between standardised clinical practice and patient safety
In healthcare and other high-volume client-based industries, such as aviation, that are safety critical, educational and practice standardisation is paramount. Quite simply, standardisation reduces variability in understanding and practice, thus increasing quality and safety (Sidiropoulos et al, 2009; Lavelle et al, 2015). Notably, the World Health Organization (WHO) has been committed to improving standardisation in healthcare since 2007, with the ongoing ‘High 5s project’ (WHO, 2013). Perhaps the most well-known example of the advantages of a single standard for a critical clinical competency is cardiopulmonary resuscitation (CPR). Globally, CPR theory, process and practice are essentially the same, based on a shared practice language and a defined set of guidelines and evidence-based recommendations (Perkins et al, 2017; Olasveengen et al, 2017). Related to aseptic technique, was the work by Pronovost et al (2006), who demonstrated that widespread standardisation of intravenous access and maintenance in intensive care settings led to highly significant reductions in healthcare-associated infections.
Standardisation and improvement require a continuous quality assurance framework to both establish and maintain high levels of patient safety. To this end, ASAP produces and freely supplies all the necessary components to support high standards of ANTT practice, including educational competency assessment, audit and evaluation tools. As one part of this multi-modal approach, many NHS organisations have used ANTT Procedure Guidelines (A4 picture-based posters) to help inform and direct best practice for the most common clinical procedures, and many have developed local ANTT Procedure Guidelines for more niche procedures.
Standardising variable aseptic technique with ANTT has been an important milestone in reducing variability and improving practice standards and patient safety. However, it is important to note that, educationally, the ANTT Clinical Practice Framework provides a robust set of principles, practice rules and a simple risk-assessment method that supports practitioners to apply critical thinking to different clinical challenges, including to emergency care scenarios (ASAP, 2020).
Study rationale
In the UK, the Welsh Government mandated ANTT as a national standard in 2015. In England, widespread adoption has been from the ground up on the specific request of practising health professionals, infection prevention leads, chief nurses and chief executive officers. Although an excellent endorsement, this voluntary, rather than mandatory, approach made it difficult to accurately quantify ANTT use. The ASAP wished to gain a complete picture of aseptic technique utilisation, including alternatives to ANTT. Therefore a survey of all NHS trusts in England and NHS boards in Scotland was undertaken in 2019. A Northern Ireland survey is at the planning stage.
Objectives of the study
Methodology
The Freedom of Information (FOI) Act 2000 provides public access to information held by public authorities in England, Wales and Northern Ireland; Scotland is covered by Scotland's own Freedom of Information (Scotland) Act 2002. Public authorities are obliged to publish certain information about their operations and members of the public are entitled to request this information, within certain parameters established by the Act(s).
The FOI survey questions were framed around compliance with the legal requirements for aseptic technique, expected of every NHS trust in England:
The survey also enquired about generally accepted indicators of best practice in clinical governance.
The survey tool aimed to elicit whether NHS trusts in England and NHS boards in Scotland had a single standard aseptic technique and what it was termed; whether staff education, training and competency assessment were provided, whether competency assessment was periodic and whether their standard aseptic technique was stipulated in policy. Finally, trusts and health boards were asked if they used ANTT Clinical Procedure Guidelines.
The survey was sent to FOI officers for recommended completion by the chief nurse or director of infection prevention and control. It was sent to an exhaustive list of NHS trusts in England identified from the NHS Confederation (2017) (N=228), consisting of:
In Scotland, the survey was sent to FOI officers in each of the 16 Scottish NHS health boards responsible for 175 NHS acute and community care hospitals in Scotland.
Results
The main findings are presented in Figures 1–4.
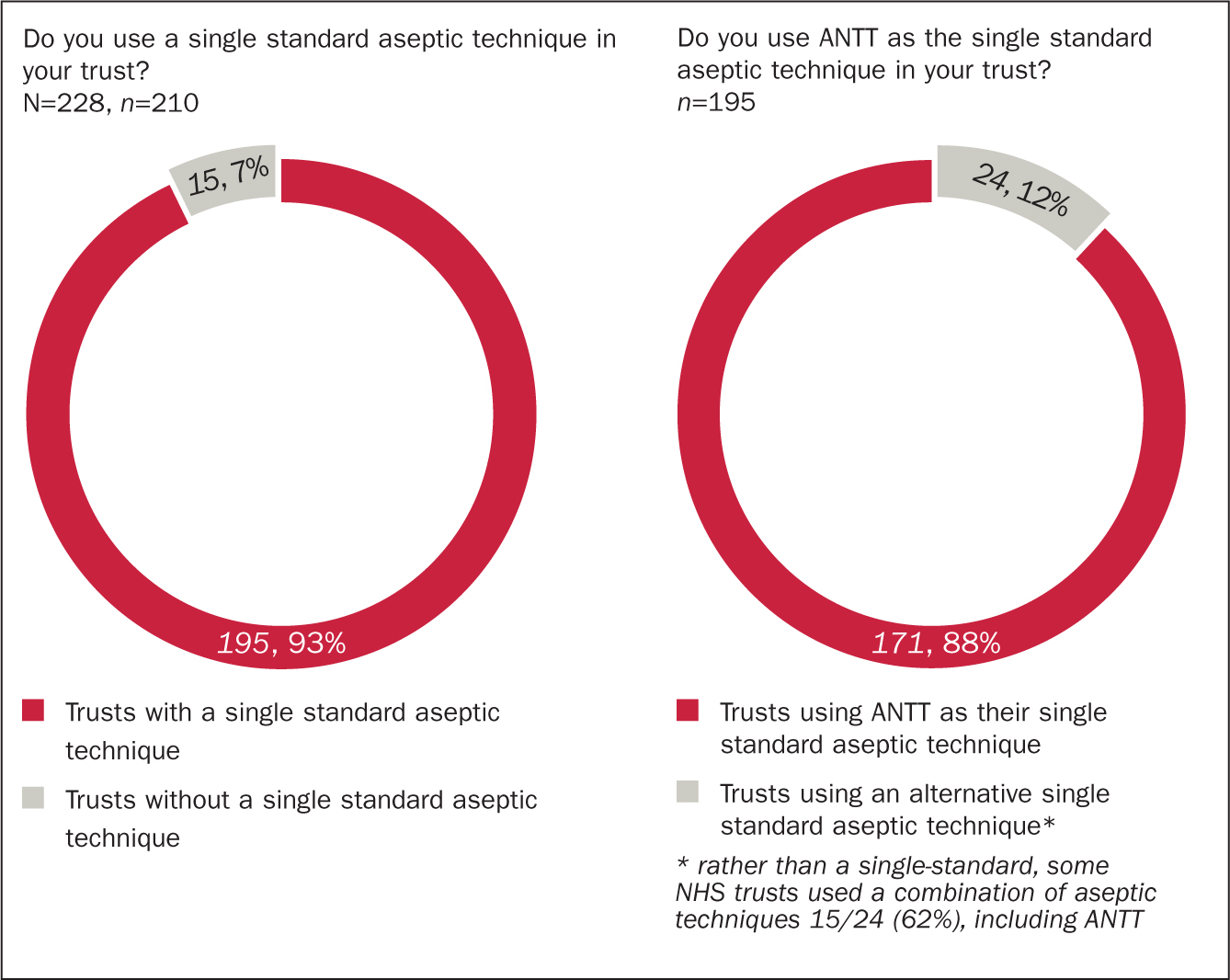
England
A standard technique
Of the 228 eligible NHS trusts in England, 210 (92%) responded to the survey. Of these, 195/210 responders (93%) stated that they had adopted a single-standard approach to aseptic technique, and of those trusts, 171/195 (88%) identified their single standard to be ANTT. The remaining 24 trusts (12%) stated they had an alternative single standard to ANTT. However, of these trusts, 10/24 (42%) stated they used ANTT Clinical Procedure Guidelines and 15/24 (62%) used combinations of different aseptic techniques, including 9/15 (60%) citing ANTT, rather than their stipulated ‘single standard’. The remaining 9/24 (37%) defined their standard generically, as either ‘the aseptic technique’, ‘aseptic technique’ or ‘aseptic procedure(s)’. In total, 158/171 (92%) of English trusts using ANTT as their single standard aseptic technique used ANTT Clinical Practice Guidelines as part of their approach.
Some 15/210 (7%) of trusts said they had no standard aseptic technique at all. These trusts had various combinations of aseptic technique: 4/15 (27%) cited a combination of all the aseptic technique descriptors from the FOI tool (ie aseptic technique, ANTT, sterile technique, clean technique, non-touch technique), 2/15 (13%) described using aseptic technique and clean technique, 2/15 (13%) identified a clean technique only, 3/15 (20%) said they used a combination of aseptic technique and ANTT and 3/15 (20%) said that ANTT was in development in the trust.
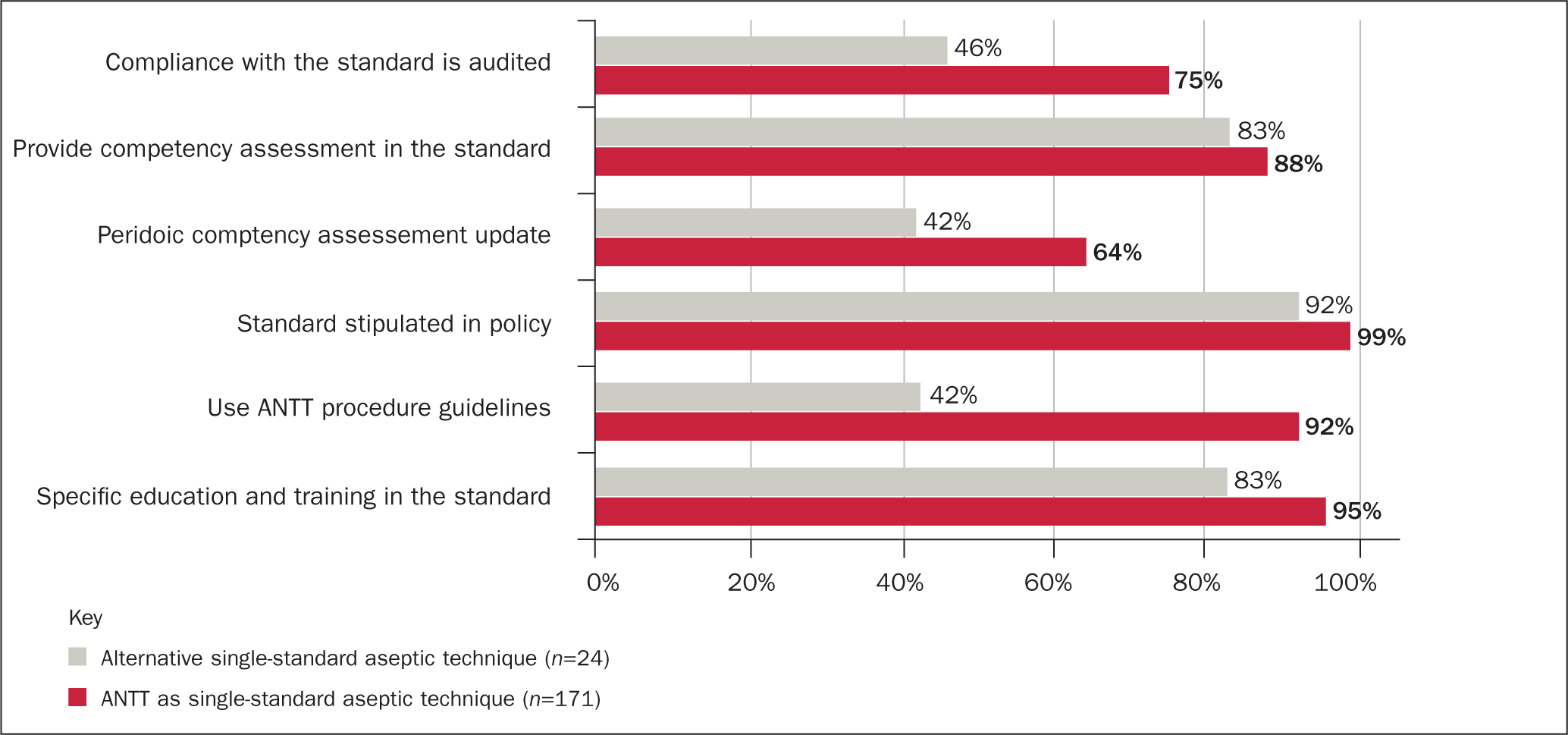
Clinical governance of aseptic technique in England
Indicators for effective clinical governance of aseptic technique were more prevalent in trusts that used ANTT as their single standard aseptic technique (Figure 2).
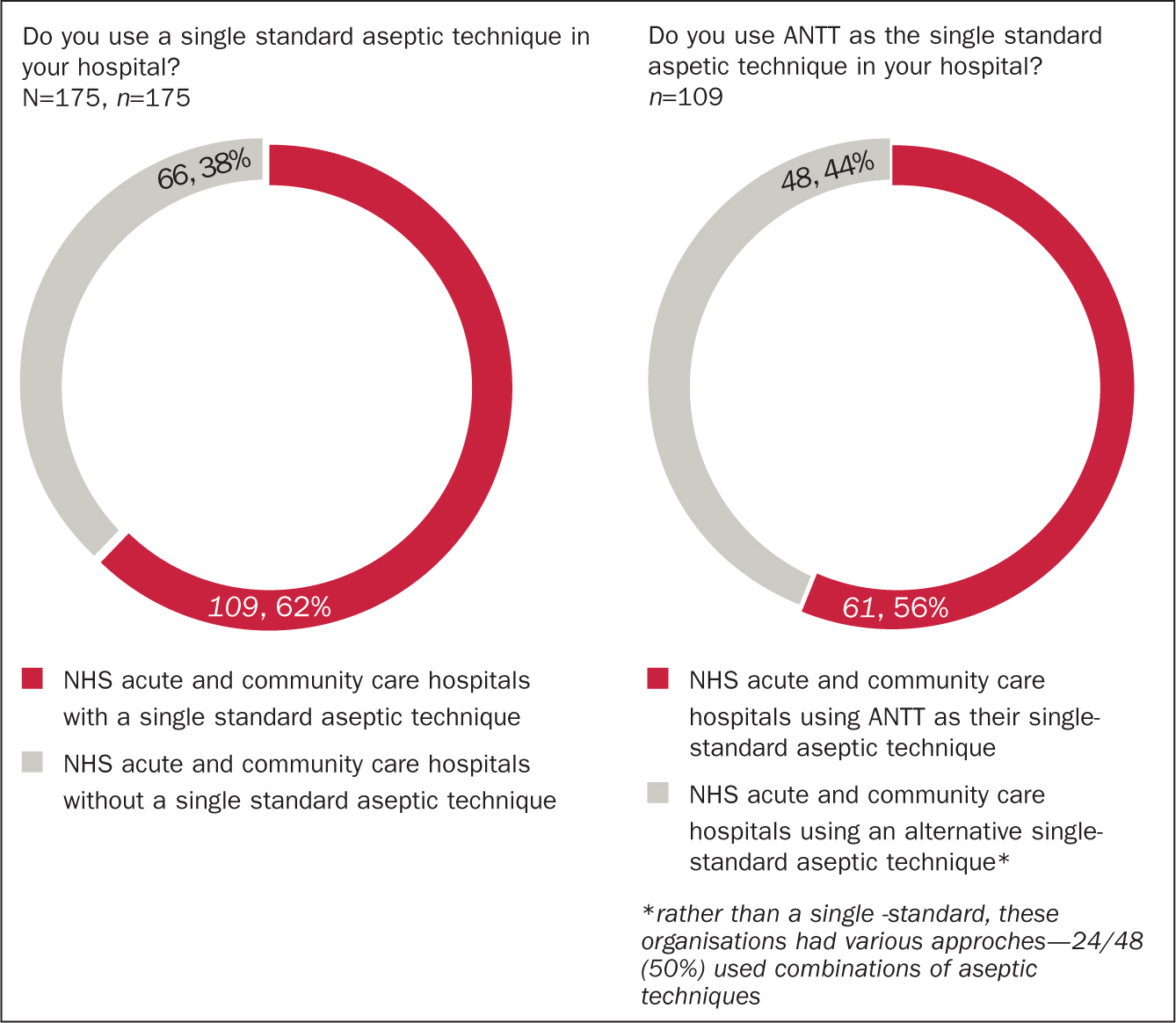
Scotland
A standard technique
In Scotland 16/16 (100%) health boards responded to the FOI survey, representing 175 NHS acute and community care hospitals. Some 109/175 (62%) Scottish NHS acute and community care hospitals reported having a single standard approach to aseptic technique, with 61/109 (56%) of these organisations citing ANTT as that single standard. A further 66 stated that they used ANTT in combination with other techniques, resulting in 127/175 (73%) of NHS acute and community care hospitals in Scotland using ANTT as their single standard or in combination.
Some 48/109 (44%) Scottish organisations said they had an alternative single standard to ANTT. However, similar to English trusts, for 24/48 (50%) this was not a single standard, but a combination of approaches. Some 42/61 (69%) organisations using ANTT as their single standard also used the ANTT Procedure Guidelines.
It seems noteworthy that, in England, where there exists a legal requirement to have a single standard aseptic technique, there is high compliance, with only 7% of trusts outlying. In Scotland where there is no such legal requirement 38% of NHS acute and community care hospitals did not have a single standard.
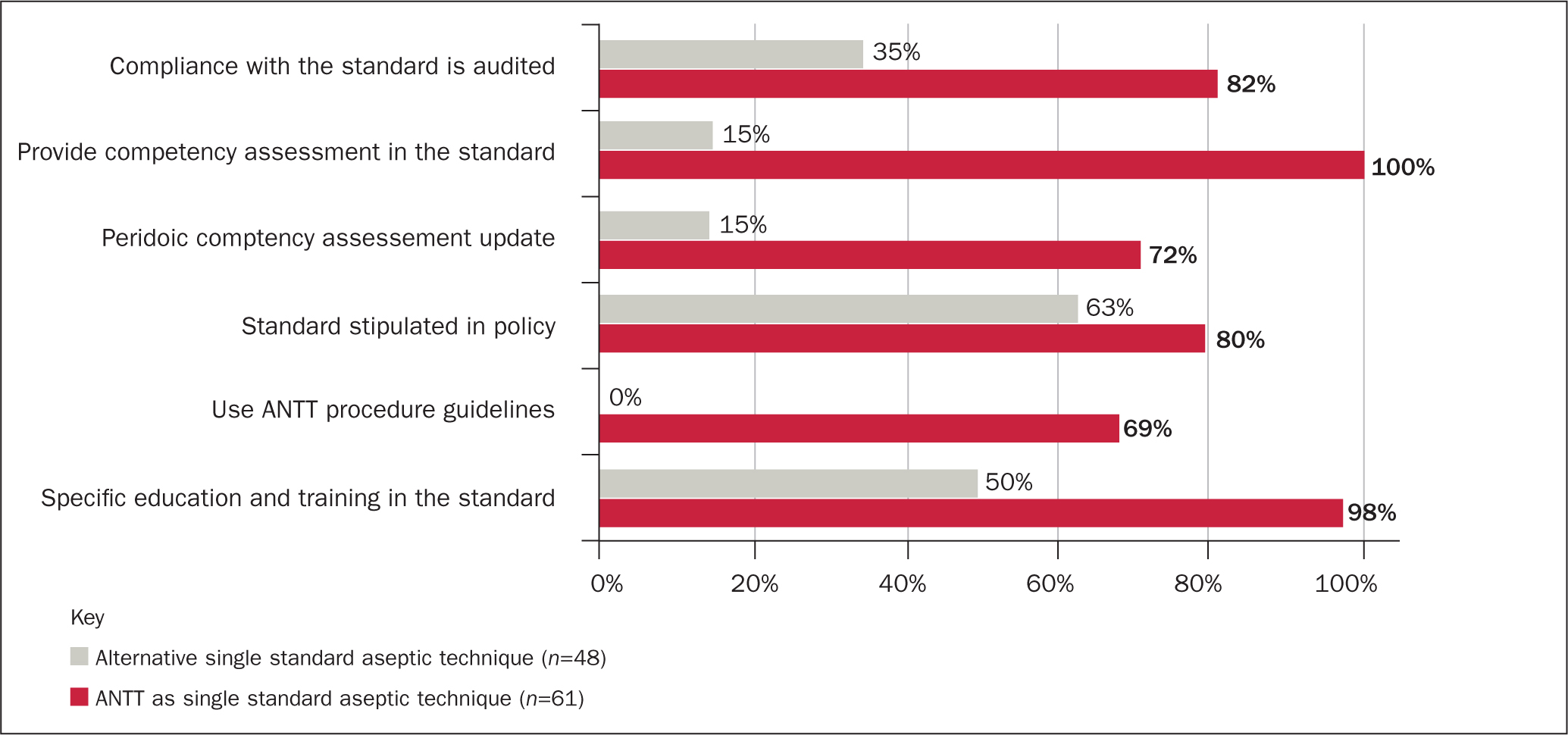
Clinical governance of aseptic technique in Scotland
Similar to England, but even more evident in Scotland, the indicators for effective clinical governance for aseptic technique were more prevalent in hospitals that used ANTT as their single standard aseptic technique (Figure 4).
Discussion
This study provided the first detailed account of the prevalence of aseptic technique type, and indicators for effective clinical governance of aseptic technique in the English trusts and Scottish NHS boards that responded to the survey.
Recognising the clinical risks inherent in the use of variable aseptic techniques, the Health and Social Care Act 2008 legislated for a single standard aseptic technique within all individual healthcare organisations in all sectors.
This study found that in the English NHS trusts that responded, this ambition has been realised, and in fact, surpassed. Rather than using multiple different standards in individual NHS trusts, one single shared standard—ANTT—exists in a large majority of trusts. Similarly, ANTT is used in more than half of NHS acute and community care hospitals in Scotland as a single standard aseptic technique and is used in combination with other standards in nearly three-quarters of all Scottish hospitals.
With ANTT already mandated by the Welsh Government as a single standard in Wales, and recognising widespread ANTT adoption in Northern Ireland (Public Health Agency, 2019), ANTT can be said to be the de facto standard in the UK.
Using ANTT provides a shared practice language, and the clinical governance of education and monitoring of practice standards. NHS trusts that do not use ANTT as a single standard, reported variable combinations of techniques, based upon ambiguous generic terms for aseptic technique that have been well documented as problematic educationally and in practice for decades (Bree-Williams and Waterman, 1996; Gilmour, 2000; Hallett, 2000; Preston, 2005; Flores, 2008; Aziz, 2009; Rowley et al, 2010; Unsworth and Collins, 2011).
Clinical governance
These result show that this is not simply a cosmetic change from the use of generic, ambiguous terms for ‘aseptic technique’ to a specifically defined term of ‘ANTT’. This survey demonstrated the first ever widespread adoption of a single standard for aseptic technique in trusts in England and health boards in Scotland. Most importantly, ANTT is a robustly defined and comprehensive Clinical Practice Framework for education and practice. It not only explains aseptic technique with the novel and now well-tried method of Key-Part and Key-Site protection, it also supports organisations to improve and maintain practice standards through robust clinical governance tools and methods.
To this end, the survey found that the presence of clinical governance indicators for safe aseptic technique, education, training, competency assessment and compliance audit, was appreciably higher in English trusts and Scottish NHS acute and community care hospitals that used ANTT as their single standard technique.
The potential benefits of this was identified in a previous ANTT implementation study of two large NHS hospitals, which identified that the framework, and associated clinical governance components, helped improve health professionals' understanding of aseptic technique, coupled with notable improvements in healthcare-associated infection rates (Clare and Rowley, 2018).
ANTT has helped NHS organisations to improve patient safety, by delivering the clinical governance requirements for aseptic technique required of them in the Health and Social Care Act 2008 in England and more generally in Scotland. In comparison, Scotland's specifically educational and non-mandatory aseptic technique initiative (NES, 2018), has had less impact on promoting associated clinical governance components required to support standards of aseptic technique.
A planned study for Northern Ireland will complete this detailed review of aseptic technique in NHS trusts in the UK. Private healthcare providers were excluded from the survey and take-up of ANTT in this sector is currently being assessed by the ASAP. Similar results are anticipated given collaboration of the ASAP with many of the major private care providers who have undertaken national approaches to ANTT implementation. ANTT is also used in the private community care sector, with Healthcare at Home (HAH), one of the largest independent community care providers in the UK, being the first organisation to achieve Gold level ANTT accreditation status—a peer-review process that evaluates every aspect of ANTT implementation and clinical governance. Head of Clinical Services at HAH, Dawn Genders (2017) said, ‘Using ANTT enabled us to effectively standardise practice nationally and, importantly, monitor our standards effectively.’
Future challenges
The challenge now is to build on this success. Although this survey demonstrated the adoption of ANTT in the majority of English and Scottish hospitals, there is no room for complacency with patient safety at stake. Of course, there will still be instances of practice confusion surrounding generic aseptic technique and no doubt ANTT also. However, the progress afforded by ANTT in providing overdue clarity for education and practice of aseptic technique, is a significant improvement over the previous state of confusion and ambiguity. At the very least, future research enquiry could stop pondering what is meant by the generic term ‘aseptic technique’.
The now clear challenge for healthcare organisations in the UK, and internationally, is to build on this solid foundation for patient safety that widespread use of ANTT has afforded, and pursue the even greater challenge of firmly embedding and sustaining practice understanding and improving ANTT compliance. However, it is important that healthcare organisations fully understand the scale of the challenge and properly invest in it. For perspective, one only needs to consider the historical and ongoing difficulties in establishing compliance with effective hand hygiene. Whereas hand cleaning involves just one, well defined and relatively simple task that has had millions invested globally, compliance is still problematic and considered to be around 50% (Fuller et al, 2011; Kingston et al, 2016; Brühwasser et al, 2016).
In contrast, aseptic technique or ANTT, involves 6-10 steps that require correct integration into every different clinical situation. Therefore, although it is pleasing to see indicators for clinical governance of ANTT in place in so many organisations, it is important that such educational, assessment and monitoring components are not ‘tick-box’ exercises and are robust enough to be effective and maximise patient safety.
ANTT's standard Clinical Practice Framework and common practice language has also allowed more meaningful and generalisable research (Mutalib et al, 2015; Taylor et al, 2017; Simarmatar and Indriani, 2017; Khurana et al, 2018). This foundation can now be built on with larger scale enquiries. For example, the two well defined approaches to practice in ANTT, Standard-ANTT and Surgical-ANTT, facilitate comparative research for specific clinical procedures. ANTT was never intended to be the final solution, but a prerequisite foundation for practice improvement.
Strengths and limitations
The survey was sent to the whole population the authors wanted to investigate, with a near 100% response rate. In England the FOI requests were handled individually by trusts and in Scotland collectively by health boards. There was no response bias, excepting the few centres that chose non-compliance with the legislative instruction of an FOI request. Governance indicators were not collated for the small minority of trusts that declared they had no standard approach.
Conclusion
This study has confirmed ANTT is the single standard aseptic technique in the large majority of NHS trusts in England and a de facto standard in Scotland. Unlike NHS Wales, where ANTT is mandated, NHS adoption in England and Scotland has been notable for its voluntary adoption and user involvement. This is testimony to the void ANTT has filled in this critical area of clinical practice and the commitment and engagement of health professionals to improve patient safety.
ANTT is being used widely internationally and is now established as the first and only global standard for aseptic technique that is commonly shared daily across the boundaries of different hospitals and countries. It provides a standardised approach to aseptic practices and a more meaningful shared practice language across all health sectors, including industry.
In research, it is evident from the literature that authors are using the shared understanding and common practice language of ANTT seen in this study, as a foundation for research enquiry across a range of clinical practices (Mutalib, et al, 2015; Taylor et al, 2017; Khurana et al, 2018; Simarmatar, and Indriani 2017). This survey identified that having a single standard ANTT policy in place has facilitated improvement in the clinical governance of this critical clinical competency and therefore in patient safety.

