Severe bowel dysfunction can present with faecal incontinence, constipation, or both, and can have neurogenic and non-neurogenic aetiologies (Byrne et al, 2019). The prevalence in the population for patients experiencing at least one episode of faecal incontinence a month is high, with up to 12.4% affected (Sharma et al, 2016). The prevalence of severe functional constipation is less well documented, but together these patients present a significant health burden to primary and secondary care. The National Institute for Health and Care Excellence (NICE) published medical technology guidance supporting the use of transanal irrigation (TAI) in patients with bowel dysfunction as it can reduce the severity of constipation/incontinence, improve quality of life, and promote dignity and independence (NICE, 2018; Mekhael et al, 2021).
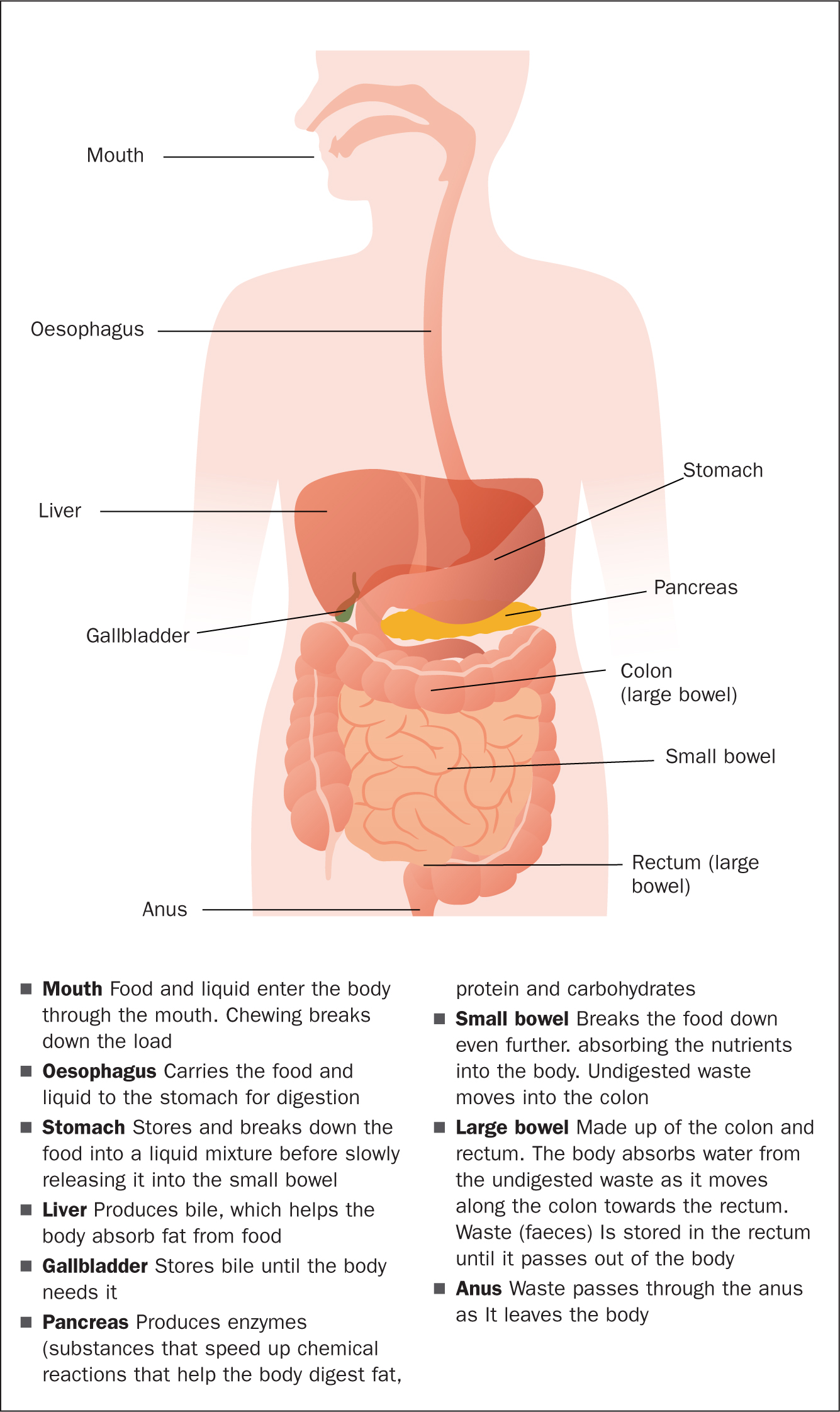
The functioning of the bowel
The bowel is part of the digestive system. It is made up of the small bowel (small intestine) and the large bowel (colon and rectum). The small bowel is longer than the large bowel, but it gets its name from the fact it is much narrower than the large bowel. The digestive system (Figure 1) works by pushing food through the intestines, which usually takes between 24 and 72 hours. Muscular contractions (peristalsis) squeeze the food through the different sections of the intestine. These different sections are separated by bands of muscles, or ileocaecal sphincters, which act as valves. The passage of food from one area of the intestines to another is coordinated so that food stays in a specific area for long enough for the gut to absorb fluids and nutrients, or process and expel waste.
Transanal irrigation
TAI has received increasing attention as a treatment option in patients with bowel dysfunction as it has shown to improve faecal incontinence and chronic constipation (NICE, 2018; Dale et al, 2019). With TAI, water is introduced into the bowel through the anus, facilitating emptying of the rectosigmoid and the left colon. By performing regular irrigations, control of bowel function, including time and place of bowel movements, can be re-gained (Emmanuel, 2019). In patients with faecal incontinence, efficient and controlled emptying of the bowel can be achieved with TAI. This can prevent episodes of incontinence in between irrigations for an average of 2 days. In patients with chronic constipation, regular evacuation of the rectosigmoid with TAI can prevent constipation (Mekhael et al, 2021). The Peristeen TAI system, which is the system discussed in the NICE (2018) medical technology guidance, is an effective treatment option for people suffering from faecal incontinence or chronic constipation. It can help relieve these conditions and offer improved quality of life. TAI is a simple and easy procedure designed to clean a portion of the bowel. It allows patients to take a proactive approach to managing their bowels, consequently giving more control over bowel movements, and preventing faecal incontinence and constipation.
Performing this procedure
It is essential to carry out digital rectal examination before the first irrigation to assess for faecal impaction, anal sphincter dysfunction and co-ordination. Faecal impaction must be treated before starting treatment. If a patient has a previous history of anal, colorectal, or pelvic surgery an endoscopy should be performed to exclude comorbidity.
A rectal catheter with a balloon, or a cone catheter (without balloon) is inserted into the rectum. The balloon is inflated in the rectum and holds the catheter in place while the water is instilled. This initiates the bowel movements (peristalsis), that moves the stool towards the rectum. When the water is instilled and the catheter is removed, the bowel can be emptied. The procedure is carried out on the toilet. It is important to appreciate that a TAI procedure should always be carried out with care. Bowel perforation is an extremely rare but serious complication of TAI and will require immediate admission to hospital, often requiring surgery. Jones et al (2022) identified that in adults, ulcerative disease represents the most common aetiology of bowel perforation, with duodenal ulcers causing 2–3 times the rate of perforation than gastric ulcers. Perforation secondary to diverticular disease represents up to 15% of cases. In those aged 65 and older, perforated appendicitis represents the most common cause of perforation. The overall incidence of perforation from colonoscopy has been reported, on average, around 2% with higher rates during colonoscopy requiring therapeutic interventions. Performing this procedure regularly will empty the bowel effectively, and the bowel will remain empty until the next irrigation. This will allow some choice regarding the right time and place to empty bowels. This offers some people a solution to regain control and the independence to live the life they prefer and without being afraid of having a bowel accident.
Patient education is important to ensure treatment and adjunctive management strategies are sustained—patients need to adhere to diet, fluid intake and co-prescribed laxative regimens. There is a risk of deterioration or exacerbation of symptoms if patients stop alternative management strategies. Realistic expectations must be discussed and agreed with the patient.
Benefits
Regularly irrigating the bowels can significantly improve bowel routine although this requires adjustment to daily routine (NICE, 2018; Mekhael et al, 2021). Patients' experience is individual, therefore it is appropriate for nurses to provide health education regarding when it is time to find new routines that are comfortable and work for the patient. Regular use of TAI has several benefits (Box 1).
Box 1.Benefits of transanal irrigation
- Reduced symptoms of constipation or faecal incontinence for up to 2 days
- Improved quality of life
- Reduced daily time spent on bowel management
- A predictable pattern for emptying bowels
- Freedom to decide where and when to irrigate supporting improved lifestyle
Source: Coloplast Charter, 2022
Contraindications
A consensus review of best practice TAI in adults (Emmanuel et al, 2013) identified the following contraindications to irrigation:
- Anal or rectal stenosis
- Active inflammatory bowel disease
- Acute diverticulitis
- Colorectal cancer (within 3 months of rectal surgery)
- Within 4 weeks of endoscopic polypectomy ischaemic colitis.
Relative contraindications include (Emmanuel et al, 2013):
- Severe diverticulitis, previous diverticulitis or diverticular abscess
- Long-term steroid medication
- Previous rectal surgery
- Radiotherapy to pelvis or surrounding area
- Faecal impaction
- Any bowel conditions that cause pain or discomfort
- Pregnancy (current or planned)
- Anticoagulant therapy
- Severe autonomic dysreflexia.
It is also important to consider patient factors that may cause barriers to use as it can take several weeks for patients to become comfortable with using TAI and some people may choose to stop using it. The patient's ability to self-administer could be an issue and acceptability of using an invasive device. Nurses should take into consideration any history of sexual abuse, patient vulnerability, capacity to consent, and risk or history of self-harm. It may be necessary to risk assess the patient's environment before initiation of treatment.
Patient preference should be a consideration. Some patients might prefer surgery, most often this is a colostomy, ileostomy, or use of anterograde continence enemas (NICE, 2018). It is important to note that the Peristeen TAI system is self-administered so there are limitations in the research on patient-reported outcome measures.
Complications
Bowel perforation is a serious adverse event that has been potentially linked to TAI. It is a rare complication with 1 in 2 million irrigations resulting in perforation (Christensen et al, 2016). Perforation can be caused by three mechanisms: direct impaling trauma, over-inflation of the balloon, or exaggerated hydrostatic pressure during water instillation.
Autonomic dysreflexia is another possible complication in people with spinal cord injuries. This is a syndrome in which there is a sudden onset of excessive high blood pressure. It is characterised by hypertension, sweating, spasms and erythema (most likely in the upper extremities), headaches and blurred vision.
Less serious side effects of irrigation can include abdominal pain, rectal bleeding and nausea. Table 1 covers potential problems and advice for managing these.
Table 1. Troubleshooting
| Problem | Action required |
|---|---|
| Bleeding | A small amount of bleeding can be expected. If the patient experiences copious or regular bleeding this needs to be investigated furtherAny haemorrhage with or without pain indicates a probable perforation and should be treated as a medical emergency |
| Pain | If the patient experiences cramps, discomfort, or pain while instilling the irrigation the procedure should be paused for a few moments. Continue slowly once this has subsided, ensure that the irrigant is at body temperature. If the patient experiences severe/persistent pain stop irrigating as this could indicate a medical emergency |
| Autonomic dysreflexia and autonomic symptoms during irrigation ie, sweating, palpitations and dizziness | It is important to instil the irrigant slowlyIf the symptoms are problematic make sure that the patient is not alone when irrigating until the symptoms are reduced/absentLimit the patient's time on the toilet depending on toleranceIf the patient is at risk of autonomic dysreflexia ensure that medication is available in the home setting. Medicine prescribed for autonomic dysreflexia is usually nifedipine or glyceryl tri-nitrate (GTN) (Spinal Injuries Association, 2017)If autonomic dysreflexia occurs, stop irrigation immediatelyRefer the patient for further assessment before continuing with irrigation |
| Leakage of water around the catheter/cone | Ensure that the catheter is properly locatedCheck water temperature (temperature of water should be lukewarm/body temperature). If the water is cold this can cause abdominal cramps, forcing water out as well as potentially causing pain and discomfortEnsure that the rectum is empty of stoolInflate the balloon more slowly |
| Difficulties in inserting the catheter/cone or instilling irrigant | Carry out a digital rectal examination and remove any stool presentIncrease frequency and/or volume of transanal irrigation to ensure evacuation is adequate |
| Irrigant not expelled | It may be necessary to repeat irrigation if the irrigant is not expelledMake sure that the patient is hydratedAssess for constipation and treat if appropriate |
| No stool evacuated after the procedure | It may be necessary to repeat the irrigation or split into two consecutive episodes waiting 10–15 minutes between each and only using half the irrigant at a time Consider using laxativesAsk the patient the result of the last irrigation. It may be that this was a good outcome, and the procedure needs to be carried out less frequentlyIf there is no stool for several days, it could be caused by constipation or faecal impaction |
| Faecal incontinence between procedures | Increase the volume of water by small increments of aroound 100 ml each time until a satisfactory evacuation is achieved and results in no faecal incontinenceIncrease frequency of irrigationConsider laxatives |
| Leakage of water between irrigations | Ensure that the patient has allowed adequate time on the toilet following the procedureConsider the use of adjunctive measures to encourage emptyingDecrease the amount of water instilledSuggest that the patient uses an anal plug if symptoms persist |
Source: Adapted from Emmanuel et al, 2013; NICE, 2018
Conclusion
TAI is an effective treatment option for people suffering from faecal incontinence or chronic constipation. It can help to relieve conditions and improve quality of life. This is a relatively simple self-administration procedure for patients allowing a proactive approach to managing their bowels, more control over bowel movements and reducing/preventing faecal incontinence and constipation.
KEY POINTS
- Transanal irrigation is a way of facilitating the evacuation of faeces from the bowel by introducing fluid into the colon via the anus in a quantity sufficient to reach beyond the rectum
- It is essential to carry out digital rectal examination before the first irrigation to assess for faecal impaction, anal sphincter dysfunction and co-ordination
- Transanal irrigation can be very effective in helping people diagnosed with chronic constipation to lead a normal life. Being able to control their bowel function often increases confidence with daily living
CPD reflective questions
- While trying to make every contact count, think about the key points you believe are most important to discuss with patients who suffer with constipation and are seeking health advice
- Are you able to discuss the indications and contraindications of transanal irrigation (TAI)?
- Make a list of the benefits and complications of TAI


