Nurses are fundamental in ensuring the delivery of high-quality care in healthcare institutions. Globally, there are an estimated 29 million nurses and midwives (Wong et al, 2015), who constitute the largest group of health professionals within healthcare organisations. However, over the past decades, nursing shortages have become a global challenge. Across the UK, there are around 50 000 nursing vacancies in total: 43 615 in England, 3060 in Scotland, 1612 in Wales and 1671 in Northern Ireland (Royal College of Nursing (RCN), 2020; RCN Northern Ireland, 2020; RCN Wales, 2020).
In 2019, the total number of registrants who left the Nursing and Midwifery (NMC) register was 27 589, which included both UK-trained and non-UK trained nurses, a figure that was 23% higher than in 2013 (RCN, 2020). Such a reduction in nurse numbers inevitably puts patient safety at risk, as well as the quality of the care provided, it also decreases efficiency. In addition, reduced staff numbers affect staff morale, the health of individual nurses, and increase costs for organisations, which have to continually recruit and train new employees to replace those who have left (AbuAlRub et al, 2009; Perreira et al, 2018).
Previous similar reports to the latest RCN workforce review warned of the current and future impending crisis in nursing staff supply, stemming from a lack of adequate workforce planning, workforce strategies and policy initiatives. Nursing retention is influenced by economic, organisational, environmental and personal factors. Identification and quantification of these issues, in order to mitigate their effects, is imperative. Although policymakers are focusing on opening new routes to nursing, actions must also be taken to address the perennial challenges that have, and will, cause nurses to leave their jobs or the profession before they reach retirement age (AbuAlRub et al, 2009).
Consistency in high turnover rates within the nursing profession and associated costs have been documented in the literature (Helm and Bungeroth, 2017). Nurse turnover rates vary across nations: in Jordan it is 36.6% (AbuAlRub et al, 2009), in Canada, 20% (Clancy, 2007), in the UK 17.5% (NHS England and NHS Improvement, 2019), and in the USA 17.1% (NSI Nursing Solutions Inc, 2020). In European countries, the rates range between 12% and 21% (Li and Jones 2013). Several studies in the 1990s argued the benefits of effective nursing management and leadership as having positive influences on nurse retention (Dunham and Klafehn, 1990; McDaniel and Wolf, 1992).
Clinical experience and the literature show that the most common factors that affect retention in nursing have remained relatively unchanged for more than 30 years. According to Health Education England (HEE), the current single biggest workforce challenge is the inability of healthcare institutions to stop nurses leaving their jobs (Mitchell, 2018). Therefore, the purpose of this review was to compile a comprehensive update on the factors that affect the retention of nurses within the ever-changing professional landscape.
Method
The Preferred Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist and flow diagram were used to design and report the review process (Moher et al, 2015) (Figure 1).
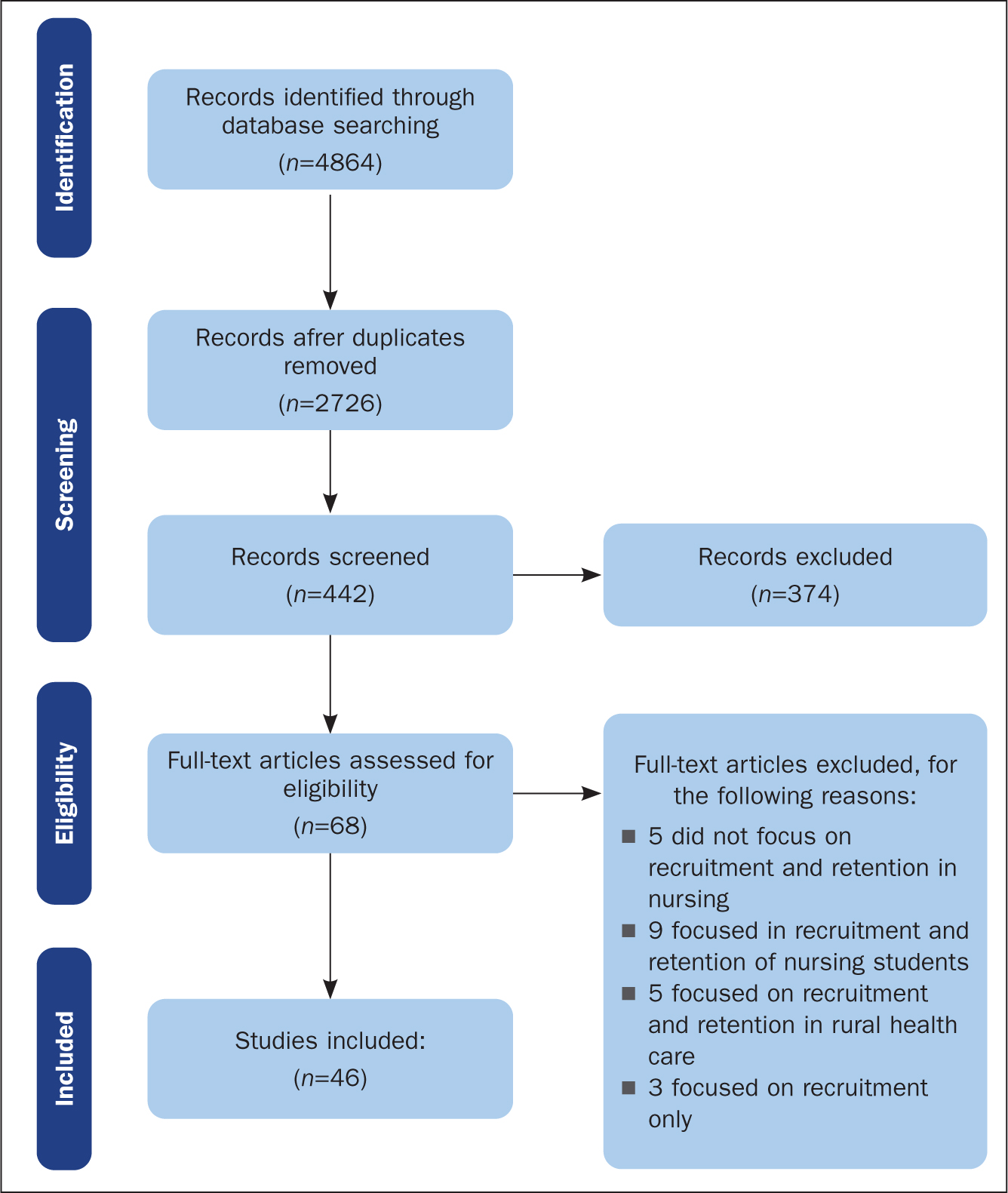 Figure 1. Flow diagram of included and excluded studies
Figure 1. Flow diagram of included and excluded studies
Search strategy
A systematic literature search was performed across five online databases: CINAHL, EMBASE, MEDLINE, and SCOPUS (via Ovid platform), and NICE Evidence Search. The search strategy was tailored to the individual database. A combination of Medical Subject Headings (MeSH) and free-text terms were used to increase sensitivity for identification of potential studies. Search terms used were recruitment* OR retention* OR nurse* and factor* OR influenc*. These terms were initially run individually and then combined in each database. Hand searches were also conducted by searching the reference list in studies identified for inclusion through an electronic record search.
Eligibility criteria
The review was based on peer-reviewed published studies only. All primary research papers considered had primary or clear secondary aims focusing on factors influencing the retention of nurses in hospitals. No limits were applied; all databases were searched up to November 2018. Studies in other languages were considered if an English translation version was available. Reviews, descriptive articles, case studies, letters to the editor and opinions were all excluded.
Study selection
The online search strategy was performed by one of the authors (DA). Selection of potential studies for inclusion both at title and abstract stages was independently implemented by DA and TM in accordance with the eligibility criteria. Neither reviewers were blinded to the study authors and journal titles. Disagreements between the reviewers were resolved by discussions and/or the input of one of the other authors.
Data extraction and methodological quality assessment
Data extraction and quality assessment were performed individually by four reviewers (DA, AC, LG, and LV), with disagreements resolved by discussion and the involvement of a fifth reviewer (TM). Data variables from individual studies included: country of study, participants, sample size and the retention factors identified. All data were entered on a pre-piloted Excel spreadsheet.
The Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group (BAQA) was used to assess the risk of bias of included studies (National Heart Lung and Blood Institute, 2018). The exclusion of studies was not based on the quality assessment score.
Data analysis
Qualitative data analysis through thematic indexing of identified recruitment and retention factors was used. Items were aggregated to provide an overall total number of factors in each thematic group.
Results
The online search strategy retrieved 4864 records. Of these, 2138 duplicates were excluded, leaving 2726 articles, of which 2284 articles were then excluded after screening by title, leaving 442 articles, of which 374 were excluded after screening by abstract, which were assessed for eligibility. Sixty-eight full-text studies were screened, yielding 46 papers and a total sample size of 44 336 participants across the studies eligible for inclusion in this review. No additional studies were identified from hand searching of reference lists of included papers.
Individual study sample sizes ranged from 10 to 16 6707; fewer than 10 had sample sizes of under 20, a similar number had sample sizes of thousands of participants, with the majority (21) having sample sizes in the hundreds.
The included research studies were conducted across 14 countries. Twelve studies were performed in the USA, 12 in Canada, six in Australia, four in the UK, two in Jordan and two in Japan. The following nations, Belgium, Iran, Lebanon, Malawi, Malaysia, Portugal, South Africa and Taiwan contributed one study each.
Methodology quality assessment
All studies included in the review article clearly outlined their objectives, study population and eligibility of participants. Thirty-six articles were cross-sectional surveys and 10 were qualitative; three (Almada et al, 2004; McGillis Hall et al, 2011; Schmiedeknecht et al, 2015) used mixed-methods approaches. All studies were rated as having a moderate risk of bias (25-75%); none had a low risk of bias.
Outcomes
Most studies focused solely on retention factors and four investigated both recruitment and retention factors (Brewer et al, 2006; Bakker et al, 2010; Hart and Warren, 2015; McLemore et al, 2015). The individual items identified as influencing recruitment and retention are presented in Table 1. Items were classified into the following 10 domains:
- Professional factors
- Nursing leadership and management
- Staffing issues
- Education and career advancement aspects
- Organisation and work environment issues
- Support at work
- Personal factors
- Demographic issues
- Financial and monitory aspects
- Unclassified influences.
Table 1. Factors influencing recruitment and retention
| Domain (subthemes) (cited by n studies) | Number of times cited |
|---|---|
| Professional issues (n=22) | Total n=45 |
|
23314911111 |
| Nursing leadership and management (n=22) | Total n=34 |
|
1011351121 |
| Staffing issues (n=11) | Total n=31 |
|
3412192 |
| Education and career advancement opportunities (n=20) | Total n=30 |
|
511113 |
| Organisational/work environment factors (n=16) | Total n=24 |
|
3101241111 |
| Support at work (n=9) | Total n=18 |
|
102321 |
| Personal factors (n=9) | Total n=15 |
|
2221113111 |
| Demographic factors (n=8) | Total n=14 |
|
4712 |
| Financial factors (n=10) | Total n=13 |
|
13 |
| Unclassified influences (n=6) | Total n=6 |
|
111111 |
Major factors identified
Nursing leadership and management
The negative effects of poor management have been highlighted as deleterious features for staff nurse retention. Twenty-two studies highlighted the influence of nursing leadership and management on staffing levels within healthcare organisations. Lack of support from managers, and staff feeling not valued (not recognised), followed by a negative management or leadership style were the most common issues that had a negative effect on nursing turnover. Bugajski and colleagues (2017) reported that of 279 nurses who responded to their survey, more than 96% stated that competent management and management that supported nurses were both very important factors. Nurses demonstrated dissatisfaction with a perceived lack of communication about implemented organisational changes, and they experienced a sense of powerlessness when major changes took place without their invited input (Leurer et al, 2007). This is supported by Valizadeh et al (2018), who observed that nurses:
‘Stated that lack of support by managers and head nurse caused feelings of emptiness, worthlessness and discouragement.’
Nurses also emphasised the significance of nurse leadership, rather than management, as being the pre-eminent factor to engage nurses and other staff in the creation of a supportive culture for quality improvement to enhance staff retention (Draper et al, 2008). Transformational leadership was seen to promote organisational fairness, affective commitment, and high-quality care, in contrast to abusive leadership, which was characterised by finding fault with staff, perpetuating a blame culture, and a culture of inaccessible leaders and incivility (Lavoie-Tremblay et al, 2016; Van Osch et al, 2018).
Education and career advancement opportunities
Professional development and promotional opportunity aspects were reported in 20 studies. Takase et al (2016) demonstrated that the availability of advancement opportunities had a negative correlation with nursing turnover. In their study of 766 nurses, Takase and colleagues reported that the lack of opportunities for promotion/professional development were cited as reasons by at least 39% of respondents to the survey. In a focus group of 56 nurses (Brewer et al, 2006), the lack of professional development opportunities was highlighted by many as a challenge for staff retention. Participants acknowledged that opportunities for continuing education—professional and academic—would encourage the recruitment and retention of staff.
Furthermore, participants stated that staff shortages, coupled with inflexible rota allocations, inevitably prevented nurses from leaving the workplace to attend lectures. Within the current economic climate, financial resources have also been identified as a strong limitation for some staff because employers do not usually pay for continuing education (Brewer et al, 2006).
Organisational factors
Many studies highlighted dimensions of the work environment as barriers to recruitment and retention:
- Work climate/culture
- A lack of teamwork and/or multidisciplinary collaboration
- Poor working conditions
- Availability of resources (including equipment, staff and infrastructure)
- Lack of staff empowerment
- Failure to promote/implement zero tolerance policies towards violence against staff.
A total of 24 organisational factors were reported in 16 studies. Healthcare environments that advocated a greater voice for nurses in decision-making, both at organisational and clinical levels to influence patient outcomes, had low turnover rates compared with those where staff were frustrated and disillusioned due to a lack of empowerment (Brewer et al, 2006). Constant threats (and physical or emotional abuse) within an already stressful environment had a negative effect on nurses' job satisfaction and morale. One of the studies (Barron et al, 2007) found that staff who experienced verbal abuse were 40% more likely to leave their current employer and 28% more likely to leave the nursing profession altogether.
Staffing levels and professional factors
Concerns about staffing levels were raised in 11 studies and included low staffing levels, high patient-to-nurse ratios, staff shortages, and the lack of opportunity to take breaks or time off. These factors were found to affect both the individual nurse and the healthcare organisation overall. The theme of staffing levels was closely linked to the professional factors identified in the studies, which included:
- Staff experiencing low job satisfaction
- High workload
- Emotional exhaustion
- High job pressure and demands
- Work-related stress and frustration from being unable to perform professional duties to the best of their abilities.
Professional issues were reported in 22 studies. High volumes of sick patients and long hours made it difficult for nurses to practise safely, with the consequence that this affected the retention of experienced nurses. For organisations, staff shortages threaten service capability, the quality of care, and lead to inadequate and inequitable access to professional development (Newman et al, 2002).
‘Nurses who reported that they intend to leave their current positions were significantly more likely to have jobs with greater physical and psychological demands, longer hours, less autonomy and lower supervision and peer support.’
Other factors
The lack of peer support and lack of allied health professional support was another retention concern, which was identified in nine studies. Individual personal factors, such as health issues and family matters, were also reported in nine studies; demographic status (age, retirement, generational differences among staff, gender and work experience) were identified as influencing factors in eight studies and working terms and conditions, including unsatisfactory salaries, were recorded in 10 studies.
Discussion
This study provides an up-to-date overview of the evidence on barriers to the retention of nurses in hospital settings, which include: poor nursing leadership and management, lack of educational opportunities and career progression, the organisational culture and environment, working terms and conditions, demographic and personal challenges. The themes observed in this review are recurrent and universal, and have been a familiar refrain for decades in this long-standing nursing shortage paradigm. Therefore, there is an urgent need to develop and implement strategic policy and clinical practice responses to the issue in order to:
- Address the multifactorial consequences of the many challenges identified
- Undertake an overall review and impact assessment of the strategies implemented previously to address the ongoing challenges.
The main factors outlined in this study are strongly influenced by the workplace culture within each individual healthcare organisation. The literature reports that organisational culture influences the workplace atmosphere, which influences nurses' decision as to whether to stay in or leave their job (Hutchinson et al, 2008). Traditional and current nursing leadership and management structures are heavily hierarchical and this cultural phenomenon affects the values, beliefs and behavioural patterns of the nurses working within the organisation. Supportive organisational cultures are key to the recruitment and retention of staff (Kleinman, 2004, Leurer et al, 2007, Draper et al, 2008).
In some cases, due to poor leadership and lack of support, nurses reported experiencing workplace bullying, leading to a higher risk of burnout consequent to the stress imposed on staff by the organisational environment (Unruh and Zhang 2013; Han et al, 2015; Valizadeh et al, 2018). The events that occurred at Mid Staffordshire Hospital, where 400-1200 potentially avoidable patient deaths occurred due to poor management and poor care over a 4-year period, are typical of a poor organisational culture (Francis, 2013). The hospital had an insidious culture of fear, bullying, a culture that tolerated poor standards, and that strongly discouraged whistleblowing, all of which prevented staff from doing their jobs to the best of their abilities and encouraged a culture of secrecy, with management ignoring the concerns of both staff and patients (Francis, 2013). Key issues highlighted by the Frances inquiry included high staff turnover and the use of agency or temporary staff. The events at Mid Staffordshire illustrate why, for example, leadership and management issues, and the hospital environment, can affect the recruitment and retention of staff. These concerns were already being highlighted 20 years ago (Dunham and Klafehn, 1990) and are the same issues that have been identified more recently (Buffington et al, 2012; Unruh and Zhang, 2013; Han et al, 2015).
Lack of staff empowerment and a lack of support for staff weakens nurses' commitment to the organisation and reduces job satisfaction. This results in major work-based problems, such as loss of confidence, staff experiencing mental health issues and depression, ultimately leading to reduced productivity, and increased staff turnover (Spence Laschinger et al, 2009). Such issues can lead to physical, mental and emotional exhaustion due to these constant work pressures. Nurses who experience burnout lose the motivation to work (Ramoo et al, 2013), which not only results in reducing the quality of services provided, but also causes nurses to be indifferent to their patients, which again leads to high nurse turnover.
A focus on patient satisfaction through the delivery of high quality care and service improvement is important, but emphasis must also be placed on the management of human resources through modification of organisational culture as a strategy to attract and retain staff. A hospital working environment that empowers and motivates nurses is a necessity for rejuvenating and sustaining the nursing workforce, which is evidenced by Magnet-accredited and Pathway to Excellence Program-accredited hospitals. The Magnet-accreditation program and the Pathway to Excellence accreditation program are overseen by the American Nurses Credentialing Center and promote the contribution of frontline nurses in influencing the practice environment and, ultimately, enhancing patient outcomes (Arthurs et al, 2018). These initiatives enhance and promote interprofessional cooperation, ensure that staff contributions are acknowledged and that there is communication with nurses at all levels, involving them in the decision-making process. These are some of the main ways that can help reduce staff turnover. Therefore, it is important for nursing managers to create channels through which staff can communicate easily with one another. One example of this would be the introduction of ward-or team-shared governance committees aimed at addressing local clinical area concerns, as has been done at Nottingham University Hospitals NHS Trust, where some of the authors work.
The development of new knowledge through research and innovation, such as the clinical academic career pathway for nurses, enhances career development pathways and is one of the ways to attract and retain nursing talent. This is confirmed in a study showing that the desire to establish a fulfilling career was the second most commonly reported reason that nurses wanted to leave the profession (Philippou, 2015), with the need for better remuneration being the main reason. This reinforces the importance of focusing on nurses' career development as a staffing retention strategy.
Nurses who participated in the research reported in the studies reviewed in this article described their struggles to deliver the care that patients deserved in the context of wider nursing, professional and staffing issues. Across the UK, the safe staffing agenda takes high priority. A policy report by the RCN (Helm and Bungeroth, 2017) found that 76% of nurse leaders had concerns about ensuring safe staffing levels, with 90% expressing concern about the recruitment of new staff and 84% with the retention of existing staff (Helm and Bungeroth, 2017). Current discourse calling for urgent action to resolve the challenges facing the nursing profession highlights that staff burnout, low morale and low job satisfaction are prevalent and on the rise. Nursing as a profession is at risk of becoming an unattractive career option and this would seem to be reflected in the drop in the number of preregistration nursing applicants to universities prior to 2018 (Beech at al, 2019). However, in the face of the current COVID-19 global pandemic, UK universities received an overall 8.5% increase in nursing applications compared with previous application cycles (Universities and Colleges Admissions Service, 2021). Box 1 outlines practical examples of the retention strategies employed at one NHS trust in England.
Box 1.Recruitment and retention strategies applied at Nottingham University Hospitals NHS Trust
- Identify factors that affect recruitment and retention at local hospital level
- Prioritise the implementation of key national workforce strategies (public policies), for example, detailed workforce measures from national documents such as the Interim NHS People Plan (NHS England and NHS Improvement, 2019)
- Identify other strategies that have been shown to positively change retention and recruitment: for example:
- Developing and implementing staff empowerment and autonomy strategies (shared governance councils) at ward, divisional and other staff group levels. This empowers staff to deal with and address local ward priorities to improve staff and patient care outcomes
- Recruiting and sponsoring international nurses
- introducing return to practice and return to work after retirement programmes
- Evaluate implemented projects to identify and quantify their impact, consider any further improvements required and disseminate good practice. For example, the Chief Nurse Excellence in Care Junior Fellowship initiative has been evaluated and published demonstrating a successful impact on professional development as a recruitment and retention tool (Bramley et al, 2018)
- Gaining international nursing recognition for world class care; American Nurses Credentialing Center (ANCC) Magnet accreditation and Pathway to Excellence accreditation
Study strengths and limitations
The authors conducted a comprehensive search strategy with strict adherence to PRISM guidelines (Moher et al, 2015). The search strategy, data extraction and quality assessment were all performed independently by the authors and consensus on the findings was reached among the team. However, the review focused on retention factors for hospital nurses only, limiting the generalisability of findings to nurses working in other healthcare settings. The authors noted that there was a limited number of studies from developing countries and rural hospital settings.
Conclusion
Globally, healthcare institutions are striving to address nursing shortages, a problem that has been heightened by the COVID-19 epidemic. Many of the identified factors that affect staff turnover require immediate evidence-based co-operative strategies between both employees and employers.
Nursing shortages inevitably have a direct impact on patient safety and the quality of care, and the factors outlined in this review place great emphasis on the need for hospitals and policymakers to develop and implement better targeted and relevant initiatives to address staff shortfalls. Although there is an acknowledgement of the limited availability of some critical resources such as finances, participants indicated that efforts to improve organisational culture and the work environment would foster greater collaborative relations among nurses, and with managers and other health professionals, which, in turn, would help increase their commitment to their jobs. Given current workforce shortages, this review further highlights the need for continuous evaluation of the strategies employed in healthcare organisations to address factors that pose barriers to the recruitment and retention of nurses.
KEY POINTS
- Nursing shortages inevitably have a direct impact on patient safety and the quality of care delivered
- Turnover factors observed across studies have not changed over time
- There is an urgent requirement to develop and implement strategic policy and clinical practice responses to address high nurse turnover rates
CPD reflective questions
- What can you do to reduce staff turnover in your clinical setting?
- Does your healthcare organisation have nurse retention strategies? If so, can you identify and outline your individual responsibility and your organisation's responsibility to ensure these can succeed?
- Identify current national policies to address nursing staff shortage and reflect on how these policies influence your daily practice
- Consider the themes highlighted in this review and how they affect patient safety

