There is increasing evidence to support the importance of the preservation of muscle mass as we age (Deutz et al, 2014). Disease, inactivity and poor nutrition can all contribute to loss of muscle mass and function, known as sarcopenia, which is more common in older age, although it can occur in earlier life (Cruz-Jentoft and Sayer, 2019).
Sarcopenia is a disease characterised by progressive and generalised loss of skeletal muscle mass and function, resulting in reduced physical performance that can contribute to frailty, prolonged physical disability, increased risk of falls and overall poorer quality of life (Anker et al, 2016; Cruz-Jentoft and Sayer 2019; Cruz-Jentoft et al, 2019). Malnutrition is described as a state of nutrition in which deficiency or excess (or imbalance) of energy, protein and other nutrients causes measurable adverse effects on the tissue/body form (body shape, size and composition), function and clinical outcome (Elia, 2003).
Malnutrition and sarcopenia are often present simultaneously, particularly in the older population. Age-associated muscle loss is common in older adults because muscle mass declines by 30-50% between the ages of 40 and 80 years (Patel et al, 2013). Ageing also stimulates infiltration of fat into muscle, which impairs new muscle growth (Batsis and Villareal, 2018). In addition, older adults have reduced muscle perfusion (Moro et al, 2019) and reduced digestive capacity; weight loss in this group carries the risk of loss of lean body mass (Phillips and Martinson, 2019).
Hormonal changes that occur as we age can also have an effect on fat-free mass. In women, menopause is associated with increased body weight and fat mass, especially around the centre of the body (increasing waist circumference) and decreased fat-free mass (Batsis and Villareal, 2018), and in men there is a reduction in testosterone of about 1% a year, leading to reduced muscle mass (Batsis and Villareal, 2018).
Malnutrition is a key cause of sarcopenia. This can either occur through undernutrition—when not enough calories or protein are consumed each day to sustain muscle mass—or through over-nutrition, where obesity promotes low-grade inflammation, in turn leading to insulin resistance, which promotes further gain in fat mass and loss of muscle mass, leading to sarcopenic obesity.
Both malnutrition and sarcopenia result in negative outcomes for patients and the healthcare system. From the patient perspective, the consequences include decreased quality of life (Vandewoude et al, 2012), delayed recovery from surgery or injury (Kenny et al, 2017), an impaired response to treatment (Bozzetti, 2017), and reduced functional capacity (Byun et al, 2017; Springer et al, 2017), in addition to contributing to a more rapid deterioration in pre-existing conditions (Byun et al, 2017; Springer et al, 2017; Landi et al, 2017). Figure 1 outlines some of the consequences of muscle mass loss on the functioning of the human body. These consequences have a knock-on effect on healthcare costs, hospitalisation rates, morbidity and mortality (Vandewoude et al, 2012).
Figure 1. Some of the consequences resulting from loss of muscle mass (Holdoway and Ashworth, 2021)
Being overweight or obese can mask sarcopenia and malnutrition. The prevalence of ‘sarcopenic obesity’—or obesity in combination with sarcopenia—is increasing in adults aged 65 years and over (Batsis and Villareal, 2018). Although in malnourished patients the presence of sarcopenia may be visually apparent, it is not always easy to identify sarcopenia in overweight or obese patients. Care needs to be taken that too much focus is not placed on treating the obesity and failing to identify sarcopenia because this could lead to adverse outcomes (Cruz-Jentoft and Sayer, 2019).
The COVID-19 pandemic has undoubtedly further emphasised the impact of low muscle mass and muscle loss in impeding recovery. The combination of reduced activity, or bed rest, caused by fatigue, poor appetite and reduced food intake, with loss of taste and smell, frequently results in weight loss. This happens particularly among older people and those with chronic conditions, and muscle is often lost at a disproportionate rate to fat mass. The nutritional consequences of COVID-19 are not yet fully understood, but knowledge gained from acute respiratory distress syndrome suggests that patients are likely to experience skeletal muscle dysfunction, which can persist for between weeks and years (Files et al, 2015). Initial research has found a high incidence of weight loss and risk of malnutrition among COVID-19 survivors—independent of hospitalisation (Di Filippo et al, 2021)—and sarcopenia, loss of muscle mass and function have been found to occur in survivors of COVID-19; older adults and the most critically unwell patients have been found to be at greatest risk (Welch et al, 2020).
Loss of muscle mass and strength can, however, be treated through nutritional intervention, including ensuring the patient has a protein-rich diet, together with resistance-type exercise or activity (Wu et al, 2021), which makes early identification of sarcopenia all the more important.
Prevalence
Depending on the definition used, sarcopenia affects 4–25% of older, independently living adults in the UK: the prevalence data vary according to the identifying tests used for sarcopenia, as well as a patient's underlying diagnosis (Patel et al, 2013; Dodds et al, 2020; Kilgour et al, 2020). Evidence suggests that incidence increases with age, so older adults are particularly at risk, especially those with conditions that limit their activity or lead to enforced periods of bed rest (Cruz-Jentoft and Sayer, 2019). There is evidence indicating that patients with malnutrition have about three to four times the risk of developing sarcopenia as those who do not (Batsis et al, 2013; Beaudart et al, 2019).
With the growth in the older population worldwide, the number of those with sarcopenia will inevitably also rise, making this issue an increasingly important public health concern.
Identification of the conditions
Malnutrition
Malnutrition can be identified by using a validated screening tool such as the Malnutrition Universal Screening Tool (MUST) (Elia, 2003). This combines measures including body mass index, recent unplanned weight loss and presence of acute illness. Table 1 provides a list of screening tools and where to access them.
Table 1. Tools and resources
| Managing Adult Malnutrition pathway resources, https://www.malnutritionpathway.co.uk | |
|---|---|
|
https://bit.ly/3ndmPCE |
|
https://bit.ly/3hgWrEa |
|
https://bit.ly/3E1ub1Z |
|
https://bit.ly/3nf3PDE https://bit.ly/2X5tLGJ |
|
https://bit.ly/2VxxVqM |
| MUST [Malnutrition Universal Screening Tool] calculator | https://bit.ly/2X5uUOx |
| SARC-F questionnaire * SARC-F is included as part of a Rapid Geriatric Assessment from Saint Louis University, USA | https://bit.ly/3kLjvwk |
| Chartered Society of Physiotherapy | |
| Advice for specific conditions | https://bit.ly/3yEmsnL |
| UK Chief Medical Officers (joint advice) | |
|
https://bit.ly/3xo1MzZ |
|
https://bit.ly/3tP6Nzg |
| Physical performance test instructions | |
|
https://bit.ly/2SvgXXW |
|
https://sforce.co/3z96fpQ |
| Further information may also be available from your local dietetic, physiotherapy or occupational therapy department | |
SARC-F =Strength, Assistance with walking, Rise from a chair, Climb stairs and Falls
Screening should take place when there is clinical concern (Box 1), eg opportunistically, such as on first contact within a new care setting or at an outpatient appointment (National Institute for Health and Care Excellence (NICE), 2012; 2017), on contact with a community/district nurse, during a medicine use review, at annual disease reviews, pre-operatively and at specialist clinics for at-risk groups (eg those with long-term conditions).
Box 1.Areas of clinical concern where malnutrition should be considered in a patient
- Unplanned weight loss
- Loose-fitting clothes
- Appearing thin
- Fragile skin
- Apathy
- Poor wound healing
- Pressure ulcers
- Muscle wasting (sarcopenia)
- Reduced physical function
- Difficulty swallowing
- Frequent falls
- Prolonged intercurrent illness
- Recurrent infections
- Poor appetite
- Altered taste sensation
- Altered bowel habit or gut function
- During and after cancer treatment
- Chronic condition or surgery
- Deteriorating medical conditions
- Side-effects due to medication
Sarcopenia
In the acute setting and specialist units, skeletal muscle mass can be assessed through body composition techniques such as CT scans, DEXA scans and bio-impedance (Cruz-Jentoft et al, 2010). However, these methods are unlikely to be available in community settings, where a more pragmatic approach is required, and where the SARC-F questionnaire (where SARC-F stands for Strength, Assistance With Walking, Rise From A Chair, Climb Stairs and Falls) is commonly used (Table 1) (Malmstrom and Morley, 2013). This is a 5-item questionnaire that helps determine the likelihood of sarcopenia. A score equal to or greater than 4 would suggest the likelihood of sarcopenia, which then be followed by simple strength measurements, such as the sit-to-stand test and hand-grip strength. Grip strength can be used as a simple method of predicting muscle function and sarcopenia, which may significantly affect severity and mortality in COVID-19 (Kara et al, 2021).
Several tests can be done to assess a patient's physical performance (Table 1), including gait speed, timed up and go test and the 4 m corridor walk (Cruz-Jentoft et al, 2019).
Managing malnutrition in sarcopenia
If sarcopenia and risk of malnutrition have been identified, patients can be managed pragmatically, using the management strategies detailed below. A multidisciplinary approach may be required to support identification and appropriate management. The cornerstone of management will involve good nutritional care together with exercise. Management of malnutrition should follow existing guidance (NICE, 2021) and can be linked to the malnutrition risk category (low, medium or high risk). The following steps should be followed:
- Identify and record risk of malnutrition and sarcopenia as described above. Figure 2 outlines the next steps, if the SARC-F score indicated that a loss of muscle function has occurred. It is important to treat the underlying causes where possible, because sarcopenia can, in many cases, be caused by a number of factors, including poor nutritional intake, bed rest, underlying conditions such as bone and joint diseases, neurological disorders and metabolic disorders (Cruz-Jentoft and Sayer, 2019)
- Agree the desired outcomes with the patient, emphasising that improvements in function are possible. These could include identifying potential improvements in the activities of daily living, reduction in falls and undertaking an assessment of quality of life to use as a baseline (Cruz-Jentoft and Sayer, 2019)
- Schedule ongoing monitoring and review.
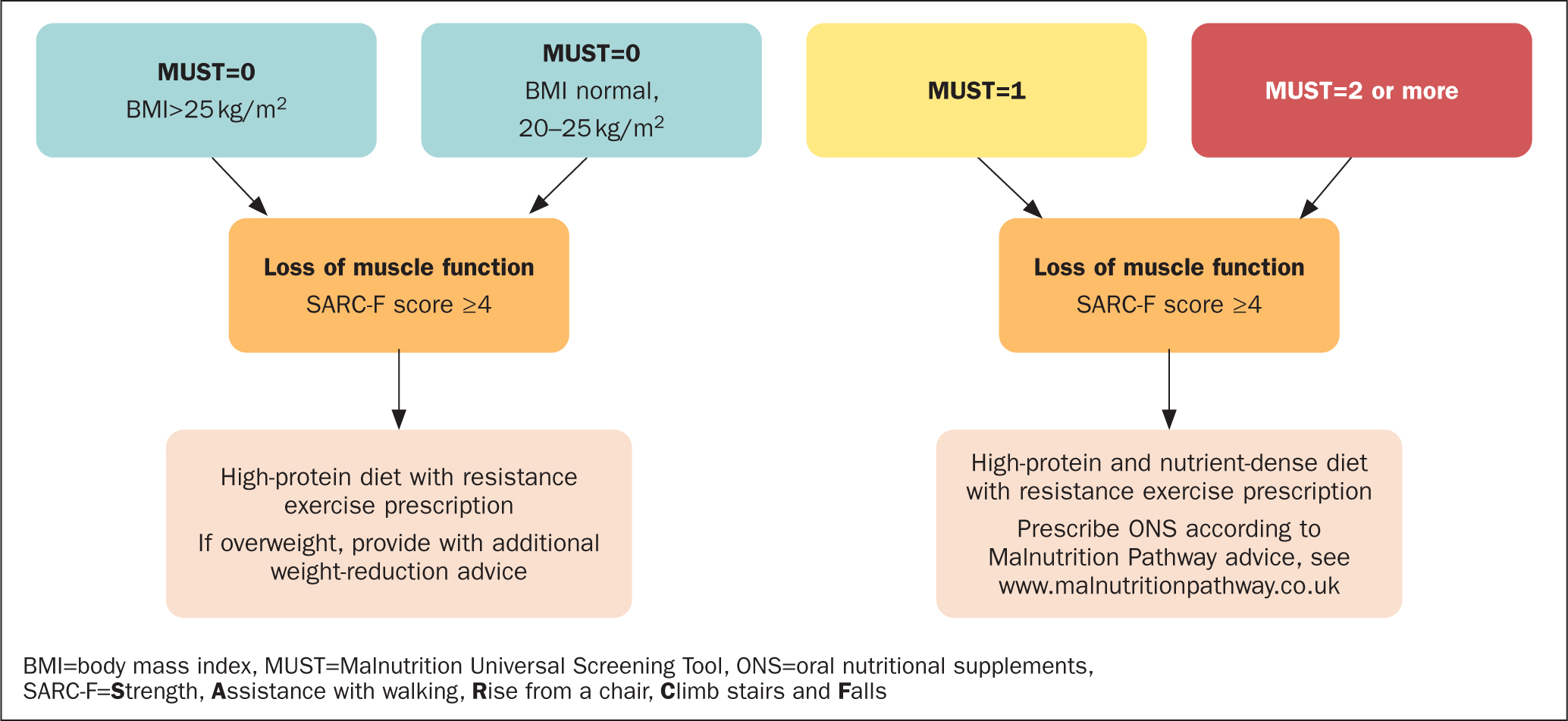 Figure 2. Managing Malnutrition and Sarcopenia in the Community (Holdoway and Ashworth, 2021)
Figure 2. Managing Malnutrition and Sarcopenia in the Community (Holdoway and Ashworth, 2021)
Optimising nutritional intake: an evidence-based approach
Protein
Muscle makes up about 45–55% of body mass and has an important role for an individual's mobility and health. Muscle mass is maintained through a balance of muscle protein synthesis and muscle protein breakdown (Kumar et al, 2009); however, in older patients, muscle protein breakdown can exceed synthesis and their muscles may start to shrink as they age and lead an increasingly sedentary lifestyle.
Adequate protein intake is essential to maintaining muscle mass and promoting muscle synthesis. However, older adults often have a reduced food intake, which can result in lower protein intake, with an estimated 10% of those receiving community care and 35% of those in institutional care failing to meet European Society for Clinical Nutrition and Metabolism (ESPEN) recommendations (Deutz et al, 2014). According to the Scientific Advisory Committee on Nutrition (SACN) (2021), 27% of 65 to 74-year-olds and 33% of over 75-year-olds have a protein intake that is below the current reference nutrient intake (RNI) for adults aged over 18 years of 0.75 g protein/kg body weight (Department of Health, 1991).
Another concern is that protein requirements for older adults may actually be higher than the current UK recommended intake The RNI was set in 1991 and it is possible that, as average body weights have increased since then, protein requirements may also have increased. Bauer et al (2013), for example, suggested a higher intake, namely that, to maintain and regain lean body mass, older adults (older than 65 years) require 1.0-1.2 g protein/kg body weight, with higher amounts for active/exercising older adults (equal to or more than 1.2 g/kg/day) and in acute or chronic disease (1.2-1.5 g/kg body weight/day). There is some evidence to suggest that 25–30 g of protein is needed at each meal to build and maintain muscle—this amount represents between one third to half of daily protein requirements of a 60 kg person, whose requirement is 1.0-1.5 g protein/kg (60-90 g protein/day) (Deutz and Wolfe, 2013; Mamerow et al, 2014; Paddon-Jones and Leidy, 2014).
It is important that protein intake should be spread out through the day to maximise muscle protein synthesis. Older people should aim for about 0.4-0.6 g protein/kg body weight/meal for three meals a day, which equates to 20-30 g per meal for a 50 kg older person, or 28-42 g per meal for a 70 kg older person.
For obese individuals, calorie intake may need to be limited to enable them to lose body fat and improve physical function. A safe rate of weight loss in those who are overweight or obese is considered to be about 0.5 kg/week (Batsis and Villareal, 2018). A lower-carbohydrate, higher-protein diet may not only enable a reduction in fat mass, but also preserve lean mass (Clifton et al, 2014), which is of key importance in managing sarcopenia.
A 20 g portion of protein equates to 3 eggs or a 100 g steak or 500 ml of milk or 80 g of peanut butter and consideration needs to be given to the fact that a frail elderly person may be unable to consume such quantities at one meal let alone several times a day. If protein deficit is significant, dietary advice may not therefore be enough to adequately increase intake, particularly in the presence of poor appetite.
Prevention: considering the whole diet
The SACN (2021) recently published a dietary survey of older adults living in the community that suggested there were excessive intakes of saturated fat, free sugars and salt, which failed to meet recommendations for intake of fruit, vegetables, fibre and oily fish together with low intakes of vitamin A, vitamin D, riboflavin and folate.
Although there currently appears to be no overall consensus on the most appropriate diet to prevent sarcopenia, it is thought a Mediterranean dietary approach, which includes fruit and vegetables, nuts, olive oil, legumes, more fish and poultry than red/processed meat and lower amounts of butter, cream, margarine, sweetened fizzy drinks and confectionery, may have the potential to be an effective strategy to improve the quality of the diet and therefore prevent sarcopenia (Granic et al, 2019).
Oral nutritional supplements for those at high risk of malnutrition
NICE guidance (2017) advises health professionals to consider oral nutrition support for those at risk of malnutrition. This includes dietary advice and the use of oral nutritional supplements (ONS), where appropriate. ONS, in addition to dietary advice, have been shown to significantly improve protein intakes and consequently clinical outcomes—particularly, in the case of high-protein ONS (Cawood et al, 2012)—and may be necessary to help meet the requirements of patients at high risk of malnutrition. Nutritional supplements also provide additional energy and micronutrients to improve overall nutrient intakes. There may be instances where ONS may be appropriate in obese individuals with sarcopenia, for example, if significant unintentional weight loss has occurred in the presence of disease, and a referral to a dietitian may be required in these situations.
The importance of exercise in combination with diet
Exercise in combination with diet can improve muscle strength and physical performance in older adults with sarcopenia (Wu et al, 2021). Exercise programmes designed to improve strength and balance should be delivered over several weeks or months, and can lead to a reduction in falls of up to 54% (Skelton et al, 2005). Individualised regimens or supervision from appropriately qualified health professionals (eg physiotherapists) should therefore be sought so that advice is tailored to the individual.
Considerations for nurses
There are a number of areas where nurses can assist in the identification, treatment and management of malnutrition and sarcopenia in the older population. These include:
- Building conversations about appetite, dietary intake and hydration into everyday patient contact
- On contact with patients, be aware of subjective indicators of patient weight loss, eg:
- – Thin or very thin in appearance
- – Loose-fitting clothes/jewellery
- – History of recent unplanned weight loss, especially in overweight or obese patients who may have lost significant amounts of weight, but still have a BMI over 25 kg/m2
- – Changes in appetite, eating or swallowing difficulties.
- Identify ways to integrate nutritional screening and care into pathways and the electronic patient record, particularly when dealing with patients and patient groups whose condition creates nutritional difficulties and dietary issues, and places them at high risk of malnutrition and sarcopenia
- If a patient is malnourished/at risk of malnutrition, take action and create a nutritional care plan
- Consult the local dietetics department and local policies and guidelines on malnutrition, where available
- Flag high-risk patients, offer dietary advice at first opportunity and consider the need for ONS based on risk category, the patient's appetite and their ability to modify their diet (see Table 1 for more advice)
- Some patients require low-protein diets for therapeutic reasons to manage specific conditions. If concerned, check the patient's nutritional care plan and refer to a dietitian before taking the decision to increase protein intake.
Conclusion
Sarcopenia and malnutrition are increasingly important issues among the ageing population of the UK. Health professionals are becoming more aware of the consequences of muscle mass loss on long-term outcomes, particularly for patients who are older and have pre-existing conditions. The increasingly obese population means that loss of muscle mass can often be hidden by the presence of fat mass. It is important therefore to identify those at risk of both conditions by incorporating nutritional screening and physical performance tests into patient reviews.
Building conversations about appetite, dietary intake, hydration and exercise into everyday older adult patient contacts can help nurses identify when issues relating to malnutrition and sarcopenia are occurring in this group. Although there is currently no consensus on the treatment of sarcopenia, advice on healthy eating and following a Mediterranean diet approach, in combination with advice on regular exercise, may be effective strategies to support prevention, while oral nutrition support together with exercise are indicated for those with malnutrition and sarcopenia.
Nurses, who work closely with dietetic and physiotherapy colleagues where appropriate, can ensure that high-risk patients are offered relevant advice on nutritional intake and tailored exercise advice. The steps they take to assess and manage older patients, whether living independently or resident in care homes, will not only improve patient outcomes, but also help reduce the costs of health and social care by preventing hospital admissions and reducing escalation to a greater level of care needs.
KEY POINTS
- The effects and clinical consequences of malnutrition and sarcopenia are wide ranging and can detrimentally affect long-term health and outcomes
- To tackle malnutrition and sarcopenia in an increasingly ageing population health professionals need to improve screening, treatment and prevention
- Sarcopenia may be more obvious in underweight patients, but obesity can often mask loss of muscle. Physical performance tests, such as sit to stand and 2-minute walk endurance tests, alongside traditional nutritional screening tools such as MUST, may therefore be helpful
- Dietary advice and oral nutritional support are important first-line treatments for patients at risk of malnutrition and sarcopenia. The importance of an adequate protein intake alongside resistance exercise should be emphasised
CPD reflective questions
- What subjective indicators would you be looking for in patients to ascertain if they are at risk of sarcopenia and malnutrition?
- Are you screening all elderly patients for malnutrition using a validated screening tool (eg MUST)? Are there tests you can put in place to measure the physical performance of patients and ensure that muscle mass is being screened, eg sit-to-stand tests?
- Do you incorporate questions on diet and exercise into everyday patient discussions?
- Do members of your team need further training on identifying and managing malnutrition and sarcopenia? Can you access training via your local dietetic department? If not, consider resources such as those available from www.malnutritionpathway.co.uk (see Table 1)


