As health professionals, our ultimate aim is to promote a healthy lifestyle, to deliver high-quality care and to enable people to live long and healthy lives. So how should nurses approach and support those patients who choose to opt out of treatment, and instead choose intentional non-adherence?
In 2013, UNAIDS launched its ambitious HIV 90-90-90 targets, meaning that, by 2020, 90% of all people living with HIV would know their HIV status, 90% of all people with diagnosed HIV infection would receive sustained antiretroviral therapy (ART) and 90% of all people receiving ART would be virally suppressed. It was envisaged that if these targets were achieved then HIV eradication would be possible (UNAIDS, 2014). Since the targets were launched in 2013 there has been increasing momentum and discussion to add a fourth 90% – good health-related quality of life (QoL) for people living with HIV (Harris et al, 2018). Access to ART has meant that substantial progress has been made in reaching these targets globally (UNAIDS, 2017).
The World Health Organization (WHO) strategy (2022) called for a person-centred approach to care for people living with HIV and recognised that viral suppression should not be the only focus. However, the WHO has failed to come up with a specific plan to ensure health-related QoL for people living with HIV and to acknowledge that it is not simply about reaching an undetectable viral load, but also helping patients face challenges such as depression, anxiety, financial stress and HIV-related stigma (Lazarus et al, 2016). Bourne and Croston (2022) pointed out that the impact of an HIV diagnosis affects many aspects of a person's life. People living with chronic conditions often have multifaceted healthcare needs related to the burden of complex symptoms and the impacts of advancing illness on their QoL (Sawatzky et al, 2018). Depression and low self-esteem, for example, are known risk factors for non-adherence to treatment in long-term conditions (Grenard et al, 2011).
What does QoL mean to individual patients? WHO has defined QoL as:
‘An individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.’
Indicators of QoL include wealth, employment, environment, physical and mental health, education, leisure time, social relationships, family, religious beliefs, safety, security, housing and freedom (Barcaccia et al, 2013). Barcaccia et al (2013) stressed that QoL relates to someone's level of acceptance of their current condition, and their ability to regulate negative thoughts and emotions about their condition, in this case their HIV status. This concept helps explain why two people in exactly the same situation will have very differing concepts of their QoL. It also helps give some perspective on why someone may choose to stop their ART.
Health professionals are at risk of bias and making presumptions about what is important to our patients. Addington-Hall and Kalra (2001) argued that health professionals will unintentionally make QoL judgements when making decisions about the delivery of care for their patients. Patients sometimes make choices with which health professionals do not agree. Do we judge people or accept their choices? Schwartz and Sprangers (2002) argued that health-related QoL is recognised as being subjective in nature, which can cause confusion for clinicians. They pointed out that the term subjective, as opposed to objective, is being used in reference to the sense of importance to the person, and stressed that patients should be the primary source of information regarding their QoL. In other words, health professionals should recognise that, when their assessment of quality of life is at odds with that of the patient, it is the patient who should have the final word (Addington-Hall and Kalra, 2001). Bourne and Croston (2022) maintained that QoL should be seen as a dynamic, ever-changing process that needs to be evaluated at regular intervals as part of good clinical care. Sudden and significant changes in a person's circumstances may alter a person's QoL and, in turn, affect adherence. Sawatzky et al (2018) stressed the need for health workers to promote QoL assessment instruments, including patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs), as a means of enabling clinicians to improve person-centred care. PROMs are important because patients have the best perspective on the impact of their treatment, which may also affect their adherence to therapy and other pressing issues.
Adherence is an important outcome measure because non-adherence to ART increases morbidity, mortality and health service costs, as well as the risk of resistance and onward transmission (Stricker et al, 2014). In order to better understand adherence to treatment we need to consider the factors that influence a patient's choice to stop ART. Applying this approach in practice requires a holistic, empathetic and no-blame approach, encouraging discussion around intentional non-adherence and any doubts or concerns patients have about treatment (National Institute for Health and Care Excellence (NICE), 2009). Non-adherence falls into two categories: intentional and unintentional (NICE, 2009). Unintentional non-adherence occurs when a patient unintentionally struggles to take their tablets due to barriers that are beyond their control, for example forgetfulness or drug and alcohol issues. Intentional non-adherence is when a patient intentionally decides to stop treatment.
In 2020, it was estimated that there were 105 200 people living with HIV in the UK; 94% of these people have been diagnosed, and therefore know that they have HIV. Ninety-eight per cent of those diagnosed with HIV in the UK are on treatment, and 97% of individuals on treatment are virally suppressed, which means that they cannot pass on the virus. This leaves approximately 3% of people with a diagnosis of HIV who are not virally suppressed (National AIDS Trust, 2019). This article seeks to explore potential reasons why someone is not virally suppressed, specifically focusing on intentional non-adherence.
Discussion
The author has 30 years of experience in the HIV field and originally had a palliative care role. Her job was to facilitate a pain-free and dignified death. When ART became available, many patients were initiated on to difficult and toxic regimens where side-effects were severe. However, the desire to live meant that many patients endured these side-effects, which often caused overwhelming distress. The world of HIV has changed dramatically and HIV is no longer classed as a life-limiting disease requiring palliative care but as a long-term condition (Jelliman and Porcellato, 2017). Although diagnosis can be traumatic and brings with it many emotions, we can now offer people hope. If people are diagnosed early and ART is initiated in a timely manner, their prognosis is extremely good and, potentially, they can live as long as someone without HIV (NHS website, 2022). Therefore, watching someone intentionally non-adhere and opt out of taking life-sustaining treatment feels uncomfortable and tragic if it leads to early death. For HIV specialist nurses who have worked in the HIV field for a long time, witnessing many people die from HIV-related illnesses has had a significant impact and has been a huge challenge to navigate. Many of them have also worked as Macmillan nurses and district nurses and have looked after palliative patients: those for whom medication was no longer an option and for whom all we could offer was effective symptomatic relief and emotional support. The aim was to enable our patients to have a dignified and pain-free death. Therefore, to have a patient in front of you who chooses to opt out of ART brings with it ethical and emotional challenges.
Adherence challenges are not isolated to HIV. Adherence is an issue across many long-term conditions (Nieuwlaat et al, 2014). In other long-term conditions, patients' beliefs about their condition and their treatment are important drivers of non-adherence (Leventhal et al, 2016). Intentional non-adherence and struggling with adherence are two very different things. Health practitioners deal with many patients who struggle with adherence but who ultimately want to take their ART and adhere so that they reach undetectable levels.
A comprehensive caseload review with the HIV community team in Brighton and Hove (Sussex Community Foundation Trust) was carried out in 2022 to identify and explore why some patients with HIV decided to stop ART. It was identified that 45% of the caseload struggled with adherence issues and needed intense support around this specific issue. Some 25.5% of the caseload had a detectable viral load. Of those with a detectable viral load, 9.8% had chosen to opt out of treatment, otherwise known as intentional non-adherence. The recent caseload review identified reasons why people living with HIV opt out of ART (see Box 1).
Box 1.Case review findings: why patients with HIV opt out of taking antiretroviral therapy
- Associating tablets with HIV-related stigma
- Adoption of personal belief systems such as religion or an alternative therapy
- Patients feel well
- Denial
- Fear of side-effects and medication toxicity
- Medication fatigue
- Invincibility/optimistic bias
- Depression/low self-esteem
- Social isolation with no incentive for good health
- Desire to survive, but not with HIV
- The need to exercise control
- Punishment of significant others
- A desire to die
The author has personally witnessed the impact of the reasons listed on patients, resulting in intentional non-adherence. Religion, social isolation and the need for control will be discussed in more detail, with short illustrative case studies.
Religion
Religion can impact on a person's response to medication and treatment. Alio et al (2019) carried out an exploration of religious leaders and their role in the lives of people living with HIV. The overarching theme was ‘to love the sinner but hate the sin’, and to help people with HIV reconcile with their religion and renounce inappropriate behaviours, in turn causing those with HIV to feel unaccepted and undeserving. Many religious dominations have condemned same-sex behaviours and refused to carry out same-sex wedding ceremonies (Sherkat, 2002). However, it is important to note that last year the Methodist Church became the largest religious denomination in the UK to allow same-sex marriages. Same-sex marriage is not permitted in the Church of England (CoE) or the Roman Catholic Church. However it is welcomed in the Scottish Episcopal Church, the United Reformed Church and the Quakers in Britain (Farley, 2021). The CoE has a mixed position on LGBTQ rights. It currently allows gay men and women, and trans men and women, to serve in the clergy. The CoE will allow blessings and prayers after same-sex marriage ceremonies, but not full religious marriage ceremonies for same-sex couples (Changing Attitude, 2022).
More studies are needed to explore the implications of sexual identity and religious status on mental health and wellbeing. Barnes and Meyer (2012) investigated the relationship between exposure to non-affirming religious environments and internalised homophobia and its effect on mental health in a sample of people from the LGBTQ community in New York City. They concluded that exposure to non-affirming religious settings led to higher internalised homophobia, more depressive symptoms, and less psychological wellbeing, which, in turn, could impact on self-worth, self-care and potentially lead to adherence issues such as intentional non-adherence. It is important to note that religious groups can provide valuable support networks to people from the LGBTQ community (Weber and Pargament, 2014). However, these positive experiences tend to be seen in LGBTQ-affirming religious groups (Dehlin et al, 2015). See the case study in Box 2.
Box 2.Case study: religious belief and adherence to treatmentAnn* was a 38-year-old woman who stopped taking her antiretroviral therapy (ART) due to her personal belief system. She was a person with a strong religious faith who struggled to reconcile her beliefs with her diagnosis and status. Ann had spent many years denying that she had HIV. Later she believed that God had healed her because her church's pastor had told her this and had also explained to her that taking ART compromised her belief in God and showed a lack of faith. Ann stopped taking her ART and, as a result, she became severely immunocompromised and her mental health deteriorated. She displayed hoarding tendencies, self-neglect and was socially isolated.She was admitted to hospital emaciated and very near to death. Her CD4 count was 11 cell/mm3 and her viral load was 2 500 000 copies/ml. She remained an inpatient for under a week and was discharged home after 5 days. The GP visited and tried to get her readmitted because she remained very unwell, but she refused.Social services came to assess her needs with the aim of implementing a care package but deemed her property a health and safety risk to staff because of the hoarding, and the offer was withdrawn. She was known to the HIV Community Team who had helped intermittently for years when she had chosen to engage. Following a multidisciplinary team meeting the community HIV nurses undertook a home visit. On assessment, their opinion was that Ann was in need of palliative care and therefore was referred for hospice care. She was underweight, cachectic, her haemoglobin was 7.9 g/dL, and she had stopped eating and drinking due to severe oesophageal pain. She was admitted to the hospice.The palliative consultants were very caring and interested in Ann as an individual. They discussed her case with the HIV Community Team in detail. A few days into her admission they discussed restarting ART to which she agreed because she was frightened of being so near to death. She was an inpatient at the hospice for 7 weeks and became stronger by the day. She gained 12.7 kg in weight, her mobility improved and she became fully adherent to ART. To date, her viral load remains undetectable and she is engaging with care.* The patient's name has been changed
The need for control
The need for control cannot be underestimated. As soon as we become a patient we experience a loss of control. Historically, patients have been seen as passive – obeying the nurse and the doctor. If they did not protest they were seen as ‘good patients’ (Truglio-Londrigan, 2015). Patients trusted the nurse and allowed them to make decisions, similar to being treated as a child (Phillips, 2016). Choosing not to take life-sustaining treatment could be seen as being about regaining some control similar to the complex nature of eating disorders such as anorexia. Other authors have discussed the control paradox:
‘Power struggles in therapeutic relationships are disastrous as they force people who feel out of control to cling more desperately to the only control they have.’
In other words, the more practitioners try to take power away from or enforce their opinions on a patient, the more the patient's symptoms and behaviours are likely to escalate. It is imperative that health professionals and patients work together as partners and equalise the power imbalance (Henderson, 2003).
The language used is crucial. Compliance can be defined as the will to consent to the wishes of another person (Buchmann, 1997). Compliance relates to a paternalistic or even autocratic relationship, in which someone is seen as either following instructions (compliant) or disregarding them (non-compliant). Being labelled ‘non-compliant’ by health professionals becomes a barrier to empathising with a patient's perspective. It prevents us understanding why the patient is unable or unwilling to adhere to lifestyle changes, medication regimens or advice. It places responsibility for a perceived failure to optimise health outcomes on the patient, and assumes that health professionals know best (Chapman, 2018).
Concordance is an indicator of the quality of decision-making in health care. It depends on patients being well informed. A concordant relationship promotes self-management of health; it is based on trust, enabling patients to discuss with the health professionals providing care how other aspects of their life influence, and are influenced by, health and health interventions. It is a partnership to achieve the best health and wellbeing outcomes (Chapman, 2018). See the case study in Box 3.
Box 3.Case study: the need for controlHannah* was a young female patient aged 22 years. She had struggled to come to terms with her diagnosis and to adhere to her ART medication. Voluntary sector workers and health professionals had tried hard over the years to engage with her. Her engagement was intermittent and she had had recent inpatient admissions for pneumocystis pneumonia due to a low CD4 count.On referral to the HIV Community Team, she had a CD4 cell count of 4 cells/mm3. The aim of the referral was to help with adherence and offer extra support. The team faced a complex case, in that many health professionals had been involved in Hannah's care over the past 7 years, all trying different ways to encourage her to take her medication. On reflection, conversations had been weighted heavily on encouraging her to take her medication with the emphasis that, if she did not, she would become unwell and could die. One could argue that there was a power struggle between the patient and the healthcare workers.The patient's relationship with her parents was complex, and she was often inconsistent in what she said to members of the multidisciplinary team. To some she articulated a desire to have a partner, children and a career and to others she clearly stated that she no longer wanted to take ART, and that she wanted her life to end. Multidisciplinary team meetings were often spent discussing whether or not she had capacity. Capacity means the ability to use and understand information to make a decision, and communicate any decision made. A person lacks capacity if their mind is impaired or disturbed in some way, and this means the person is unable to make a decision at that time, according to the Mental Capacity Act 2005.For a while, Hannah underwent directly observed therapy visits, Monday to Friday, in which staff observed her taking her ART. However, this was short lived. She started to cancel visits and her engagement became sporadic. The team visited her one day and took her bloods. Her viral load had escalated and she was extremely weak and underweight. She was admitted to the ward. Very sadly, Hannah died 6 weeks later with end-stage HIV, despite all the interventions from so many healthcare workers.* The patient's name has been changed
The death of a young patient, as in the case study in Box 3, leaves members of the wider multidisciplinary team emotionally exhausted, incredibly sad, frustrated and with many unanswered questions. As an HIV service we spent much time reflecting. Had we listened enough? Had we accepted the patient's wishes to opt out of ART or had we tried too hard to impose our own wishes on her? And what could we learn from this case? When we witness a patient choosing not to take their medication and consequently see their health deteriorating before our eyes it leaves us feeling helpless. The ‘right to die’ is a highly emotive topic. Respecting someone's choice to stop life-sustaining treatment is complex. Liberty and autonomy, or self-government, are sources of human dignity too.
The General Medical Council (GMC) has discussed personal beliefs and medical practice. It has stated:
‘You must respect a competent patient's decision to refuse an investigation or treatment, even if you think their decision is wrong or irrational. You may advise the patient of your clinical opinion, but you must not put pressure on them to accept your advice.’
Social isolation
Social isolation and loneliness are being increasingly recognised as serious public health issues. There is growing evidence of social isolation and its negative effect on health outcomes (Holt-Lunstad, 2020). If you have no one in your life who cares about you then, one could argue, what is the incentive to look after yourself and care for yourself? When an individual develops the feeling of being isolated, whether it is actual or perceived, their health can be compromised (Bhatti and Haq, 2017). See the case study in Box 4.
Box 4.Case study: isolationLuke*, a young man aged 27, was referred to the HIV Community Team. He had chosen to stop taking his ART as he wanted to die.Luke had experienced stigma and discrimination due to his HIV diagnosis and this had caused him to retreat and isolate himself from friends and family. The HIV specialist nurses had gently made it clear that they advised he take ART and explained the consequences of him not taking his medication. They had also decided as a team to actively show him that they respected his decision to opt out of ART. The nurses attempted to visit weekly and were there to listen to him, to ‘hear his voice’. Their aim was to help him die with dignity as that was his wish, and to support his family too.In a situation such as this, advanced care planning is crucial because it provides the opportunity to not only prepare the patient, but also to prepare family members. The patient had asked that the nurses take the advanced care planning documentation to his home and help him fill it in. He had also made it clear that he did not want resuscitating so the nurses had advised him to discuss this with his GP because this would require filling out a ‘do not resuscitate’ form.Luke's CD4 cell count was extremely low and he was suffering with recurrent thrush for which he was taking prophylactic fluconazole. Although it was hard to watch a young patient choose to opt out of ART, as a team, the nurses felt they were approaching the situation appropriately and sensitively. At any point the patient could change his mind and ask to restart ART. This was the preferred and desired outcome; however, those involved in his care had to respect his wish not to take ART and continue to offer him high-quality care.Robust interdisciplinary working and strong referral pathways into palliative care are crucial. This particular patient was referred to the palliative care team at his request for symptom control. For 2 years the HIV specialist team and the palliative care team took care of this patient and liaised with one another regularly. One day Luke chose to restart his medication and decided that he did not wish to die but wanted to live. He restarted his ART and has grown stronger each day.* The patient's name has been changed
This brings us back to the question of QoL and Bourne and Croston's (2022) crucial point that it should be seen as a dynamic, ever-changing process that needs to be evaluated at regular intervals as part of good clinical care and account for elements such as sudden and significant changes in a person's circumstances, which may in turn affect adherence. In this case, the patient went from intentional non-adherence to adhering fully to his medication.
The role of the practitioner
What is the role of the practitioner when caring for those who opt out of treatment? How should they respond? Trauma-informed care is crucial when caring for patients who are choosing not to take their ART. The five principles of trauma-informed care are safety, choice, collaboration, trustworthiness and empowerment (Fenney, 2019). Trauma-informed care shifts the focus from ‘What's wrong with you?’ to ‘What happened to you?’. A trauma-informed approach to care recognises that health professionals need to have a complete picture of a patient's life situation – past and present – in order to provide effective healthcare services with a holistic approach. Adopting trauma-informed practices can improve patient engagement, treatment adherence and health outcomes.
There are many elements to supporting a patient to adhere to their medication (see Figure 1).
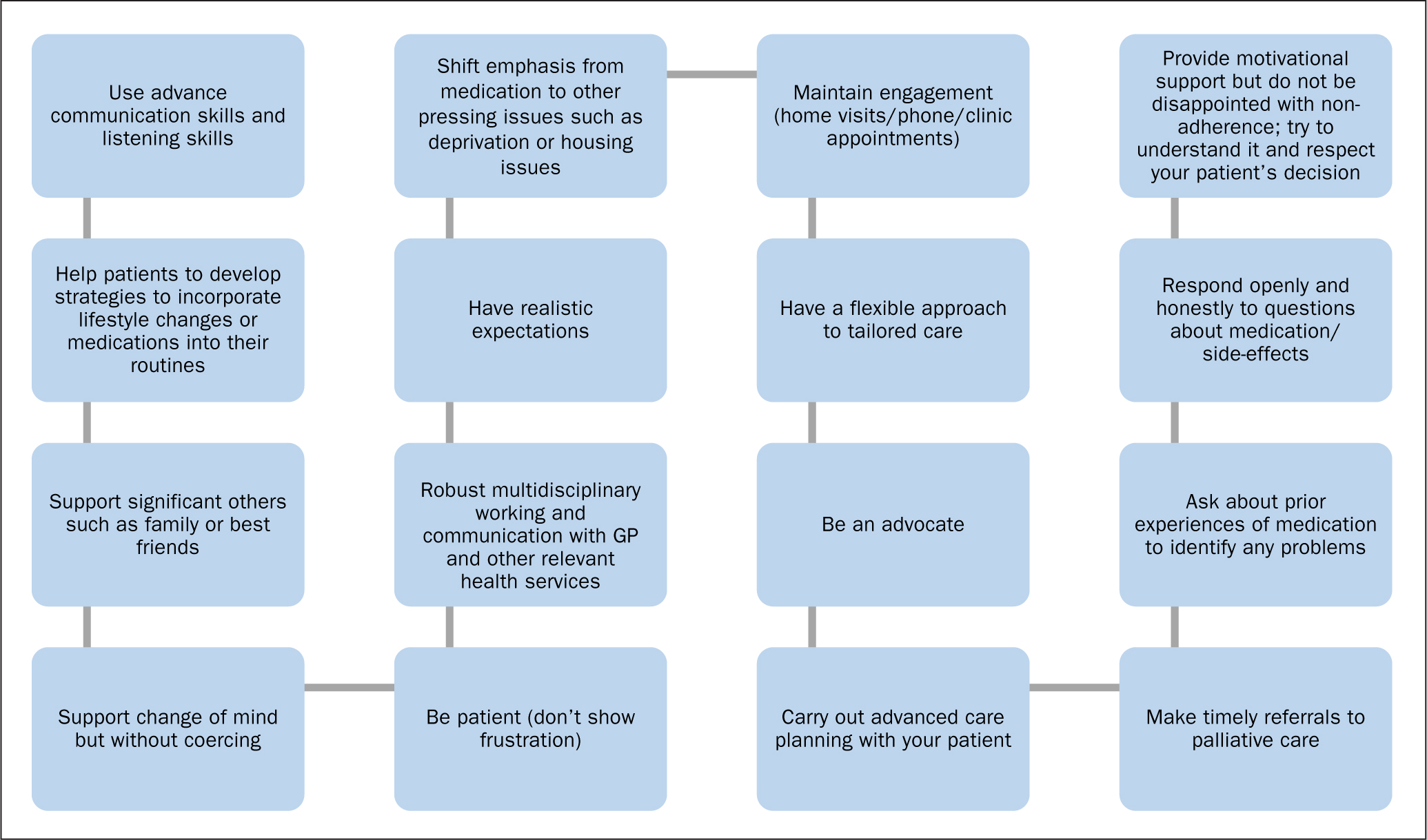
More information on supporting adherence is available from Downes and Foote (2019), who have produced best practice guidance. NICE's (2009) medicines adherence guidelines provide recommendations for supporting shared medication decision-making and adherence. Health professionals need to talk with patients so that they understand a patient's perspective and establish key medication beliefs before prescribing new treatments and when reviewing medicines. NICE (2009) recommends using standardised assessment tools, such as the Beliefs about Medicines Questionnaire (Horne et al, 1999) or by finding out from a patient what they know, believe and understand about their medicines, including any specific worries they may have. Doing this gives nurses an opportunity to help correct any mistaken beliefs and help support patients' decision-making around their treatment and care.
Conclusion
It is vital to understand the psychological reasons and issues that lead someone to choose to opt out of ART so nurses are better able to help patients on their journey (Grant et al, 2011). Trust is the most important factor in patient satisfaction and adherence to care. Health professionals need to develop a concordant relationship with patients (Chapman, 2018). Respecting a patient's choice, even if we do not agree or understand it, is crucial and our duty of care remains the same with patients who choose to stop ART. HIV specialist nursing teams, both nationally and globally, manage patients with complex medical and psychosocial needs. The case studies in this article demonstrate the complex nature of some patients. Maintaining robust links within and between teams, multidisciplinary team working and awareness of palliative care services are all important.
Continuously striving to increase the quality of care nurses deliver to patients and improving the patient experience is vital. Using the skills of other multidisciplinary teams and in so doing supporting each other is beneficial. Whether or not a patient is taking ART, the quality of care that nurses provide should remain the same.
KEY POINTS
- Antiretroviral therapy has made it possible for people with HIV to be virally suppressed, one of UNAIDS' 90-90-90 targets. However, viral suppression should not be the only focus, quality of life is also important
- Patients' adherence to treatment may be affected by their religious beliefs, a need for control over some aspects of their life, and social isolation
- Health professionals need to have a complete picture of a patient's life situation to provide a holistic, non-judgemental approach to care. In this way they can support a patient to adhere to their medication
CPD reflective questions
- The quality of communication in interactions between HIV specialist nurses and patients has a major influence on patient outcomes. Reflect on barriers to communication that you have personally experienced. What have you put in place to overcome them? Reflect on your how your own self-perceptions can be a barrier to effective communication
- Reflect on your political and spiritual beliefs, and how you communicate with patients. How do you think these beliefs affect your views on supporting and communicating with patients? How would you act as a nurse if you fully acted out your political and spiritual beliefs? Is caring and communication for all patients equally in harmony with your political and spiritual beliefs? Make a note of your responses. What feelings came up for you when reading through each of the points?
- Robust multidisciplinary working and communication with GPs and other relevant health services is key to improved patient outcomes. Reflect on how well you work with other services involved in your patients' care. How could you improve your own interdisciplinary working?
- Patients make choices with which we, as health professionals, do not always agree. Think back and reflect on conversations you have had with patients about their lifestyle choices. Do you judge people or accept their choices? Do you have your own biases that you need to work on?


