HIGHLIGHTS
- The first in-depth global study on underresearched facets of VAT initiatives.
- VA professionals interviewed universally endorsed the benefits of specialized VATs.
- Participants reported improvements in patient satisfaction and clinical efficiency.
- Nonclinical personnel on VATs can alleviate barriers to data collection or analysis.
- Collaborations, data tracking, and outcomes dissemination can serve as VAT metrics.
Numerous vascular access devices (VADs) are placed worldwide annually,1 with up to 90% of all hospitalized patients undergoing catheter placement,2,3 resulting in substantial health care expenditures.4 Even under ideal clinical conditions, VAD failure rates range between 25% and 69% due to device malfunction or clinical complications.5,6,7,8,9 Nosocomial infections, such as central line-associated bloodstream infections (CLABSIs), are especially concerning given the plethora of associated comorbidities, including thrombosis, phlebitis, and bacteremia.10 Given the potential clinical and financial benefits of optimized vascular access (VA) practice, there is an imperative to establish VA teams (VATs) with expertise in VAD selection, placement, and management.3,11 Specialized training inVA may reduce VAD failure rates, leading to better clinico-economic outcomes.2,3,1213,14
Growing demand for dedicatedVA providers has prompted a need to examine their impact. Authors of recent studies found a correlation between specialized VA training for nurses and emergency medicine clinicians and improved outcomes.15,16 In both studies, didactic-, simulation-, and procedural-based trainings resulted in department-specific and hospital-wide improvements in multiple outcomes, including first-time catheter insertion rates, postreferral placement duration, nosocomial complications, and patient and provider satisfaction.15,16 However, these single-site studies with emphasis on specific medical departments provide limited context for comparison. Mussa et al17 surmount some of these shortcomings by using a qualitative, multisite survey of multidisciplinary VAT members to explore the benefits of these teams at European institutions. Although authors of multiple studies2,15,16,17,18,19 have highlighted lowered hospital costs and enhanced patient and provider satisfaction with VATs in specific medical or geographic contexts, the generalizability of their findings is hampered by insufficient data on a worldwide, multi-institutional scale.
In this study, we aim to examine underresearched facets of VAT initiatives focused on diverse perspectives from VAT leaders or members from institutions around the globe. This framework evaluates diverse VAT roles in VAD management and elucidates factors or obstacles regarding establishment, propagation, and training for VATs. Additionally, underresearched barriers to collecting and disseminating VAT-related data are explored.
Methods
Study design
A semistructured interview approach based on a convergent mixed methods design was used, which combines qualitative and quantitative research elements to provide sufficient breadth and depth regarding the topics of interest. This approach was appropriate for the study considering the wide range of underresearched topics surrounding VATs, some of which required significant detail (ie, the impacts of VAT initiatives).20 In-depth interviews conducted with physicians, nurses, and specialist VA nurses determined the complexity and heterogeneity of VATs and their impact on clinical, efficiency, and patient-related outcomes. The inclusion criterion for participants was VAT leadership or membership. A screener questionnaire designed to establish VAT-related credentials was used, and the final list of respondents included representatives from Asia, Australia, North and South America, and Europe. The study was based on in-depth interviews with clinicians to indicate their perspectives regarding VA teams; no patient data were collected, and participants consented to the release of information obtained due to their participation.
Recruitment and screening were conducted in 21 countries with 38 potential interviewees who were identified through the judgment sampling method to ensure geographical diversity and capture perspectives from a range of roles, specialties, and experience levels. Fourteen VAT members and leaders from 9 countries were interviewed: Australia (n=2), Brazil (n=3), Canada (n=1), China (n=2), Colombia (n=1), UK (n=1), Italy (n=1), Sweden (n=1), and the USA (n=2). The interviewees included 5 physicians (2 surgeons, 2 anesthesiologists, and 1 intensive care physician), 6 nurses, and 3 specialist VA nurses with a range of experience levels: less than 5 (n=4), 5–9 (n=4), and 10 or more (n=6) years. The participants practiced at urban, teaching, or nonteaching hospitals (250–2400 beds) in various specialties, including primary care, oncology, and transplant medicine. Participants were anonymized with alphabetical codes derived from country names (ie, CH=China). Multiple participants interviewed from the same country were sequentially assigned numbers based on their interview dates (ie, CH1, CH2).
All respondents were recruited and interviewed between October 2020 and January 2021. Phone interviews (~1 hour) were semistructured and included open- and closed-ended discussion questions regarding various aspects of VATs. Questions in the discussion guide were formulated based on a targeted review of the literature (detailed in the Supplemental Methods) conducted on VAT initiatives to assess the global VAT landscape and identify underresearched topics that would benefit from clinician insights. The underexamined areas identified by the literature review informed questionnaire development, including heterogeneity of VATs (i.e., roles, responsibilities, tools, composition, and training or recruitment strategies), gaps in nonclinical outcomes (i.e., patient satisfaction and clinical efficiency), challenges underlying team formation processes, and constraints surrounding collection and dissemination of VAT-related data. The discussion guide was internally validated by the researchers, which included VA specialists and individuals who implemented VAT programs at their organizations and therefore have the relevant experience or qualifications.
Data collection and analyses
Reporting follows the Standards for Reporting Qualitative Research guidelines.21 All interviews were audio-recorded and transcribed with participants’ informed consent. The convergent mixed-methods approach22 was used to analyze participant responses. Qualitative data were thematically analyzed manually, and patterns in meaning were identified in the interview transcripts.23 Ranking questions using a 7-point Likert-like scale (1=no improvement at all, 7=significant improvement) were used to assess interviewees’ perceptions of VAT components, the impact of VATs. All responses to ranking questions were averaged using MS Excel (Microsoft, Redmond, WA) and presented using GraphPad Prism (GraphPad, San Diego, CA).
Results
Fourteen respondents participated in interviews focusing on 2 key thematic concepts:
- Fundamentals of VAT organization, duties, co-initiatives, and impacts, and
- Underresearched facets of VAT initiation, evaluation, and evidence dissemination.
An additional topical theme, the impact of COVID-19 on VATs, captured perspectives about the repercussions of the pandemic.
Theme 1. Fundamentals of VAT organization, duties, co-initiatives, and impacts
Subtheme 1. Diversity of VAT responsibilities
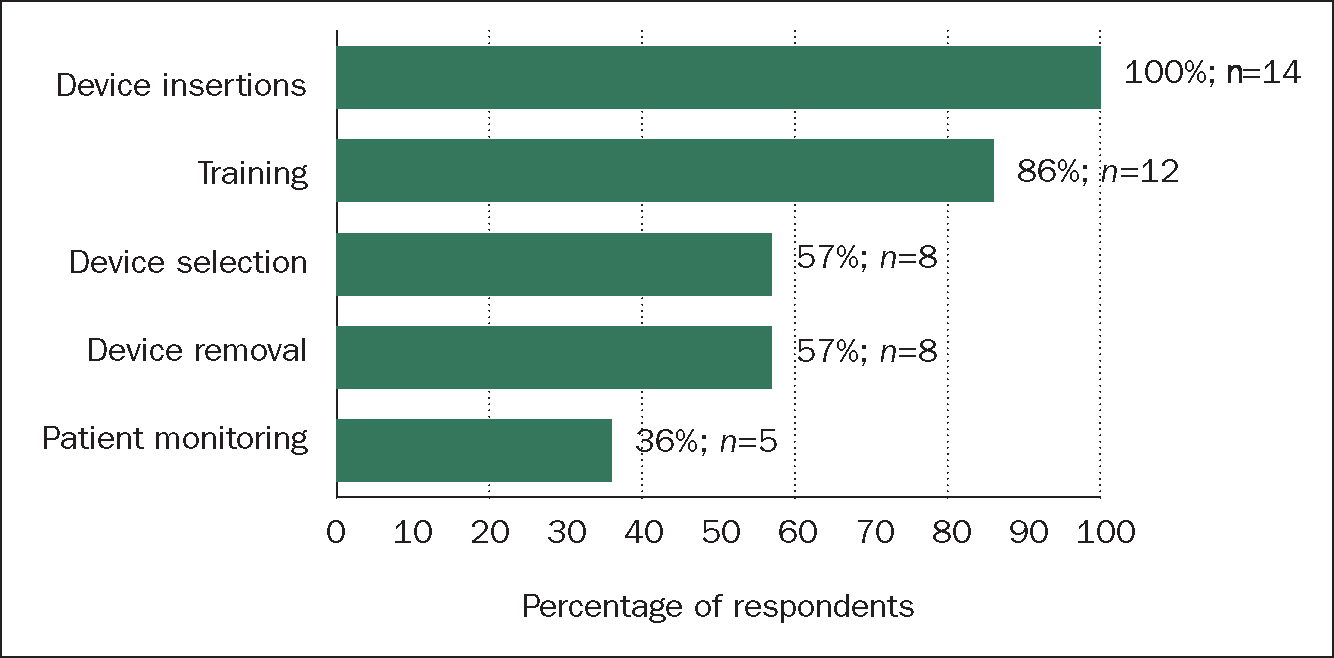
VAT responsibilities involved 1 or more aspects of VAD management: catheter insertions were the most performed function (100%; n=14), followed by training (86%; n=12), and device selection or removal (57%; n=8; Figure 1).Training types and responsibilities ranged from specialized exercises for VAT members to hospital-wide training by VATs (43%; n=6). Routine postinsertion patient monitoring was seldom stated as a team function (36%; n=5); however, all respondents (100%; n=14) reported troubleshooting postinsertion access-related issues on an as-needed basis.
‘We don't get a lot of time to involve with regular follow-ups, unless it is of a reactive nature…’
A1
Subtheme 2. VAT composition and recruitment
Team composition
Detailed team compositions are included in Table 1. Overall, there were 6 nurse-specific teams, 2 specialist VA nurse teams, 5 teams consisting of both nurses and physicians, and a physicians-only team. Occasionally, nonclinical personnel were included in supporting roles (ie, data collection and analysis).
Table 1. Vascular access team composition exhibits diversity
| Participant code | Country | Team composition |
|---|---|---|
| A1 | Australia | Specialist vascular access (VA) nurse |
| A2 | Australia | Specialist VA nurse |
| B1 | Brazil | Physician, biomedical researcher, scribe |
| B2 | Brazil | Physician, nurse |
| B3 | Brazil | Nurse |
| C1 | Canada | Specialist VA nurse |
| CH1 | China | Physician, specialist VA nurse, nurse, master's student |
| CH2 | China | Nurse |
| CO1 | Colombia | Physician, nurse |
| I1 | Italy | Physician, nurse |
| S1 | Sweden | Physician, nurse |
| UK1 | UK | Specialist VA nurse, nurse, assistant practitioner, health care administrator |
| US1 | USA | Nurse |
| US2 | USA | Physician champion, nurse |
‘My team is composed of 7 vascular surgeons only… and I have 1 biomedical (professional) who helps with data collection, and we have 2 scribes who help us in the performance of access’
B1
In China and Europe, VATs included both nurses and physicians, with specialized device insertion responsibilities:
‘We have 10 nurses: all specialists in infusion therapy. We have doctors who insert venous ports (as well as) other specialist nurses’
CH1
Recruitment strategies and training
Participants identified differing criteria for selecting new members, such as continued interest in VA, language proficiency, educational qualifications, VA skills, and prior experience. Overwhelmingly, 71% of respondents (n=10) preferred recruits with strong VAD placement skills and some VA experience but stipulated no formal degree or certification requirements. Only 1 interviewee from China detailed a structured approach and clear criteria set for VAT recruitment.
‘[Recruitment] criteria like the clinical skill is the first one; the second one is the education degree, also the communication skill, their interest in the role, and the English proficiency’
CH2
Fifty percent of the interviewees (n=7) specified that formal certification or credentialing is not a requirement for entry but a time-bound expectation after hiring. Only 29% (n=4) indicated the need for a formal educational degree. Nearly all respondents identified institutional and external options for didactic and hands-on training, supplemented with refreshers.
‘It [ongoing education and training] is definitely part of orientation when they [nurses] start, but we try to do an annual or bi-annual education day’
C1
‘Every member of the team needs to train and know the protocols and gears of the program. Training is conducted in different phases. In the first phase, the leader of nurses and I deliver a similar training to doctors and nurses. The members also study institutional protocols for insertion and device selection. After they know all that, they have an operational training with the ultrasound machine. After getting skilled with ultrasound machine, they go to a practical training in models. After they are confident with models, then they go to patients, they watch the first insertion and do 1 or 2 procedures with ultrasound and develop the skills’
CO1
Subtheme 3. VAT co-initiatives and tools
VATs use supportive biomedical technologies and co-initiatives to augment VA practices. Average utilization rates for 6 different VAT tools or co-initiatives averaged consistently around 85% (Figure 2). All participants reported relying on evidence-based protocols and advanced technologies such as point-of-care ultrasound, electrocardiography (ECG), and catheter tip location or confirmation systems for line placement. Evidence-based protocols were either used directly from literature (UK) or developed or modified by the institution (China).
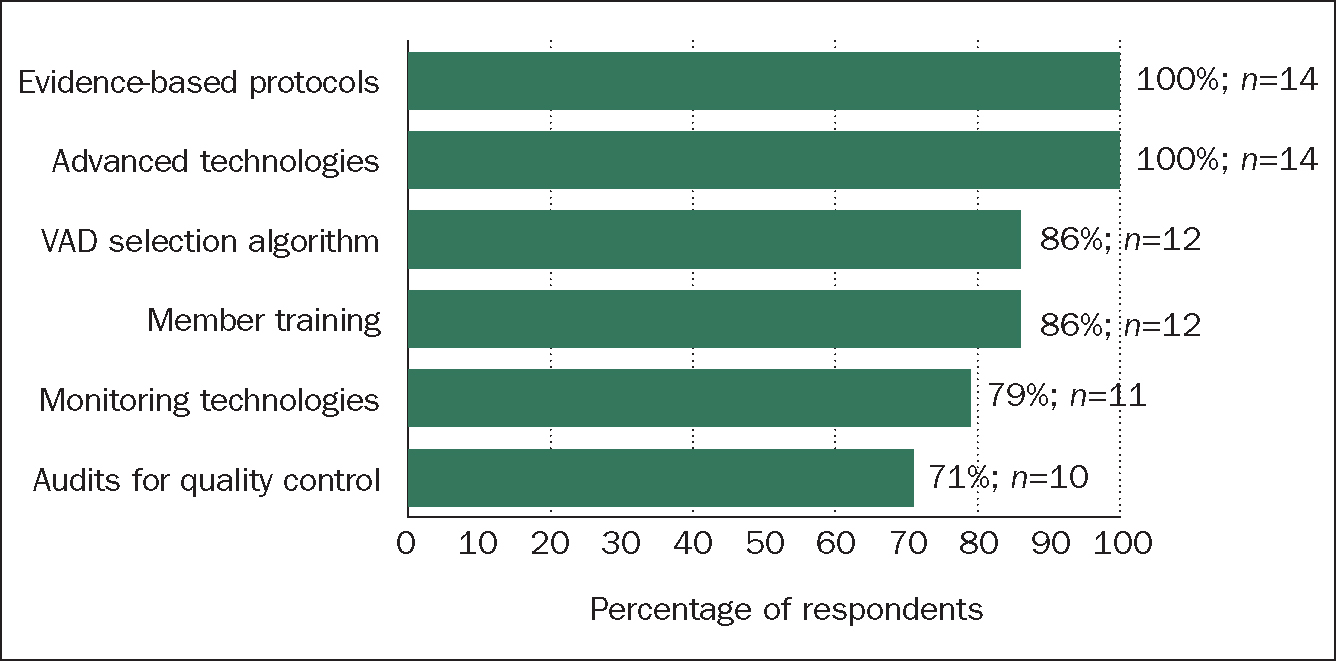
The majority reported using device selection algorithms (86%; n=12), VAT training exercises (86%; n=12), and database or spreadsheet applications for collecting VAT-related data (79%; n=11). VA trainings included online training portals, procedural or didactic instruction from experienced colleagues, educational conferences, and journal clubs. Systems used for tracking VAT-related data ranged from simple spreadsheet software (ie, MS Excel) to exclusive tracking databases to record, monitor, and analyze data. One US respondent used a specialized database to generate quarterly staff- and device-performance reports and noted an app-based real-time data entry system, making bedside charting easier and more accurate.
‘…I also provided quarterly outcomes on performance of the staff, and then we looked at things like how many lines [were placed]… we were basically looking at costs for the patient… costs for the hospital, and savings in terms of not placing a device that we didn't need’
US1
Bedside audits by VATs for quality control registered relatively modest participation (71%; n=10) and were reported as sporadic and inconsistent.
‘No, only if asked, not regular’
B1
‘Those [bedside audits, rounds] are all random and manual, with paper and clipboard… I try to do it once a week, but the objective is to do it once a month’
C1
Subtheme 4. Observed impact of VATs
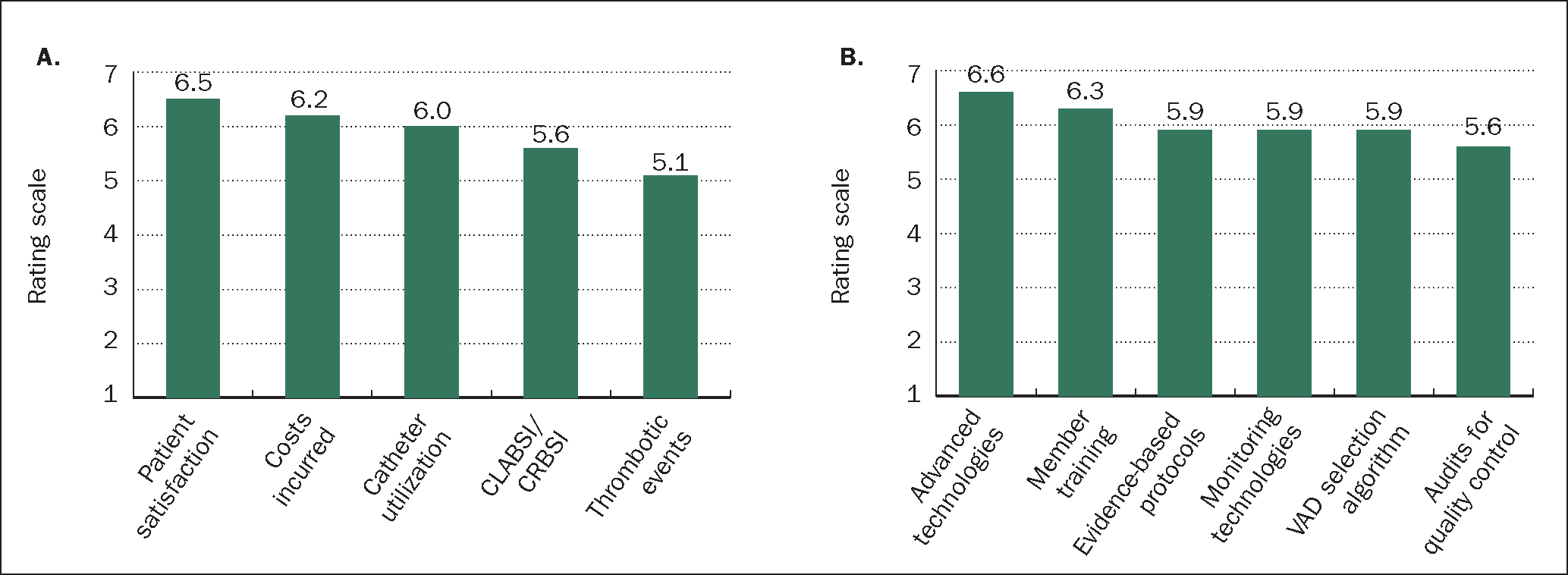
Interviewees rated the impacts observed post-VAT on a Likert scale of 1–7, with a score of 7 indicating a significant improvement (Figure 3A). Patient satisfaction (6.5) recorded the most notable improvements after VAT endeavors, followed by hospital costs (6.2). Interviewees noted efficiency enhancements such as time elapsed between the request and VAD insertions.
‘I look at the time from request of the access device to the time of insertion… For the [peripherally inserted central catheter (PICC)] lines and midlines we place, we do them within the first 24 hours of receiving the request’
UK1
Observed impacts on CLABSI rates and thrombotic events were relatively modest, with average scores of 5.6 and 5.1, respectively.
Using the 1–7 scale, interviewees were also asked to gauge the relative importance of the various co-initiatives for VAT impact assessment (Figure 3B). Advanced technology utilization (6.6) and ongoing member training (6.3) scored as the priorities for enhancing VAT endeavors. Evidence-based protocols, database implementations, and VAD selection algorithms (5.9) played relatively limited roles, while audits for quality control (5.6) emerged as the least influential co-initiative.
When asked open-ended questions regarding VATs’ own definition or metrics for success, respondents listed both clinical (e.g., complication rates) and nonclinical parameters (eg, cost savings, improved reimbursements):
‘For the success of the team, the most important is the decrease of complications and the satisfaction of our patients’
CH1
‘… in the end [after 3 years of data], we have a lot of significant reduction in cost with the best choice of the right catheter for the right patient for the right reason’
I1
‘… health insurance denying reimbursement, so that was a challenging situation. The team couldn't do anything with prior losses. They established catheter commission or group to check if the catheter had correct indication which solved reimbursement issues’
B2
Theme 2. Underresearched facets of VAT initiation, evaluation, and evidence dissemination
Subtheme 1. Impetus for VAT initiation and hurdles encountered
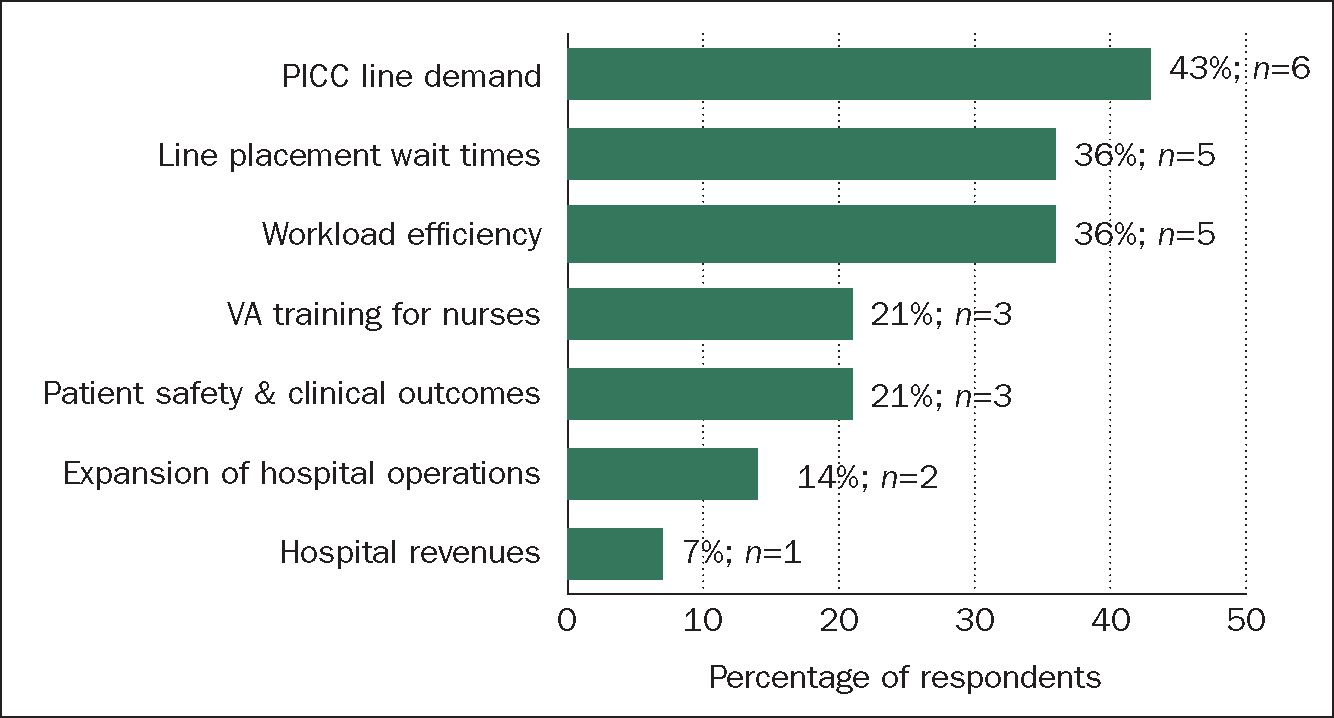
Interviewees provided differing but compelling rationale for VAT formation (Figure 4). The chief drivers of VAT implementation were (i) accommodating increasing VA demand (43%; n=6) or workload (36%; n=5); (ii) reducing VA-related waiting times (36%; n=5); (iii) improving training and clinical outcomes (21%; n=3); (iv) expanding hospital operations (14%; n=2); and (v) revenue considerations (7%, n=1).
‘… all PICC lines were done in interventional radiology. This results in long delay… one other thing that motivated the building of the team was patient safety …’
US2
‘The administration already had the idea, the vision to build a full-time [intravenous (IV)] team. So at the beginning, they already have data [from the US] that shows a full-time IV team can produce more efficiency and also more money’
CH2
Challenges in convincing decision makers emerged as hurdles surrounding VAT formation. Around two-thirds of respondents (57%; n=8) reported using both clinical and cost-based evidence to persuade different stakeholders: published VAT literature and conference materials for convincing physician leaders and economic or efficiency benefits to convince hospital leadership or administration. Three teams either remedied deficient VA training with new coursework or implemented rigorous VA training exercises for nurses to overcome institutional skepticism over nurse proficiency.
‘Before the team was in place, vascular surgeons would place the central lines in the hospital, and they said that PICCs would not work, nurses weren't prepared… I had to break the taboo that nurses couldn't do it, and they tried it in the hospital, and it didn't work, so I had to deal with a strict criteria… and in the end, we could succeed and change the reality in Brazil and expand this experience to other hospitals and start creating VATs’
B3
‘The problem in the beginning was to change the mentality… that nurses can't perform the insertion with a high level of competence’
I1
Subtheme 2. Barriers to VAT impact evaluation
Despite the positive impacts of VATs, participants noted that the lack of baseline data and difficulties with tracking outcomes often pose challenges to demonstrating VAT value. To address these challenges, 3 institutions (Australia, China, and the US) had already created or were in the process of creating a formal database of VAD-related statistics.
‘We maintain a database on all of our PICC lines. We also need to fill out a report if there is a line infection, and it is reviewed by infection prevention control’
A2
Most institutions (64%; n=9) did not have routine mechanisms for recording data on device selection, patient outcomes, and associated costs in pre- or post-VAT periods.
‘I haven't got evidence of that [outcome] being monitored prior to VAT’
UK1
‘No, we haven't formally measured them [outcomes] as such’
A1
Interviewees identified common insufficiencies detrimental to gauging VAT utility, such as time or workload constraints, in conducting follow-ups and data collection.
‘We are not able to review things properly because of the workload. We don't have the time to get around and be a bit proactive about things identified as issues.’
A1
Subtheme 3. Underresearched challenges to disseminating VAT data
All participants (100%; n=14) agreed on the importance of sharing VAT-related data to demonstrate VAT impact. Examples of potential benefits included providing a rationale for new VAT initiatives and justification for existing VAT programs. Interviewees identified time constraints (57%; n=8) and challenges to performing continuous data collection and simplifying data analyses (29%; n=4) as major deterrents to data dissemination.
One US participant identified the shortcomings of the electronic medical record (EMR) systems, underscoring the need for VAT-specific data monitoring:
‘There is such a misunderstanding where people think their EMR is going to provide all the data they need, when they need it, and it is just not accurate … I quickly learned that EMR didn't provide the data points that we needed. So we needed to collect the data ourselves… There is a lack of understanding that data collection and monitoring needs to be a continuous process’
US1
A striking 93% of respondents (n=13) revealed attempting some form of data dissemination activities—active publications in clinical journals, speaking engagements, posters at national or international conferences, and data sharing within or across institutions (Table 2). Several teams used dedicated resources (ie, biomedical researchers, graduate students) to support data collection, analyses, and publication processes.
Table 2. Vascular access team data dissemination methods attempted by respondents
| Data dissemination methods | ||||
|---|---|---|---|---|
| Participant code | Publications reports | Speaker presentations | Conferences | Posters |
| A1 | X | X | X | X |
| A2 | X | X | X | |
| B1 | ○ | X | X | |
| B2 | X | |||
| B3 | ||||
| C1 | ||||
| CH1 | X | X | ||
| CH2 | X | X | X | |
| CO1 | X | X | ||
| I1 | ||||
| S1 | † | X | ○ | X |
| UK1 | † | X | X | X |
| US1 | X | X | ||
| US2 | X | * | X | X |
X=no attempt; =active participation; °=in planning; †=internal data sharing; *=internal presentation.
‘… they [master's students] can do the data collection and analyze all kinds of data for us. We do this together for any research. We don't do this by 1 person, but as 1 team’
CH1
‘My biomedical [professional] collects the data, and every 6 months, I look for the data, and I know how many thrombosis [cases] I have …’
B1
Participants from China, Sweden, and the UK elucidated the positive effects of data sharing and research-related collaborations with other institutions.
‘For the first 5 years, the hospital from USA… they help us to manage this hospital… they already have the VAT. They already understand what is the benefit of this team’
CH2
‘… we usually exchange our protocols and our observational studies. We share that materials with each other [with colleagues in the nearby region]’
S1
‘… we have had numerous new teams looking at forming VAT… have come out and spent time with us to see how we do things… [we] shared some of the documents [protocols] we have used’
UK1
Topical theme. VATs and COVID-19
Teams reported distinctive experiences in terms of workload, staffing, and impacts. The majority (64%; n=9) experienced an increased demand for VAT services, which the participants’ attributed to COVID-19-related surges as the pandemic progressed.
‘I think it [COVID-19] increased the need for the team… patients are more, and also treatments… kind of VAD [demand] become more and more, need to choose more, and do more’
CH1
Participants from Sweden and UK (14%; n=2) noted that adherence to new COVID-19 infection control protocols considerably lengthened VA procedures.
‘We had to deploy more resources on the mobile team. If COVID-positive patients need [VA] then it's done in COVID wards, and we need more people to deploy, more time because of the protection gear and everything. You need more time than usual to put central venous lines for [COVID-19] positive patients’
S1
Discussion
This is the first worldwide multicenter study on VAT initiatives spanning multiple continents. Previous studies either focused on a specific region (ie, Europe)17 or were single-center or single-department analyses,2,15,16,18,19 leading to inadequate global VAT insights. By focusing on underresearched facets of VATs, in this study, we used in-depth interviews to elicit the rationale for establishing VATs, the need for co-initiatives, and to evaluate clinical, efficiency, and patient satisfaction outcomes. In summary, we enunciate the need for VATs, the necessity for recording and quantifying VAT outcomes, and the importance of VA education or training. Repurposing oft-neglected VAT-related data dissemination activities and institutional partnerships into VAT-sustaining activities can transform the VA landscape.
As documented in the literature, the VAT professionals interviewed for this study illustrated diverse team compositions with physicians or nurses.17,19,24,25 However, geographical variations and institutional policies modified the multidisciplinary nature of VATs. For instance, in Brazil, hospital policies prohibited third-party contract physicians from including nurses on VATs, whereas teams in China formed an infusion committee comprised of nurses to audit or monitor VA-related outcomes.
There is not much precedent in the literature examining the varied VAD management responsibilities and division of labor. Differing approaches to teams were evident: respondents from Brazil, UK, and the US noted hierarchically organized teams, while participants from Canada and Australia described specialized VA nurses without clear roles or hierarchy. Two highly structured teams from Brazil and China included nonclinical personnel, such as biomedical researchers or master's students, respectively, for tracking and analyzing data. In this study, we are the first to highlight the importance of including research personnel in VATs. Our findings also reveal that, despite VAT involvement in device insertion, fragmented patient care may persist since only 36% of teams were involved in routine postinsertion VAD management. VATs should consider neutralizing the fragmented nature of VA practice and associated burdens given the overall benefits.15,26,27,2829,30,31
Intriguingly, a participant who heads a physician-only team stated that a multidisciplinary team is better equipped to optimize VA practice. Studies have shown improved clinical outcomes and patient and provider satisfaction when nurses and physicians are involved in collaborative VA training exercises in multiple settings.11,15,19,29,32
Recruitment practices and criteria for VATs have not been described elsewhere in the literature. In this study, we reveal the prioritization of VA-related interest, experience, and skills in the member selection process. In most teams, there were no prerecruitment training mandates; however, all participants emphasized the existence of postrecruitment training programs, supplemented with annual or bi-annual refreshers, certification, and credentialing. The emphasis on training is consistent with the literature: specialized competency training is linked to higher first-attempt success rates of cannulation with ultrasound guidance,15,31,3233 minimized complications (eg, phlebitis),16 and increased patient and provider satisfaction.15,16 These findings offer incentives for investments in robust training infrastructure for VA.
Our results correspond with published literature acknowledging a combination of technology, training, evidence-based protocols, and feedback to guide VA practice.29,34 All participants endorsed evidence-based protocols and VAD selection algorithms known to minimize the complications associated with PICC placements and improve patient safety or outcomes.16,35,36 The importance of specialized VAT training and advanced technology from our study validates previous findings of nearly doubled unsuccessful VAD placement chances (35% increase) by generalist inserters lacking specialized guidance technologies or training.18,33 While in this study we did not evaluate cost savings, the use of advanced technology, ECG, and ultrasound offer proven, quick, cost-effective alternatives to conventional postprocedural chest X-rays.37,38
Workload and time pressures contribute to the limited use of tracking databases and sporadic participation in regular audits, at odds with established standards. Systematic approaches to VAT monitoring via tracking, audits, education, technology, and training have led to impressive declines in complications (ie, CLABSI, pneumothorax).16,39 These findings suggest enhancements toVA practice when VAT programs simultaneously implement training, advanced technology, protocols, and partnerships.
The modest improvements in complication rates reported by the participants cannot be overlooked, considering that recent global CLABSI rates estimated at 5.05 per 1000 central linedays are nearly 6 times greater than the rates reported in the US.40 CLABSIs represent 84,000 to 204,000 infections per year in the US, resulting in up to 25,000 preventable deaths and an estimated cost of $21 billion.41 Previous reports have demonstrated that a trained VAT using evidence-based frameworks can dramatically reduce the incidence of CLABSI by 90%.19,39 Respondents identified evidence-based protocols and member training as key metrics for VAT success; device selection algorithms and postplacement audits had lower rankings, contrary to evidence that algorithms for device selection can minimize incorrect device choice costs and attendant morbidities.42,43 These observations are perhaps attributable to the underestimation of longstanding, stringent hospital procedures to decrease CLABSI rates, and the commonplace nature of VAD selection algorithms may blunt their perceived impacts.
Nearly 64% of our study respondents noted that during the COVID-19 pandemic, overburdened health systems witnessed increased VA demand, and 43% cited device selection and catheter management expertise of VATs in mitigating these challenges. Thus, during a global crisis, dedicated VATs helped alleviate resource and health care constraints, concordant with contemporary literature.17,44,45,46
VAT initiatives improve the clinical and economic outlook for institutions. Embracing recent trends toward patient-centered health care models, in this study, we investigated underreported metrics of VAT impact to supplement traditional clinical and clinico-economic measures, such as patient satisfaction,30,47 which scored highest in post-VAT evaluations. Fewer VAD placement attempts have been shown to reduce patient-reported pain scores, lower complications from multiple venipuncture attempts or delayed treatments, and enhance patient confidence in providers,16,31 reinforcing clinician observations of improved patient satisfaction post-VAT.
Global barriers to the dissemination of VAT-related research need to be tackled; most published data originate from North America with relatively scarce data from other parts of the world.48 There is an unmet need for systematic data tracking and dissemination. Evidence on the need for tracking and sharing VAT-related data is lacking and merits close attention. Participants noted a trifecta of challenges currently surrounding VAT implementation or sustainability: (i) difficulties in convincing stakeholders to form VATs; (ii) barriers to data collection or dissemination; and (iii) diffuse efforts at collaborative research and training partnerships.
Interviewees acknowledged multiple constraints to continuous VAT data collection, analyses, and dissemination: scarcity of time, resources, staffing, and financial considerations. Gaps in data pre- and post-VAT implementation are not conducive for comparisons and pose additional challenges in informing administrative and clinical priorities for VAT implementation.
Despite significant differences in their backgrounds, roles, geographies, and experience levels, the interviewees provided consistent responses regarding VAT composition, co-initiatives, and associated challenges. Most of these agreements are about well-established topics in the literature, which may partially explain the endorsement of multidisciplinary teams,19,41 emphasis on postrecruitment training,32,41 wide use of evidence-based protocols,19,39 as well as device selection algorithms.42,43 These consistencies are not surprising since the published literature likely guided their implementation in a wide range of geographies or institutions. The respondents also agreed on the importance of sharing VAT-related data, which is unlikely to be driven by the literature considering the underresearched nature of this topic. However, it highlights the increasing role of information technologies in shaping health care delivery across the globe.49
Immediate recommendations from this study might address the traditional challenges of VAT implementation and assessment. Mentoring or partnering with other institutions could facilitate a free exchange of ideas, VAT implementation plans, expertise, protocols, and VA tools or co-initiatives. For instance, a hospital in China partnered with a US university hospital for VAT knowledge sharing, training, and technology implementation, and a respondent from the UK reported interinstitutional data sharing for VAT establishment at other hospitals. Data sharing could help circumvent avoidable pitfalls during VAT implementation, and collaborative research could help promote global awareness of VAT impacts. Thus, in this study, we offer a unique window into the importance of collecting, analyzing, and sharing VAT-related data and possible solutions for surmounting obstacles to data dissemination. Authors of studies show that skilled VA professionals can optimize patient-centered health care18,31,33 and impart training and education for bedside nurses to improve clinical outcomes and cost savings.30,31 Thus, collaborative data sharing benefits VA practice and outcomes and could help persuade stakeholders about initiating new VAT services11,32 or sustaining existing teams.11,32
Overall, the insights that we collected from a diverse set of VAT members or leaders offer potential solutions for health care institutions looking to expand or substantiate their VAT operations. In this study, we succeeded in (i) identifying measurable clinical, economic, financial, and patient-oriented VAT endpoints and (ii) discovering how integrating VAT initiatives with institutional and industry alliances helps spread VAT practices, education, research, data sharing, and training.
Study limitations
This study has multiple limitations: first, all interviewees worked at large or urban institutions, which is expected since larger institutions are more likely to establish dedicated teams based on VA demand and available resources. Second, there may be bias from overestimating VAT impacts, as the interviewee selection process was skewed toward stakeholders with VAT experience. Third, underestimation bias may have occurred due to neglecting longstanding clinical outcomes and technology with a lack of comparative insights from non-VAT professionals. Fourth, selection bias may have also played a role in the study findings, as the respondents were chosen using a nonrandom, judgment sampling approach. Fifth, the data gathered from a limited sample of 14 interviewees were qualitative, representing subjective perceptions based on individual and institution-specific experiences. While not fully representative of the views of every clinician on VA across the globe, our limited sample of 14 respondents provides unique, informative perspectives on VATs.
Conclusions
Our respondents, representing perspectives from various geographies, backgrounds, and roles, endorsed the benefits of VATs. The formation of dedicated VATs can lead to significant improvements in patient satisfaction and other clinico-economic outcomes, despite the considerable diversity attendant upon VAT form, function, and responsibilities.
Recommendations for practice
We recommend the formation of multidisciplinary VATs, including dedicated members for collecting and analyzing data on VA-related outcomes. Training and education opportunities, combined with advanced VA technologies, evidence-based protocols, clinical audits, and data collection, can boost VA practice and lead to improved outcomes. Institutional and industry partnerships can facilitate data collection and dissemination efforts that are central to the optimization and sustainability of VAT initiatives across the globe.
Disclosures
SM, ED, and CP report no potential conflicts of interest. KA and SG are employees of BD.


