Insertion of a central venous access device (CVAD) facilitates easy access to a patient's circulation, enables administration of irritant medications, parenteral nutrition, antibiotics, and facilitates frequent bloodwork. Central venous access is also used to deliver lifesaving measures including renal replacement therapy, extracorporeal membrane oxygenation, and rapid delivery of fluids during hypovolemic shock (O'Grady et al, 2011). As such, a CVAD is placed frequently among intensive care unit (ICU) patients. Although they are essential to care, complications such as central line infection and occlusion may develop. These complications may become life threatening and serve to increase morbidity and mortality of ICU patients (Ziegler et al, 2015). Preventing complications associated with central venous access is imperative to ensuring the best possible care for patients experiencing critical illness.
Many interventions to prevent complications, such as central line-associated bloodstream infection (CLABSI), catheter occlusion, and premature removal, have been implemented into ICU standards of care. Examples include the use of catheter insertion bundles and checklists (Lee et al, 2018), hub decontamination, or ‘scrub the hub’ procedures (Caspari et al, 2017), regular dressing changes and flushing (O'Grady et al, 2011), daily chlorhexidine bathing (Shah et al, 2016), quality improvement projects relating to adequate staff training (Coopersmith et al, 2002; Warren et al, 2004), and maintenance of appropriate staffing of units (Holder et al, 2020; Stone et al, 2008). Many modifications to catheters themselves are also available including silver impregnation and antibiotic coating (Lorente et al, 2016). Despite these efforts, CVAD complications remain a problem in the ICU setting. According to the Canadian Nosocomial Infection Surveillance Program, the rate of CLABSI was reported to be 1.2 per 1,000 catheter days in the adult mixed ICU in 2018 (Canadian Nosocomial Infection Surveillance Program1*, 2020). Recent changes to practice caused by the COVID-19 pandemic have been shown to increase rates of CLABSI by as much as 325% (Assi et al, 2021; LeRose et al, 2021).
The use of alternative catheter locking solutions with additional antimicrobial and anticoagulant properties presents an enticing option to clinicians, as a means of complication prevention. Catheter locking is already part of standard catheter maintenance, thus requiring no additional effort from nursing staff. As the catheter lock stays in the internal lumen of the catheter only when the patient is not receiving any medication or fluids, there is no need to worry about incompatibilities. Further, the use of highly concentrated fluids as a lock is possible, as catheter locks are aspirated and do not enter the patient's circulation. These high concentrations may be more effective at killing microorganisms and preventing occlusions, as compared to lower systemic doses (Justo and Bookstaver, 2014).
Although there may be benefits to using alternative catheter locking fluids, the potential for them to make a difference in the adult critical care population is unclear. Due to the high acuity of these patients, CVADs may be in use for the majority of a patient's stay, without the possibility of being locked for a long enough duration for the fluid to be effective.
The purpose of this observational study is to determine the amount of time CVAD lumens in the ICU remain in use versus in a locked state. Baseline rates of CVAD complications potentially modifiable by a change in locking practices were also tracked, although they have previously been well documented in the literature in larger studies. Results of this study will serve to inform the protocol, enrollment timeline, and power calculations of a future randomized controlled trial investigating the effect of 4% tetrasodium ethylenediaminetetraacetic acid (EDTA) as a catheter-locking fluid in the prevention of central line complications in the adult critical care population (NCT04548713).
Materials and methods
Study design
This was a single-centre observational study that utilized a combination of prospective and retrospective data collection techniques.
Setting
The setting of this study included a 30-bed adult intensive care unit (ICU) and high acuity unit (HAU) located in a tertiary care hospital in New Westminster, British Columbia, Canada. The observation period began on December 8, 2020, and ended on January 5, 2021. As there was no intervention in this study, there was no follow-up. (Standard protocol for HAU and ICU CVAD care at this hospital can be provided on request.)
Participants and enrolment
Participants of this study included adult patients (18 years or older), admitted to the ICU or HAU during the observation period and who met inclusion and exclusion criteria. Patients were eligible to be enrolled in the study if they were admitted to the ICU or HAU and had a central venous access device that required locking. This included central venous catheters (CVCs), peripherally inserted central catheters (PICCs), and hemodialysis catheters. Patients were excluded from the study if they had a confirmed or suspected pregnancy, declined to receive blood products, declined to participate, or were currently enrolled in any other research study that could confound outcome measures.
The inclusion and exclusion criteria used for this observational study were the same that will be used in the future randomized controlled trial. The decision to keep the inclusion and exclusion criteria the same was made to determine the enrolment rate during the observational study, to inform the estimated recruitment timelines of the future trial.
Outcome measures and diagnostic criteria
Patient baseline characteristics collected during this study included patient age, sex at birth, APACHE IV score upon admission, any immunodeficiency, and if they had previously experienced a case of CLABSI or CVAD occlusion prior to their enrolment in the study. Information about pre-ICU and ICU length of stay was also collected.
Members of the research team gathered information used to calculate the proportion of time that a patient's CVAD spent in a locked state during the entirety of its ICU lifecycle.
Other outcome measures included incidence rates of CLABSI, catheter colonization, catheter occlusion requiring alteplase use, catheter occlusion requiring replacement, extravasation/local infection/phlebitis at the site of catheter insertion, and catheter-related venous thrombosis.
Diagnostic criteria were based on national guidelines. Reasons for CVAD removal were also tracked and recorded.
Data sources and measurement
Sources of data collection include routine records kept in patient charts, medical imaging records, laboratory results, and microbiology results, as well as results from an in-person data gathering discussion with the nursing staff.
Ethics approval
Permission to conduct this study protocol was provided by the Fraser Health Research Ethics Board. This protocol was also reviewed and approved by the University of British Columbia Clinical Ethics and Simon Fraser University Ethics Boards. As this was not an interventional study, there was no need for informed consent. Study procedures began promptly following ethics and institutional approval.
Data collection
Data collection for this study took place in two parts. First, between December 8, 2020, and January 5, 2021, eligible patients in the ICU were enrolled prospectively by members of the research team according to inclusion and exclusion criteria. Upon enrolment, paper case report forms (CRFs) containing details about patient baseline characteristics, dates of hospital stay, CVAD type, and date of CVAD insertion were completed by reviewing patient charts. Following enrolment, data regarding locking status was obtained through engaging in daily discussions with nursing staff about the status of their patients' CVADs. Data related to central line complications and reasons and dates of removal were collected via a combination of review of patient charts, as well as in-person discussions with nursing staff to gain additional details or clarifications.
Information about whether each catheter lumen in the ICU was in use or locked was collected twice daily (AM shift and PM shift) during the above-mentioned in-person discussions with nurses by the Research Coordinator (JW). The percentage of time each catheter was in a locked state was calculated by determining the percentage of data points recorded as ‘locked’ as compared to the total data points, per catheter and per individual lumen.
The second part of data collection occurred between March 15 and April 9, 2021. This portion of data collection included a retrospective chart review of HAU patients admitted to the unit between December 8, 2020, and January 5, 2021, and the continued follow-up of ICU patients who were transferred to the HAU within that same time period. Due to administrative delays in obtaining relevant ethics board approval to include HAU patients prior to the start of ICU in-person data collection, these data were collected retrospectively and were limited to information found only in patients' charts, without information provided by nursing staff. As such, only data regarding CVAD type, insertion date, removal date, reason for removal, and complications were collected. These were combined with data from the ICU patients enroled previously.
Locking data for the HAU patients were also gathered via retrospective chart review. However, upon assessment of the quality and completeness of data gained prospectively versus retrospectively, we opted not to combine HAU locking data with that obtained from ICU patients. This review process served to inform future data collection procedures for future trials.
The patients were followed by members of the research team until their discharge or end of the observational period, whichever happened first. All CVAD care and maintenance procedures remained the same throughout the observation period. The standard protocol included flushing locked lumens every 12 hours for CVCs and PICCs, and every 48 hours for hemodialysis catheters, as described in the Appendix.
Results
Participants
A total of 75 patients were enrolled in the study during the observation period. All patients who were confirmed eligible completed the study. Data from all 75 patients were included in the analysis. A total of 46 (61.3%) were male. The mean (±SD) age of patients enrolled in our study was 60 (±15) years old, with an APACHE IV score of 112 (±29). The youngest patient was 18 years old, and the oldest was 85.
On average, patients had a pre-ICU/HAU hospital stay of 4 (±12) days (n=29 patients), and an ICU and HAU length of stay of 9 (±10) days. One patient had a pre-ICU hospital stay of 86 days. Of all patients, two (2.7%) had previously experienced CLABSI and CVAD occlusion during their hospital stay. Two patients were immunocompromised (summarized in Table 1).
Table 1. Baseline characteristics of patients enrolled during the observation period in the ICU and HAU population
| Characteristic | Mean ± SD | n (%) |
|---|---|---|
| Age (years) | 60 ± 15 | |
| APACHE IV score | 112 ± 29 | |
| Pre-ICU hospital LOS (days) | 4 ± 12 | |
| ICU LOS (days) | 9 ± 10 | |
| Sex, male | 46 (61.3) | |
| Immunocompromised | 2 (2.7) | |
| Previous CLABSI | 2 (2.7) | |
| Previous CVAD occlusion | 2 (2.7) |
CLABSI=central line-associated bloodstream infection; HAU=high acuity unit; ICU=intensive care unit; LOS=length of stay
Types of CVADs recorded in ICU and HAU patients
A total of 125 CVADs were observed during the study period. Of these, the majority were non-tunneled, triple-lumen catheters, single-lumen hemodialysis lines, and triplelumen PICCs (n=77, 17 and 17, respectively). The next most common type observed was the double-lumen PICC (n=9; summarized in Table 2).
Table 2. Count of CVAD types inserted into patients enrolled during the observation period in the ICU and HAU population
| CVAD type | n=125 |
|---|---|
| Non-tunneled CVC (3 lumen) | 77 |
| Hemodialysis catheter (1 lumen) | 18 |
| PICC (3 lumen) | 17 |
| PICC (2 lumen) | 9 |
| PICC (1 lumen) | 1 |
| Cordis single lumen | 1 |
| 9 French introducer sheath central line | 1 |
| 8.5 French introducer sheath central line | 1 |
CVAD=central venous access device; ICU=intensive care unit; HAU=high acuity unit; PICC=peripherally inserted central catheters
CVAD days and locking data
The average number of days that a CVAD was in place in ICU and HAU patients was 7 (±6) days. The minimum number of days observed was 1 day, and the longest a CVAD was observed to be in place for was for 31 days. The total number of catheter days of CVADs tracked in this study was 871 catheter-days.
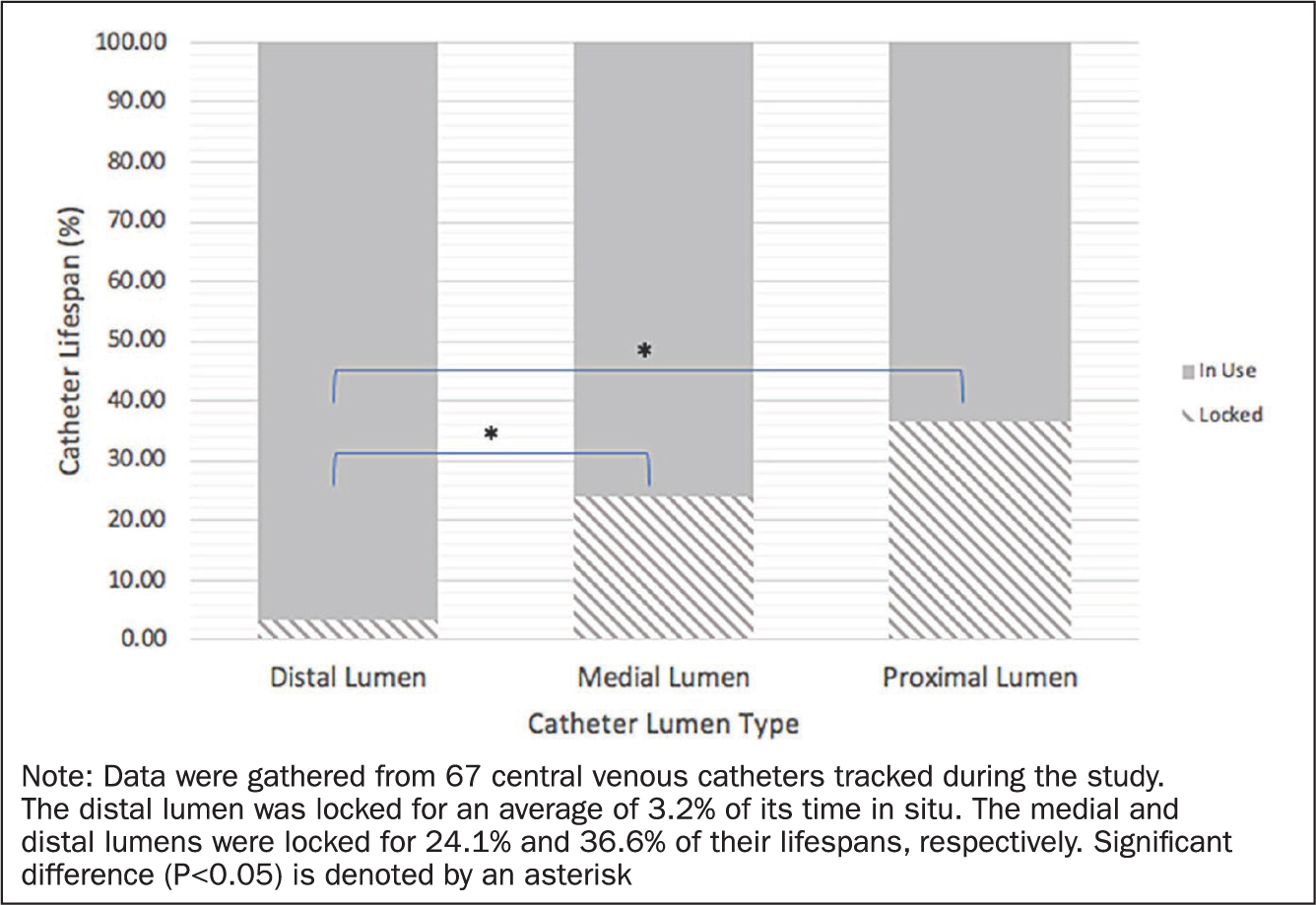
Out of the 77 triple-lumen, non-tunneled catheters tracked, results indicate the medial and proximal lumens were locked for 24.1% and 36.6% of their lifespan, respectively. The distal lumen was found to be locked for an average of 3.2% of its time in situ. A separate analysis was also performed to determine whether there was a difference in percentage of locked time depending on type of lumen (distal, medial, or proximal). Results of a Kruskal-Wallis test showed significant differences in percentage of locked time between lumens (P=0.000). Follow-up post hoc testing, using a Dunn's Multiple Comparisons test, revealed significant differences between the distal and medial (P=0.000), and distal and proximal lumens (P=0.000), but not between medial and proximal lumens (P=0.095). All analyses were performed at alpha=0.05 (see Figure 1).
For all CVADs tracked in ICU patients (including triplelumen catheters, PICCs, and hemodialysis catheters), it was found that each catheter had at least one lumen locked for an average of 22.4% (± 21.0) of its time in situ.
Complication rates
The most common complications recorded during the observation period were CVAD occlusions (23 cases, or 18.4%) and associated alteplase use (also 23 cases, or 18.4%). This equates to an event rate of 26.41 cases per 1,000 catheter days (as shown in Table 3). One CVAD experienced occlusion of all three lumens and was consequently replaced (0.8%, or 1.15 cases per 1,000 catheter days). A catheter-related venous thrombosis was observed in one catheter. With regards to infectious complications, one case of CLABSI and one case of colonization were observed.
Table 3. CVAD complications during the observation period in the ICU and HAU population
| Complication | # Cases | Event rate% | Event rate (per 1,000 catheter days) |
|---|---|---|---|
| Confirmed CLABSI | 1 | 0.8 | 1.2 |
| Occlusion | 23 | 18.4 | 26.4 |
| Replacement due to occlusion | 1 | 0.8 | 1.2 |
| Catheter-related venous thrombosis | 1 | 0.8 | 1.2 |
| Doses of alteplase | 23 | 18.4 | 26.4 |
| Extravasation/local phlebitis | 0 | 0 | 0 |
| Catheter colonization | 1 | 0.8 | 1.2 |
CLABSI=central line-associated bloodstream infection; CVAD=central venous access device; ICU=intensive care unit
The organism that was responsible for the CLABSI case was Staphylococcus epidermidis. This patient was only in the ICU for a few hours for end-of-life care and acquired this infection in their previous unit.
Reasons for CVAD removal
A summary of reasons for CVAD removal can be found in Table 4. Thirty-nine patients were discharged from the ICU with either their CVC or PICC line still in place.
Table 4. Reasons for CVAD removal or loss to follow-up during the observation period in the ICU and HAU population
| Reason for removal | n=125 |
|---|---|
| Removed due to investigation for infection | 10 |
| Removed due to occlusion of all 3 lumens | 1 |
| Removed due to presence of a clot | 1 |
| Change from CVC to PICC for long-term access | 10 |
| Patient left unit with CVAD in place (loss to follow-up) | 42 |
| Reduced clinical need | 3 |
| Patient death | 22 |
| Still in place at study end | 19 |
| Accidentally removed during patient manipulation | 2 |
| Unknown (reasons not listed in HAU patient chart) | 15 |
CVAD=central venous access device; CVC=central venous catheters; HAU=high acuity unit; ICU=intensive care unit; PICC=peripherally inserted central catheters
Aside from patient death, the most common reason for CVAD removal was due to an investigation of an infection. Nine CVADs were observed to be removed for this reason, even though only one was determined to be a confirmed case of CLABSI.
Discussion
Results reveal that at least one lumen of the majority of central lines in the ICU is locked for longer than a third of the total time in situ. This is a much larger proportion of time than initially expected and the first time that this has been reported in the literature, to our knowledge. This is an important finding as it indicates that the lumen of a catheter has a locking solution in situ for a significant proportion of time, allowing it to have a local effect on biofilm and thrombus production. This emphasizes the importance of using effective CVAD locking solutions and performing appropriate clinical testing powered to detect differences in complication rates (Pérez-Granda et al, 2014; Souweine et al, 2015; Quenot et al, 2019).
These baseline rates of CVAD complications during this observation period are comparable to the incidence rates in Canada previously reported in the literature (Canadian Nosocomial Infection Surveillance Program1*, 2020). With regards to global comparisons rates, a 2018 meta-analysis by Takashima et al (2018) revealed the incidence rates for CLABSI to be 4.59 per 1,000 catheter days. The results of this study put the pooled percentage of occlusion or blockage of the catheter at 11%, which is lower than the 18.4% observed in our study (Takashima et al, 2018). This large meta-analysis compiled the outcomes of more than 50,000 CVADs and 396,951 catheter days in 63 international studies, which can help explain discrepancies with our own results. Occlusion rates at our centre also were found to be higher than those reported by Takashima et al (2018). This may be due to nursing culture at our unit, to lock central line catheters when not in use, as compared to other units where the standard may be to keep all catheter lumens open with patency maintenance fluid infusion. Although potentially appealing as a method to reduce CVAD complication rates, ongoing additional fluid administration has well recognized consequences. Even a low amount of fluid administration can accumulate over a long period of time and lead to fluid overload, which has been shown to be positively associated with increased complications and mortality (Gillespie et al, 2004; Bouchard et al, 2009; Claure-Del Granado and Mehta, 2016).
Results of baseline characteristics of patients enrolled in this study are representative of the typical ICU patient. These baseline characteristics were of interest to us, as previous literature has shown them to be related to the development of CVAD complications (van Rooden et al, 2005; Baskin et al, 2009; Hermite et al, 2012; Lissauer et al, 2012).
One interesting observation made during the study was the presence of a few patients who contributed multiple incidents to the complication count. One patient experienced six occlusions that were resolved with six doses of alteplase to one of their CVADs. Similarly, another patient experienced three CVAD occlusions, required four doses of alteplase, and one colonization incident in one of their CVADs. This patient then experienced a subsequent five occlusions that were resolved with six doses of alteplase in the next CVAD they had inserted during their ICU stay. The medical charts of these patients warrant further investigation for the identification of potential risk factors that could have contributed to their high complication rates. These cases also provide evidence to support the notion that CVAD infections and occlusions are related, and that the development of one of these complications increases the risk for the development of another (Timsit et al, 1998; Ryder, 2005; Baskin et al, 2009). Ideally, locking interventions aimed at preventing the development of catheter complications should possess antimicrobial, antibiofilm, and either anticoagulant or antithrombotic properties.
Examples of alternative locking solutions studied to date include ethanol, taurolidine, various antibiotics, and ethylenediaminetetraacetic acid (EDTA). Efficacy of these alternatives has been compared to current standard of care saline, heparin, and citrate. Although potentially protective, benefits must be weighed against risks of use. For example, ethanol has been shown to damage industry standard polyurethane and silicone catheters (Mermel and Alang, 2014), stimulate S. aureus and S. epidermidis biofilm formation (Redelman et al, 2012; Luther et al, 2015), and cause adverse events (Pérez-Granda et al, 2014; Wolf et al, 2018) in patients. In terms of risks to the global healthcare system, use of antibiotic locks has been discouraged with the emergence of antibiotic-resistant bacteria and subsequent shift toward antibiotic stewardship initiatives (Laxminarayan et al, 2013). Further, many of the locking fluid alternatives studied are effective at preventing only certain avenues of complication. For example, while taurolidine has been shown to be effective in eradicating gram-negative bacteria (Liu et al, 2013), complications may still arise due to gram-positive infection. Additionally, ethanol, antibiotic, and taurolidine locks lack significant antithrombotic or anticoagulant activity.
In contrast, chemical chelators, such as EDTA, exhibit potent antimicrobial, antibiofilm, and anticoagulant properties (Percival and Salisbury, 2017). Although promising for use as a locking fluid in the critical care setting, evidence for its efficacy in the literature is limited to a few randomized controlled trials in other patient populations (Campos et al, 2011; Ferreira Chacon et al, 2011; Kanaa et al, 2015; Luiz et al, 2017; Rijnders et al, 2019) and in vivo analysis (Liu et al, 2018), highlighting the need for further investigation and premise for our future trial.
Another important finding of this study includes that one of the most common reasons for CVAD removal in the ICU is due to suspicion of a potential infection. This reflects standard practice in the ICU to remove all lines out of an abundance of caution when the patient begins showing signs of unexplained infection. The majority of CVADs removed for this reason were either not sent for microbiological testing, or not found to be the cause of infection. Although protective for the patient, this results in added utilization of healthcare resources and cost to the system (Pearse et al, 2021). The use of alternative locking solutions could potentially reduce the number of CVADs replaced unnecessarily by reducing the probability of the CVAD causing an infection.
Limitations
The significant limitation of this study includes the lack of quality locking data for part of the study population. Due to the reduced acuity of HAU patients, it is likely that rates of CVAD locking are higher in this unit, contributing further cause for the usefulness of a locking intervention.
Further, this study was performed only at a single centre. This limits generalizability, and is reflective only of nursing culture at our site. Nevertheless, we feel patients and standard CVAD care procedures at our centre are consistent with international guidelines and may be representative of many ICUs. Due to the limited generalizability and level of evidence of this study, results should be interpreted as descriptive and hypothesis-generating only.
Another limitation of the study includes not systematically investigating each CVAD for presence of colonization following removal. According to standard practice at our unit, CVADs in the ICU are only removed for testing at the discretion of the treating physician based on patients' infection symptomatology. As such, it is likely that the true rate of CVAD colonization was under-represented by the results of this study. However, as this is standard practice in most ICUs, the rate of catheter colonization was still in line with previously published literature (Takashima et al, 2018).
Lastly, a limitation of this study includes potential bias caused by nurses being unblinded to study procedures and subsequent effect on the CVAD complication rate. As the in-person data component was essential to gathering important information about CVAD locking status, there was no way to prevent this unblinding.
Conclusions
Although the results from this study should be generalized with caution, it is a reasonable assumption that duration of CVAD lumen locking is under-utilized as a tool to help protect against CVAD complications. The critical care population is a good candidate for investigations of alternative locking fluids due to adequate exposure to the locking intervention and high rates of CVAD occlusions potentially modifiable by locking practices. Prevention of CVAD complications in this population is essential to reduce morbidity and mortality and improve patient outcomes.


