Despite advances in treatments and improvements in clinical outcomes, HIV remains an under-recognised disease (British HIV Association (BHIVA), 2018). Although HIV is now considered a long-term illness, the stigma associated with the disease results in patients being reluctant to engage with services, which ultimately affects their overall health and wellbeing (Croston et al, 2022). The role of a community HIV specialist nurse (CHSN) is often a misunderstood and complex one. The role includes supporting a caseload of people living with HIV, who are underserved by other healthcare services for various reasons, such as:
- Having very complex health issues
- Non-engagement with services
- Being unable to access services due to physical and/or mental health complications (Watson et al, 2018).
The spectrum of illnesses seen in people living with HIV has widened. Due to an increasingly ageing population cohort living with HIV, requiring a longer duration of treatment, the HIV-associated pathology and health outcomes have changed. The changes include non-HIV comorbidity health concerns such as neurological, cardiac and oncological health issues (BHIVA, 2018). The need for robust multidisciplinary working is essential not only in providing care for people living with HIV (BHIVA, 2018), it is also the most effective way to address their complex needs (Campbell et al, 2022). The CHSN is in a unique position to co-ordinate such care, particularly for patients who are hard to reach (Watson et al, 2018).
Multidisciplinary working is seen as an essential part of providing high-quality HIV care (BHIVA, 2018) Despite this, little research has been undertaken to quantify to what extent community HIV specialist services (CHSS) teams facilitate multidisciplinary working and support people living with HIV to access appropriate services. The study reported in this article aimed to demonstrate this, by auditing the number and type of referrals completed by the community HIV team. It is hoped that the results will help CHSSs in developing their services to meet the changing needs of people living with HIV, especially hard-to-reach patients seen within the CHSS. The author's CHSS team includes community nurse specialists, clinical team nurse leaders, a clinical nursing lead, a lead psychologist and administration staff.
Methodology
Due to the large geographical area, 30 eligible patients were selected from the West Sussex, Brighton and Hove area using the following inclusion/exclusion criteria:
Inclusion criteria
All patients identified needed to be actively receiving care from the team to ensure the auditor had access to all documentation on the computer system.
Exclusion criteria
Patients referred for short-term interventions such as HIV-related blood tests and venepuncture were excluded because they are not routinely offered a full assessment by the nurses, as their care is case managed by acute services.
Audit
Once the patient cohort was identified, a retrospective audit of their notes was completed by a single researcher applying the data system used by the local CHSN teams.
Because this research was carried out over multiple trusts, referrals were made in different ways, so the following areas were reviewed to ensure all types of referrals were identified:
- Referrals to other services and health professionals
- Contact with other professionals
- CHSN assessments: plans and referrals
- Record attachments
- Care plans
- Notes concerning communications with patients and other services and copies of letters.
Data collection
Data collection was carried out by a single researcher. Microsoft Excel was used for data storage; this was updated when referrals to other services were found within the identified documentation. Initially, all referrals were documented separately; later, the researcher decided to combine referrals to services that had a common theme to simplify the research. These were grouped into relevant data sets such as ‘GPs’, ‘social services’ and ‘HIV peer groups’ to be further analysed. The aim of this audit was to identify the types of referrals made, therefore no further statistical analysis was performed.
Results
A total of 154 referrals was made by the CHSNs, with a range of between 1 and 12 per patient and an average of 5 per patient. Figure 1 provides an overview of the type of services to which patients were referred, which included:
- HIV community charities: these provide services such as advocacy, HIV advice, emotional support, and practical advice with matters, such as financial and benefits issues
- HIV specialist care and support charities: charities that provide both specialist HIV care via inpatient units for those patients requiring admission, as well as day-care services and peer support
- Non-HIV charities: these included charities that support those affected by domestic abuse, sexual abuse, substance misuse, and provide support for refugees and vulnerable migrants.
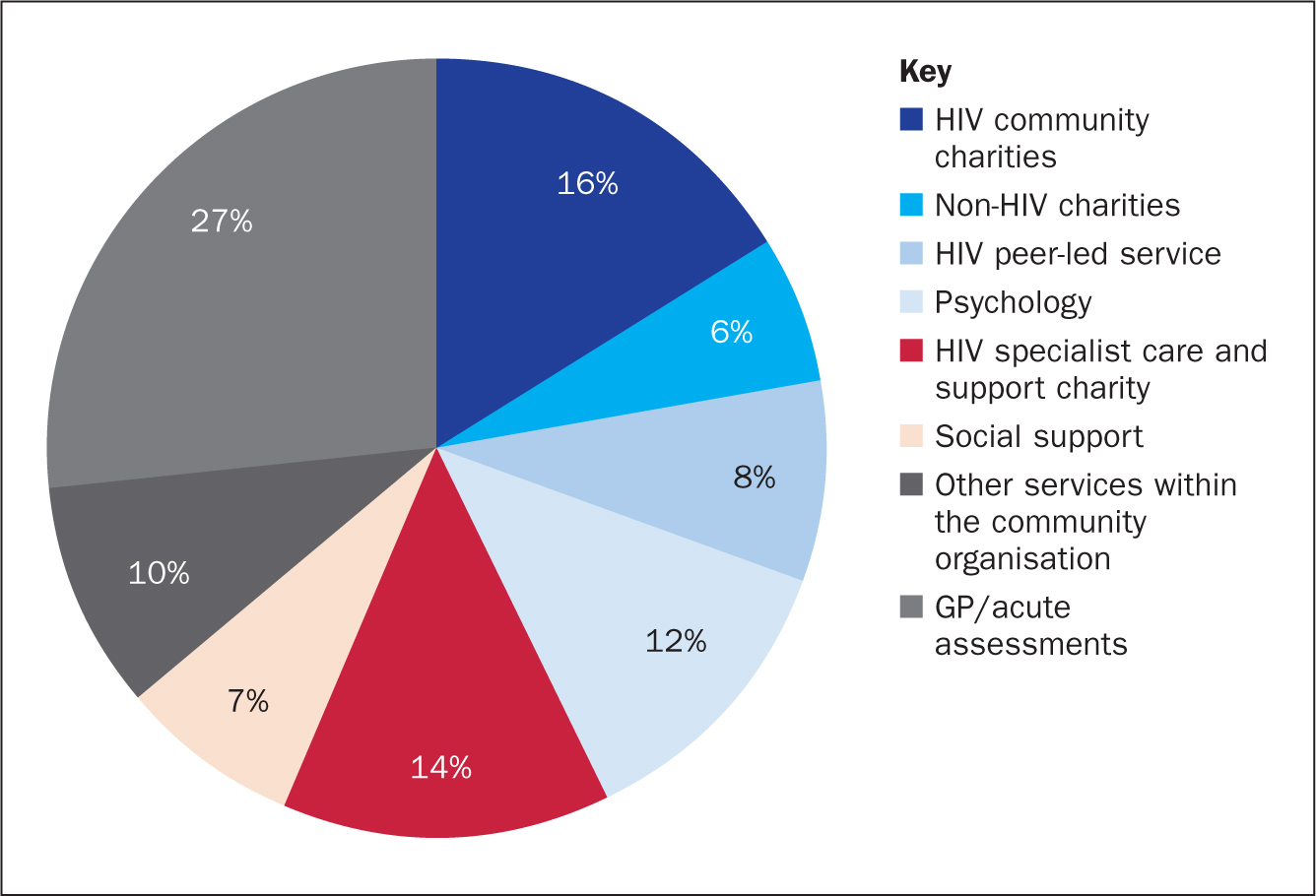
As mentioned previously, people living with HIV are increasingly being impacted by other non-HIV conditions as they age (BHIVA, 2018). Fifty-four per cent of the referrals made by the CHSS team were non-HIV related, which shows that the majority of assessments and inter-professional work being undertaken by this community HIV team is related to a large number of non-HIV-specific issues. This illustrates the diversity and complexity of patients seen within the services. It also supports the possibility that the patients seen within the community HIV service have challenges accessing, and are underserved by, generic services for the reasons previously mentioned. This further highlights the importance of the CHSN meeting patients' multiple care needs of and ensuring that an equitable standard of care is delivered to people living with HIV across all healthcare and social care settings (BHIVA, 2018).
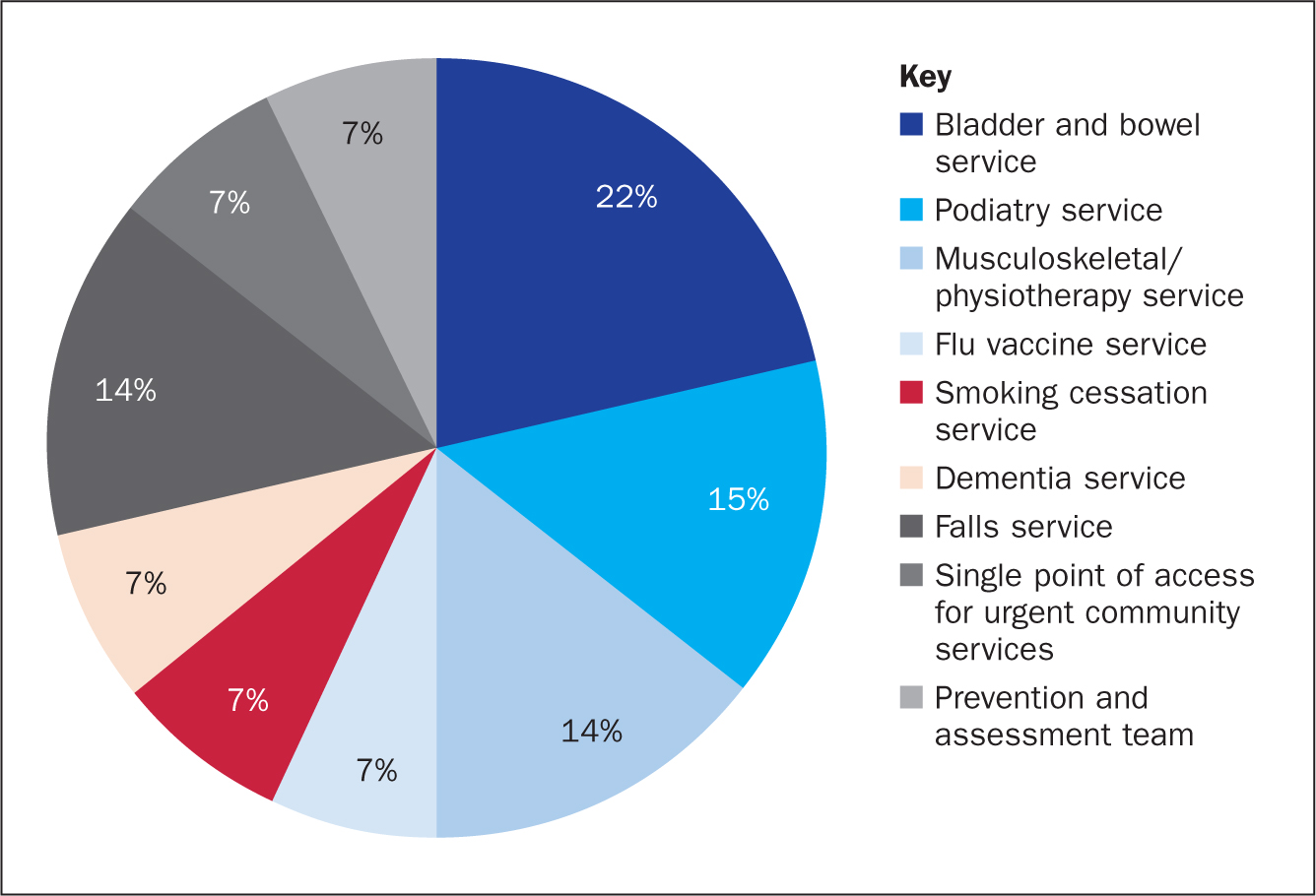
A total of 53 referrals were made to other services within the NHS community trust and to GPs and other acute services. Figure 2 shows the types of referrals made by the CHSS as a direct result of the holistic assessments carried out by the team. The organisations to which patients were referred included:
- Prevention and assessment team: a service that focuses on prevention of admissions to hospital
- Single points of access for urgent community services: these include access to rapid assessment teams, paramedics, dementia beds and access to community beds within the geographical area
- Musculoskeletal/physiotherapy services.
As part of the CHSN initial assessment, a holistic patient assessment is carried out, including a review and assessment of physical and mental health. As a result, GP and acute assessment referrals (Figure 1) make up the largest percentage (27%) of overall referrals, which not only demonstrates the value of carrying out such assessments, but also the importance of the CHSS. By the nature of the community service and referral criteria, the majority of the caseload consists of hard-to-reach patients, such as those who struggle to access and engage with services. Having input by the CHSS not only enables patients to have thorough assessments, but also to access other services by way of appropriate onward referrals, neither of which they may have accessed without the CHSS (Figure 3).
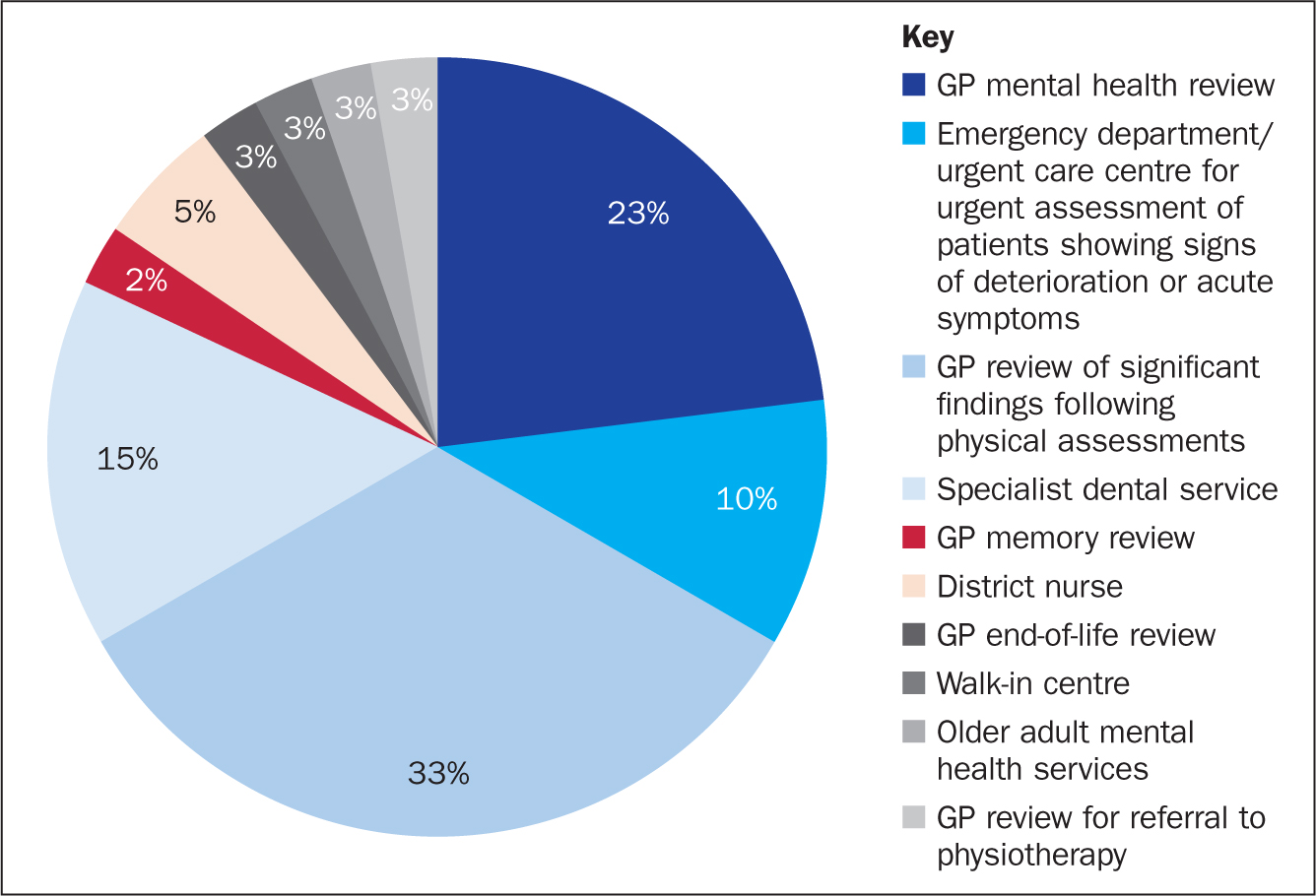
As well as physical health, generic mental health assessments are carried out during the health assessment. People living with HIV are at higher risk of developing psychological difficulties than the general population (Figure 4). There are direct links between improving a person's mental health and its positive impact on physical health and reducing risks of HIV transmission (BHIVA, 2011), meaning that adequate assessments and treatments are essential. The need for such assessments and access to services is reflected in the fact that 23% of the GP/acute referrals were for mental health reviews, namely medication reviews and the need for further assessments. In addition, the CHSS nurses directly referred patients to psychologists (Figure 1 and Figure 4). Based on the assessment and discussion with the team's psychologist, if a patient's presenting complaints were linked directly to their HIV diagnosis, then these referrals were made to an HIV-related psychologist. Alternatively, they were referred to a non-HIV-related psychologist, based on their needs (Figure 4).
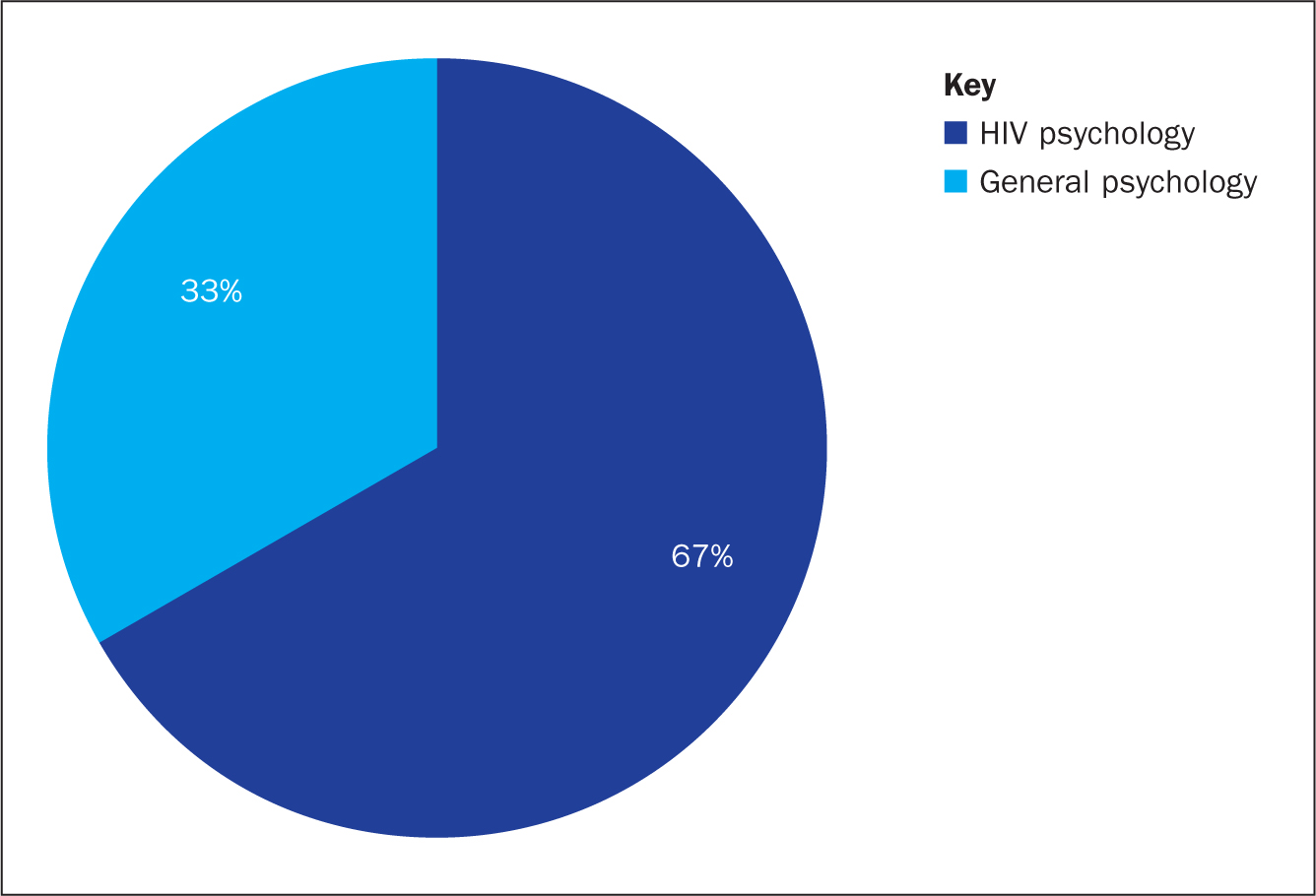
Overall, onward referrals as a result of mental health concerns accounted for 19% of the total patient cohort (n=154) (including GP mental health reviews and psychology referrals). This shows the importance of having robust pathways between HIV care and mental health teams, ensuring that people living with HIV have access to such services.
Limitations and strengths of the study
Due to the workload within the service, the audit was carried out by one researcher. To limit data input errors, the patient record and data entry were checked twice to ensure accurate data were collected. However, because the data collection was done by a single researcher, this allowed for consistency in the identification of referrals, adding to its validity.
The audit was conducted within a geographical area that is linked to large HIV clinics and local acute services. This is not the case throughout the UK, so the transferability of findings may be an issue because it does not represent the services available to all people living with HIV in the UK.
Discussion
Although this is an HIV specialist service, the majority of onward referrals made by the CHSS were in fact non-HIV related. This approach supports the changing needs of HIV patients, advancements in treatments and an ageing population. This audit has shown not only the importance of the need to continue to develop HIV services to cater for this changing population, but also the importance of the CHSS in supporting all patients and especially those who are hard to reach.
The solution for these hard-to-reach patients is not to simply hand them over to generic services. In fact, a large proportion of CHSS work is to support them to engage in care and with the services, long after the referral has been made. The CHSS in this audit are within a well-supported geographical area with links to various HIV and acute services; this may not be the case in other regions.
Based on the findings of this audit, more research is needed to explore the needs of hard-to-reach groups in a wider geographical area.
Conclusion
As a result of undertaking this audit, it is the author's opinion that a potential improvement in HIV care could be to invest in CHSS teams, ensuring all practitioners have access to advanced nursing qualifications, not only in HIV-related but also non-HIV-related conditions. These would include the areas highlighted such as advanced physical assessments and drug and alcohol dependency. The audit also highlighted the large number of mental health-related referrals, suggesting that additional areas of development are required, for example staff mental health training, the incorporation of mental health professionals as part of the community HIV team and the formulation of robust pathways to mental health support.
These solutions and potential developments would not only increase the practitioners' knowledge but would also enable them to meet the complex needs of the patients seen within the service, because CHSSs are often the key care providers for hard-to-reach patients. This will help achieve the ultimate goal – that all people living with HIV will receive care that is as high quality as that provided to those not living with HIV, regardless of their circumstances.
KEY POINTS
- Due to the advancement of treatments, the spectrum of needs for people living with HIV is changing, resulting in the need for robust multidisciplinary working
- Care provided by community specialist HIV services includes a wide range of non-HIV-related physical and mental health care due to the changing needs of people living with HIV
- Holistic assessments of patients that include both physical and mental reviews are vital for individuals with complex conditions to ensure that their care needs are met and that appropriate services are accessed to improve overall physical and mental health outcomes
- Community teams are integral to co-ordinating care for hard-to-reach patients, ensuring the delivery of an equitable standard of care for those living with HIV
CPD reflective questions
- In what way does multidisciplinary working improve care for patients in your own practice? Can you think of any improvements that could be made?
- How do holistic assessments help identify the care needs of patients? How could you incorporate this approach within your practice?
- How can services be developed to ensure the provision of equitable care for people living with HIV in wider geographical areas?


