The global COVID-19 pandemic changed healthcare delivery on an unforeseen global level. With the pandemic came the need for extended and prolonged use of personal protective equipment (PPE) by health professionals. This increased use lead to reports on social media and in the news noting an increase in skin issues among health professionals. Galanis et al (2021) conducted a systematic review focusing on the physical risk and impact of prolonged PPE use on health professionals during COVID-19 and estimated the prevalence of skin issues among this group to be 78%.
Since the onset of enhanced infection control measures for COVID-19, including prolonged use of PPE, several skin conditions related to the use of PPE and frequent skin cleansing among health professionals have been reported, including pressure injuries, contact dermatitis, and pruritis (Darlenski and Tsankov, 2020). Despite numerous personal and media reports by health professionals of PPE-related skin injuries, there are few publications to date in the healthcare literature describing the prevalence of these injuries (Alves et al, 2020). It has been reported that an increased duration of PPE use can be associated with skin irritation and breakdown (Darlenski and Tsankov, 2020).
A recent survey of 542 healthcare workers in Bulgaria reported common PPE-related symptoms including burning, itching, stinging, erythema, papules, maceration and scaling, 97% of which have been associated with the prolonged use of PPE (Darlenski and Tsankov, 2020). The most common areas where problems occurred were found to be the nasal bridge, cheeks, forehead and hands. Dermatitis of the hands has been reported to be linked to long-term glove use occluding the skin and causing a moisture imbalance; coupled with excessive hand cleansing, irritation, maceration, erosion and dermatitis become possible (Darlenski and Tsankov, 2020).
PPE-related skin injuries are frequently seen as mild irritations and it is believed that they are often overlooked or minimised. It must be noted that even small skin irritations may increase the risk to health professionals as skin irritation may predispose many to inadvertently touch their face (when not wearing a PPE) and break PPE protocol unconsciously (Kantor, 2020). During the 2003 severe acute respiratory syndrome (SARS) outbreak, a study in an acute care hospital in Singapore (n=109) reported staff experienced acne (59.6%), facial itch (51.4%), and rash (35.8%) from regular N95 mask use. In addition, staff reported dry skin (73.4%), itch (56.3%), and rash (37.5%) related to prolonged glove usage (Foo et al, 2006).
It has been hypothesised that skin damage under a medical face mask can be a portal for the coronavirus to enter the body. It will also allow other hospital-acquired bacterial, viral or fungal infections to take hold (Gefen, 2020). PPE-related skin conditions include, but are not limited to, dermatitis, eczema and infections. Breaks in a health professional's hand skin integrity can increase the risk of breaching infection control policy (itching and premature removal of PPE), and can lead to a decrease in work productivity and absence from work (Public Health Ontario, 2016).
Aim
The purpose of this cross-sectional study was to explore the impact that prolonged PPE use has on the skin integrity of Canadian health professionals. The two research questions posed were:
- What is the prevalence of PPE-related skin injuries among Canadian health professionals?
- What types of PPE-related skin injury are Canadian health professionals experiencing?
Methods
A descriptive, pan-Canadian, cross-sectional, self-administered online survey was carried out between October 2020 and April 2021 to explore the type and prevalence of PPE-related skin injury among Canadian health professionals. A convenience sampling method was used to disseminate the online survey link to health professionals via their provincial or national associations. As participants were invited by their provincial or national associations, a refusal rate cannot be calculated. The research team at no time had access to the names and email contact lists of potential participants. Confidentiality and anonymity were guaranteed. The surveys were completed online and directly downloaded to the Fluid survey server. Fluid survey removed all identifiers (email addresses) from the responses prior to downloading data by the research team. Ethical approval was obtained from the Queen's Health Sciences Research Ethics Board (TRAQ # 6031555). The survey was available in English and in French.
Data collection and measurement tools
Two nurses specialised in wound, ostomy and continence (NSWOCs) and a physician designed a questionnaire, which contained 23 survey questions, including four demographic questions, aimed at exploring the impact that PPE use has on skin integrity among Canadian health professionals. A sample group of 10 NSWOCs assessed the survey for flow, ease of use and time for completion in order to determine face validity. In addition, five NSWOCs reviewed the survey for content validity and appropriateness of questions prior to the study onset. Revisions of the survey were made based on feedback from these groups. The revised survey was then translated into French.
Sample
A confidence interval of 95% (z=1.96) and an allowable margin of error of ± 5% (d= 0.05) were chosen for sample size calculation. Based on a population of approximately 500 000 nurses and physicians in Canada, the required sample size to adequately power the study was 384 participants.
Statistical analysis
The data were analysed using SPSS version 25 for Mac. Descriptive statistics, frequencies and percentages were generated to provide information on the type and prevalence of PPE-related skin injury among Canadian health professionals.
Results
The online survey was completed by 757 health professionals and 740 individuals completed the question related to professional designation. The majority, 59% (n=433) were registered nurses followed by 13% (n=99) medical doctors (Table 1). Respondents were from across the continuum of care, with the largest group 27% (n=207) from acute care hospital units (Table 2). The majority of respondents, 86% (n=650), were female, 11% (n=87) male, 2 respondents were non-binary, 7 chose not to declare and 11 did not answer. As participants were invited by their provincial or national associations, it is not known how many health professionals received the survey and therefore a refusal rate cannot be calculated.
Table 1. Professional designation of survey respondents
| Designation | Frequency | % | Valid % |
|---|---|---|---|
| Registered nurse | 433 | 57.2 | 58.5 |
| Medical doctor | 99 | 13.1 | 13.4 |
| Other health professional | 72 | 9.5 | 9.7 |
| RPN/LPN | 59 | 7.8 | 8.0 |
| Occupational therapist | 30 | 4.0 | 4.1 |
| Physiotherapist | 26 | 3.4 | 3.5 |
| PSW | 13 | 1.7 | 1.8 |
| Nurse practitioner | 8 | 1.1 | 1.1 |
| Total | 740 | 97.8 | 100.0 |
| Missing | 17 | 2.2 | |
| Total | 757 | 100.0 |
PSW = Personal support worker; RPN/LPN = Registered practical nurse/Licensed practical nurse
Table 2. Survey respondents' professional settings
| Healthcare setting | Frequency | % | Valid % |
|---|---|---|---|
| Acute care hospital unit | 207 | 27.3 | 27.8 |
| Emergency department | 144 | 19.0 | 19.4 |
| Other | 89 | 11.8 | 12.0 |
| Outpatient | 67 | 8.9 | 9.0 |
| Long-term care | 64 | 8.5 | 8.6 |
| Home care | 61 | 8.1 | 8.2 |
| Critical care | 37 | 4.9 | 5.0 |
| Primary care | 29 | 3.8 | 3.9 |
| Rehabilitation | 24 | 3.2 | 3.2 |
| Operating room | 7 | 0.9 | 0.9 |
| Complex continuing care | 6 | 0.8 | 0.8 |
| Hospice | 5 | 0.7 | 0.7 |
| Retirement home | 4 | 0.5 | 0.5 |
| Total | 744 | 98.3 | 100.0 |
| Missing | 13 | 1.7 | |
| Total | 757 | 100.0 |
The majority of respondents (89%; n=670) primarily wore surgical masks, 7% (n=54) reported wearing a combination of surgical or N95/KN95 respirator masks (it should be noted that in other regions, such as the UK, the equivalent mask is an FFP2) and only 3% (n=20) stated that they wore N95/KN95 respirator masks alone. In all, 85% (n=641) reported always wearing a mask while at work. Of those, 61% (n=394) indicated that they change their masks 2–3 times per 8–12-hour period and 39% (n=247) stated that they wear the same mask all shift and only remove at the end of the shift.
Protective eyewear – either goggles, full face shield/visor or a combination of both goggles and face shield/visors – were reported to be used by 90% (n=681) of respondents, whereas 10% (n=73) indicated that they did not wear protective eye wear. Of those who wore protective eyewear, 26% (n=175) only wore the protective face covering when the situation warranted its use, 24% (n=164) used the protection for each patient encounter with removal after the encounter, 41% (n=277) always wore the protection except during breaks and 8% (n=56) only removed the face protection at the end of their shift.
Respondents reported issues related to mask and/or face protector/goggle use. These included soreness/pressure injuries behind the ears for 70% (n=527) of respondents, 52% (n=395) reported new or worsening acne, 45% had a runny nose or sneezing, 39% (n=299) reported itch (face, eyelids, lips) and dry skin in 37% (n=279) of respondents (Table 3).
Table 3. Issues related to mask and/or face protection use
| Issue | Frequency | % |
|---|---|---|
| Soreness/pressure injury behind the ears | 527 | 70 |
| Acne (new or worsening) | 395 | 52 |
| Runny nose/sneezing | 344 | 45 |
| Itch (face, eyelids, lips) | 299 | 39 |
| Dry skin | 279 | 37 |
| Red skin | 273 | 36 |
| Sore skin | 236 | 31 |
| Rash | 160 | 21 |
| Increased pore size | 158 | 21 |
| Problem with breathing, shortness of breath, tightness of chest | 146 | 19 |
| Feeling claustrophobic when wearing personal protective equipment | 131 | 17 |
| Moisture-associated skin damage | 49 | 6 |
| Panic attack | 31 | 4 |
Note: Respondents selected all that applied
Respondents indicated that since the pandemic, medical glove usage and hand cleansing increased. Hand care was almost evenly mixed with 51% (n=390) reporting never or occasionally moisturising their hands, compared to 49% (n=367) moisturising their hands at least once per day. Respondents reported issues related to medical glove usage. The top reported glove-related issues were dry skin (53%; n=404), red skin (30%; n=224), itch (26%; n=200), broken skin (20%; n=155), rash (16%; n=118) and dermatitis (11%; n=83) (Table 4).
Table 4. Issues related to glove use
| Issue | Frequency | % |
|---|---|---|
| Dry skin | 404 | 53 |
| Red skin | 224 | 30 |
| Itch | 200 | 26 |
| Broken skin | 155 | 20 |
| Rash | 118 | 16 |
| Dermatitis | 83 | 11 |
Note: Respondents selected all that applied
In relation to the use of either disposable or reusable protective gowns by health professionals, 58% (n=439) occasionally wore gowns as required, 22% (n=163) wore gowns for each patient encounter and 20% (n=155) did not wear protective gowns. Considering problems related to gowns, 6% (n=42) indicated experiencing itching while wearing a gown, 5% (n=38) reported moisture-associated skin damage, 4% (n=31) stated they felt claustrophobic when wearing a gown and 3% (n=22) reported new or worsening acne (not located on the face); 87% (n=662) experienced increased perspiration while wearing protective equipment.
In terms of help-seeking behaviour, 15% (n=114) of respondents sought assistance for PPE-related issues from the internet, family/friends or self-help resources, 5% (n=40) consulted with occupational health, 2% (n=8) visited their primary care provider, 2% (n=7) sought support from a dermatologist and 2% (n=7) requested support from an NSWOC. Some 43% (n=322) of respondents reported that their mental health has become worse in relation to wearing PPE for a prolonged period of time.
Discussion
The results of this study demonstrate the impact that prolonged use of PPE has on Canadian health professionals, over a variety of healthcare settings. During the COVID-19 pandemic, health professionals have been subjected to not only the emotional strain of harsh work environments but also the physical strain. The use of PPE greatly increased as part of measures to reduce coronavirus transmission, and the situation has been further complicated by global shortages of PPE. The prolonged use of the equipment as a result has contributed to health professionals suffering while still trying to maintain patient safety and comfort. This study explored 757 health professionals and their experience wearing PPE such as masks, face protection, gloves and gowns. Although prolonged use of the equipment was necessary due to depleted resources, the longer duration of wearing the equipment contributes to increased PPE-related injury (Yan et al, 2020). Evaluating the results of this study provides the opportunity to explore how interventions can be implemented to prevent skin injury within the current situation, and future situations, of PPE shortages.
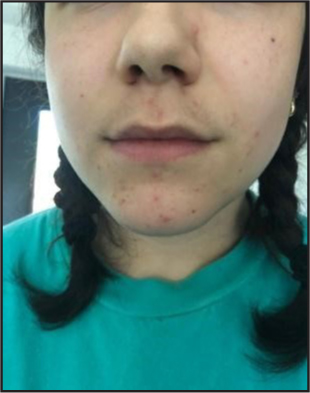
At the time of survey release, health professionals in Canada were predominantly wearing surgical masks and changing them 2–3 times per 8–12-hour period. It is recommended that surgical masks be changed as soon as they are wet or at most every 4 hours to maintain skin integrity and mask efficacy (Lepelletier et al, 2020). Health professionals reported adverse effects such as acne (Figure 1), overall itchiness and dry skin, and soreness behind the ears related to the use of masks or face protection. Additional mention of excessive heat and moisture being trapped within the mask, as well as infrequent changing of masks, are likely to increase bacteria growth on the skin and contribute to the aforementioned skin issues (Wan et al, 2022). Peko et al (2021) reported an increased skin temperature associated with surgical masks in comparison with N95 masks. This is suspected to be due to a lower volume of free air underneath the mask, which prevents skin heat loss. Larger points of contact such as the nasal bridge, chin, and cheeks were considered at greater risk for irritation due to temperature increase as well.
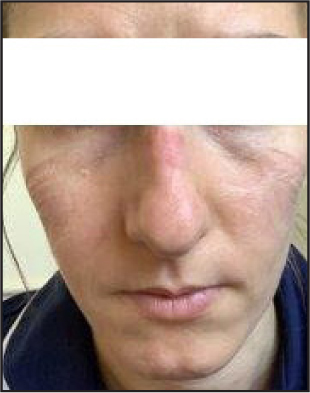
More frequent adverse effects are associated with wearing N95/K95 respirator masks in comparison with surgical masks (Verberne et al, 2021). In contrast to surgical masks, N95 masks require individual fitting to ensure proper use. If the respirator masks are ill-fitting, they are not only rendered less effective but also pose a risk for skin injury such as pressure injuries (Figure 2andFigure 3). Due to mass shortage of respirator fitted masks, healthcare workers during the COVID-19 pandemic were forced to wear ill-fitted masks. Verberne et al (2021) found that skin injuries associated with N95 use was more prevalent in females due to limited models suitable for them. They found that N95 models were typically made for male faces which has resulted in limited models for females. As of 2018, Statistics Canada (2021) reported that over 78.8% of healthcare workers were female. Therefore, with women making up such a large proportion of the medical field, more research and work should be put into developing PPE specific to the female population. In the current study, 85.9% of respondents were women, in keeping with the fact that the majority of healthcare workers are women. More research is required to determine if women health professionals in Canada develop a greater proportion of PPE-related skin injuries.

A position paper released by the National Pressure Injury Advisory Panel (NPIAP) (2020) describes various techniques to be implemented regarding prevention of skin injury from facial masks. The first outlines the importance of skin preparation before and after wearing the mask. Preparation should focus on facial points of contact with the mask and any personal problematic areas (NPIAP, 2020). Second, frequent PPE offloading is recommended to reduce bacteria build up and allow the skin to recover. This offloading should be performed according to donning and doffing protocols. Third, treat any visible skin injuries that are caused by the PPE. The panel suggests that the wounds could be treated with ‘visible injury or open wound with topical moisturisers, liquid skin sealants/protectants, cyanoacrylate or a protective non-porous dressing’ (NPIAP, 2020). Further research should be conducted surrounding the design of PPE and any improvements that can be implemented to reduce risk of skin injury.
The use of gloves has been shown to disrupt epidermal barrier function and skin homeostasis (Montero-Vilchez et al, 2021). The frequent hand washing, use of harsh cleaning materials, and glove use all contribute to decreased epidermal barrier function, which inhibits protection against COVID-19. The use of gloves contributes to higher erythema and temperature which can increase skin permeability, ultimately increasing risk for skin reactions. According to the World Health Organization (2009), healthcare workers are required to perform hand hygiene at five moments: before touching the patient, before clean/aseptic procedures, after body fluid exposure risk, after touching the patient, and after touching the patient surroundings. With the added risk of COVID-19, healthcare workers are also expected to don a new pair of gloves in each patient interaction. Our results demonstrated that skin integrity issues experienced related to the use of gloves include itchiness, redness, dry skin, and broken skin. Of interest, 25% of participants stated that they experience dry skin on the hands related to gloves; however, 50% stated that they did not moisturize their hands on a regular basis. Regular moisturising can mitigate skin dryness and roughness caused by frequent hand washing (Kampf and Einen, 2006). In Canada, it should be noted that, skin care is an individual responsibility and most employers do not provide moisturisers for health professionals' use. It is therefore important to include moisturising as an education topic for health professionals.
The need to wear protective gowns corresponds with the type of isolation a specific patient is under. For a patient requiring no protective precautions, institutions did not require health professionals to wear gowns. Despite this, patients would be put under precautions for COVID-19 on essentially every admission to a healthcare setting until their test results proved negative. With these considerations in mind, the majority of health professionals wore reusable cloth gowns (60%), disposable cloth gowns (54%), and disposable waterproof gowns (47%) when required. Healthcare workers reported feeling overheated and restricted in the frequent gown use, but some confirmed it was worth it as it improved patient safety and made the patients feel safer (Lee and Goh, 2021). Increased temperature beneath the gowns contributes to greater reports of perspiration, which can pose challenges to certain individuals. Lee and Goh (2021) reported that increased perspiration and friction caused by gowns was associated with the presentation of eczema and contact dermatitis in varying individuals. They recommended that healthcare workers should wear thin, moisture-wicking fabrics beneath their gowns to prevent excessive heat and humidity. In addition, frequent breaks from the protective equipment should be granted to allow healthcare workers to re-hydrate.
In the current study, 43% of respondents stated that their mental health was negatively affected by wearing PPE. Swaminathan et al (2022) supported the notion that PPE use impacted the mental health of health professionals. They reported that PPE use was associated with increased somnolence, anxiety, depression, and fear of contracting the coronavirus while doffing PPE. Healthcare employers across the continuum of care should include physical (providing adequate moisturisers and appropriate PPE) and mental health resources for health professionals. Swaminathan et al (2022) highlighted an important concept in that the future impact of COVID-19 is not known and it can be expected that other viruses with a significant impact will emerge in the future. It is important that health professionals explore the lessons learned from the first waves of the pandemic and implement measures to ensure the effects of prolonged PPE use are minimised in the future. It is imperative that manufacturers who produce PPE continue to work with their research and development teams on products that minimise the impact of PPE use on the skin of health professionals.
Conclusion
By better understanding the impact of PPE use on Canadian health professionals, existing recommendations, such as those of the NPIAP, can be adapted for use in Canada and guidelines can be developed to prevent and manage PPE-related skin injuries among health professionals. The current study is an important first step in the understanding of how Canadian health professionals are impacted by PPE usage. Education for health professionals should focus on skin protection (regular skin moisturisation), prevention of PPE-related skin complications and support for mental health issues. Further research is required to fully understand the impact of PPE use on health professionals and to minimise the effects of prolonged PPE use on health professionals in the future.
KEY POINTS
- During the COVID-19 pandemic, the prolonged use of personal protective equipment (PPE) has contributed to health professionals suffering while still trying to maintain patient safety and comfort
- This survey asked health professionals across various health settings in Canada about their experiences wearing PPE
- Pressure injuries and acne were the most common complaints with face protection, 39% of respondents wore the same mask all shift and only removed at the end of the shift
- Dry skin was the top reported glove-related issue, and 51% reported never or occasionally moisturising their hands, with 49% moisturising at least once a day
- Education for health professionals should focus on skin protection (regular skin moisturisation), prevention of PPE-related skin complications and support for mental health issues.
CPD reflective questions
- Can you identify personal protective equipment (PPE) related skin injuries among health professionals?
- Can you describe the importance of ensuring any prevention or treatment does not interfere with PPE efficacy?
- What else can health professionals and employers do to reduce skin damage among health professionals related to PPE usage?


