Eating disorders are serious illnesses that impact both physical and psychiatric health. Eating disorders involve ‘abnormal eating behaviour and preoccupation with food as well as prominent body weight and shape concerns’, as defined in the ICD-11 (International Classification of Diseases) (World Health Organization, 2019). There are a number of eating disorders, each with their own presentations: the primary type, featured in this study, is anorexia nervosa, the key features of which include:
‘… an intense fear of weight gain and a disturbed body image, which motivate severe dietary restriction or other weight loss behaviours such as purging or excessive physical activity.’
Other eating disorders include bulimia, or ‘binge-eating followed by compensatory purging behaviours’ (Nitsch et al, 2021:333), diabulimia, or ‘the deliberate administration of insufficient insulin for the purpose of weight loss’ (Coleman and Caswell, 2020), and avoidant/restrictive food intake disorder (ARFID), described as:
‘… avoidance of certain foods or categories of food resulting in a diet that is limited in variety, and/or restriction of overall intake resulting in a diet that is limited in volume.’
The Medical Emergencies in Eating Disorders (MEED) report (Royal College of Psychiatrists (RCPsych), 2023) was released in 2022 (and updated in 2023) to aid health professionals in recognising when a patient is medically compromised due to an eating disorder, and to give guidance for hospital management. The report replaced the Management of Really Sick Patients with Anorexia Nervosa (MARSIPAN) guidelines, published in 2010 and revised in 2014, and the Junior MARSIPAN guidelines, published in 2012.
The MEED report includes a risk assessment with a list of red, amber and green flags (RCPsych, 2023:31-35): this suggests that one red flag or two amber flags indicate an impending threat to life, providing a tool for clinicians when assessing a patient with an eating disorder.
The red flag list consists of a range of warning signs, including a body mass index (BMI) of less than 13, pulse rate of less than 40, fluid refusal and a tympanic temperature of less than 35.5°C. Further indicators include life-threatening medical conditions (eg diabetic ketoacidosis, severe haematemesis), long corrected QT interval with another ECG abnormality, a number of biochemical abnormalities (such as hypokalaemia and hyponatraemia) and low white cell count or low haemoglobin. There may also be acute food refusal, very poor engagement with the management plan, high levels of activity, severe purging behaviours, and severe self-harm.
There are fewer amber flags. These include a BMI of between 13 and 14.9, pulse rate of between 40 and 50, severe fluid restriction, temperature of between 35.5°C and 36°C, non-life-threatening medical condition (eg mild haematemesis), long corrected QT interval with an otherwise normal ECG, poor engagement with the management plan, moderate levels of activity, purging behaviours, and self-harm.
People with eating disorders are more likely to have other psychiatric conditions. There is a significant bidirectional increase in the incidence of having both an eating disorder and other psychiatric diagnoses (Momen et al, 2022). Common psychiatric comorbidities of eating disorders include mood disorders (most commonly major depressive disorder), anxiety disorders, substance abuse disorders, obsessive compulsive disorder, post-traumatic stress disorder, and schizophrenia (Blinder et al, 2006; Hambleton et al, 2022). Associations have also been identified with neurodiversity, including autism spectrum condition (Huke et al, 2013).
The Mental Health Act 1983 allows for involuntary treatment of patients with psychiatric issues that ‘present significant risks to themselves or others’ (RCPsych, 2018:4). According to the National Institute for Health and Care Excellence (NICE) (2017) guidelines, the Act is applicable in treating eating disorders when:
‘… a person's physical health is at serious risk due to their eating disorder, they do not consent to treatment, and they can only be treated safely in an inpatient setting.’
The MEED report (RCPsych, 2023) contains a flowchart to aid decision-making regarding the use of legal frameworks to admit a patient to hospital. Patients differ in response to involuntary treatment: according to Seed et al (2016), for some it can cause even more difficulty between them and staff responsible for their treatment due to feeling ‘powerless’ or a loss of personhood, whereas for others there may be an element of relief that they were no longer in charge of their food intake.
For some patients, discharge to the community would not be appropriate as they need further inpatient care, so they may be referred for eating disorder treatment at a specialist eating disorders unit (SEDU) (RCPsych, 2023:62).
The aim of this study was to evaluate a patient cohort at a large teaching hospital in Manchester and identify whether there was a correlation between the severity of physical compromise experienced by patients admitted with an eating disorder (as determined by the number of red and amber flags they have on admission) and the likelihood of three different outcomes of their admission. The outcomes looked at were detainment under the Mental Health Act 1983 (‘sectioning’), length of stay, and discharge destination (further specialist inpatient care or community care).
Methods
The study used retrospective data, anonymised before analysis, for 27 patients who had been diagnosed with an eating disorder and were admitted to an adult ward at a large inner-city teaching hospital between March 2018 and April 2023. This review was undertaken as a medical student project within the Manchester University NHS Foundation Trust institutional ethical framework as part of the University of Manchester Medical School Applied Personal Excellence Pathway. Formal ethics committee approval was not required.
Inclusion and exclusion criteria
Patient health data were documented, using paper patient notes, alongside the electronic patient record systems. For the purposes of the study the data extracted from each record were those indicating red flags for a patient's physical health on admission, such as BMI, evidence of very little food or liquid intake prior to admission or acute food refusal, clinical observations, ECG results, and blood test results. Further data recorded were the patient's age, the eating disorder they had been diagnosed with, length of stay, ward of admission, whether they had been sectioned at any point in their admission, and the discharge destination.
One patient who had been diagnosed with anorexia nervosa in the community was excluded because none of their hospital admissions were linked to their eating disorder, leaving 26 patients for analysis in the study.
Statistical approach
The MEED report (RCPsych, 2023: 31) states: ‘… a patient with one or more red ratings or two or more amber ratings should be considered as high risk.’ The authors therefore used the risk assessment tool provided in the report to identify patients' level of risk. The number of red and amber flags relating to medical compromise for each patient was therefore calculated with reference to the criteria set out in the report (RCPsych, 2023). For the purposes of the analysis, two amber flags were equated to one red flag to create an overall flag score for each patient. Using this scoring method, the highest possible score was 20.
The SPSS statistical software package was used to perform a binomial logistic regression, with the independent variable being a patient's overall flag score and the dependent variable being whether the patient had been sectioned at any point during admission. This was used to determine whether there was a correlation between severity of physical compromise and likelihood of being detained under the Mental Health Act 1983.
Another binomial logistic regression was then performed, the independent variable being the overall flag score and the dependent variable being the place of discharge (community care or further inpatient care). This aimed to determine whether there was a correlation between severity of medical compromise and being referred for further inpatient care.
The SPSS software was also used to perform a simple linear regression, with the overall flag score as the independent variable and length of stay as the dependent variable. This aimed to determine whether there was a direct linear correlation between the severity of physical compromise and length of admission.
Results
The majority of data were retrieved for all 26 patients deemed eligible for inclusion. However, paper dietetic notes were missing for three patients, so it was not possible to determine their calorie intake prior to admission. Other missing information included two patient ECGs, and in a further two cases, it was not possible to obtain potassium levels on admission due to haemolysis. Nevertheless, there were sufficient data on these patients, so they were included in the study.
Patient demographics
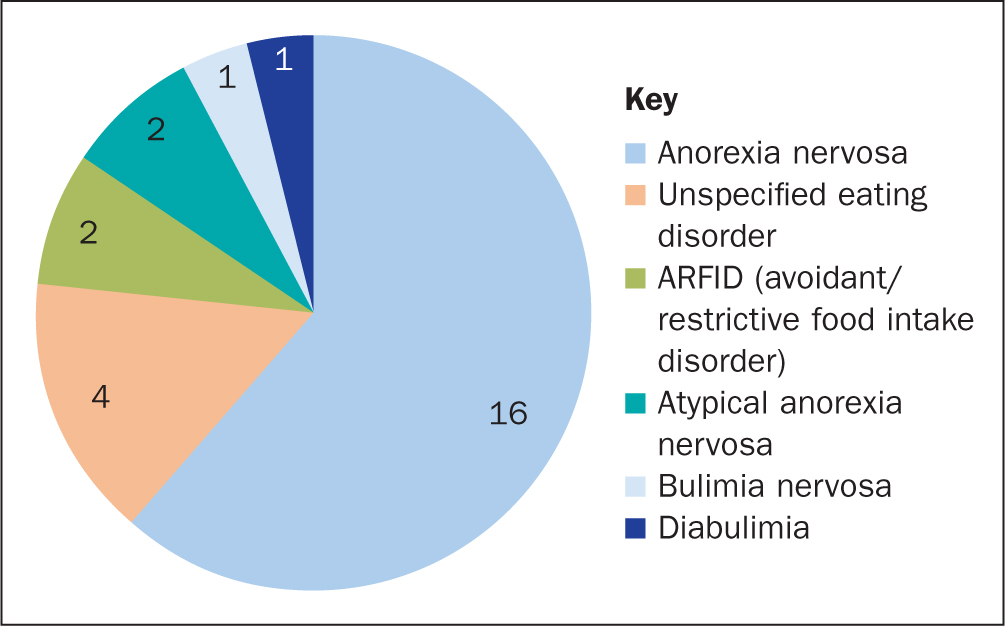
Of the eligible patients (n=26), 16 had a diagnosis of anorexia nervosa, 4 an unspecified eating disorder, 2 an ARFID, 2 atypical anorexia nervosa, 1 bulimia nervosa, and 1 diabulimia (Figure 1). There were 21 were female (80.8%) patients and 5 male (19.2%) patients.
Five patients (19.2%) also had a diagnosis of autism spectrum condition: 4 were female and 1 was male. Within this group, there were 2 anorexia nervosa diagnoses, 1 diabulimia diagnosis, 1 atypical anorexia nervosa diagnosis, and 1 ARFID diagnosis.
The youngest patient was aged 17 years, but had been admitted to an adult ward and so was included in the study; the oldest was aged 70 years. After excluding this patient as an outlier, the mean age was calculated at 24.7 years (SD=8.28)
In 2018, the number of patients with an eating disorder was 2, but increased to 11 in 2021.
Outcomes
There were no deaths or serious medical outcomes among the 26 patients.
Length of stay
Patients were admitted to a variety of wards: 10 to gastroenterology, 7 to acute medicine, 5 to general medicine, 1 to the high dependency unit, 1 to thoracic medicine, 1 to surgical outliers, and 1 to upper gastrointestinal (GI) surgery.
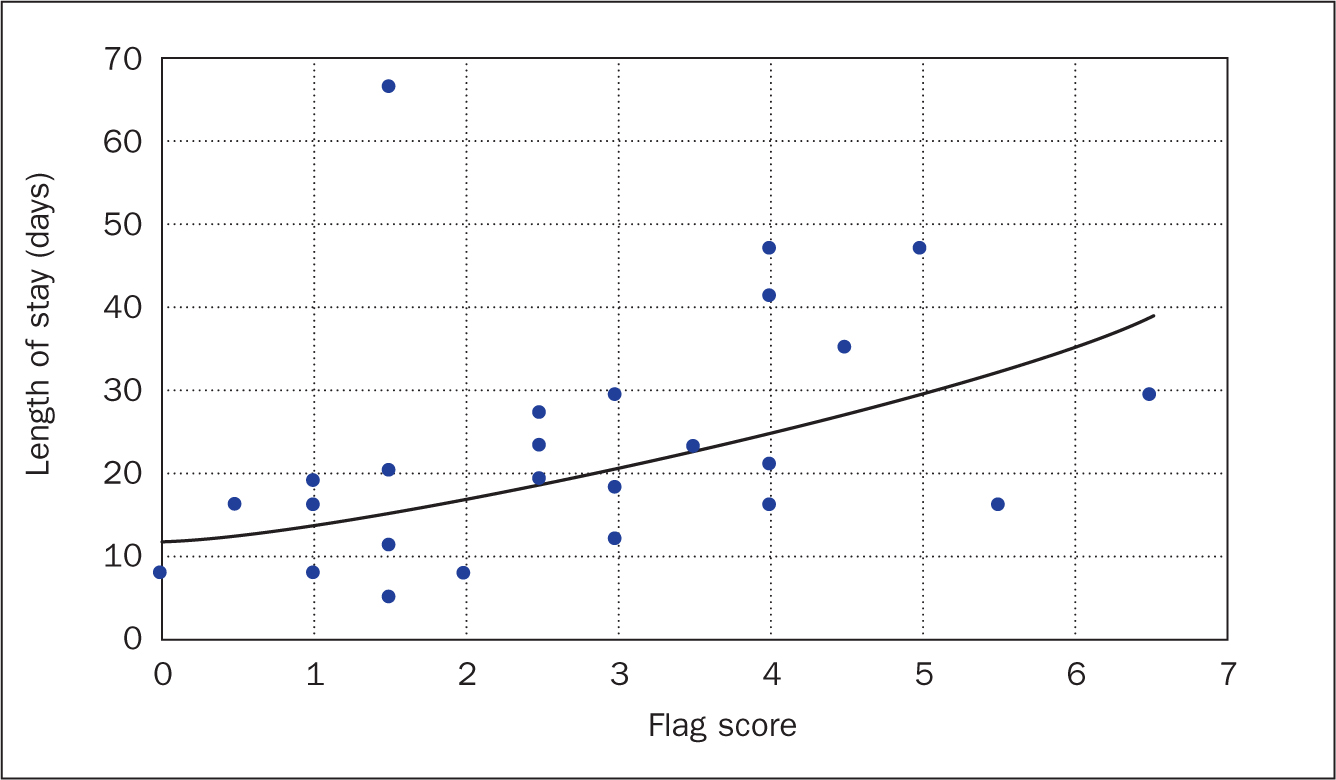
For the specific analysis of length of stay, 1 patient was excluded, because their stay was prolonged due to specialist funding issues. For the remaining 25 patients, the longest stay was 66 days and the shortest stay was 5 days. Mean length of stay was 23.2 days (SD=14.56) and the median was 19 days.
Discharge destinations and detainment
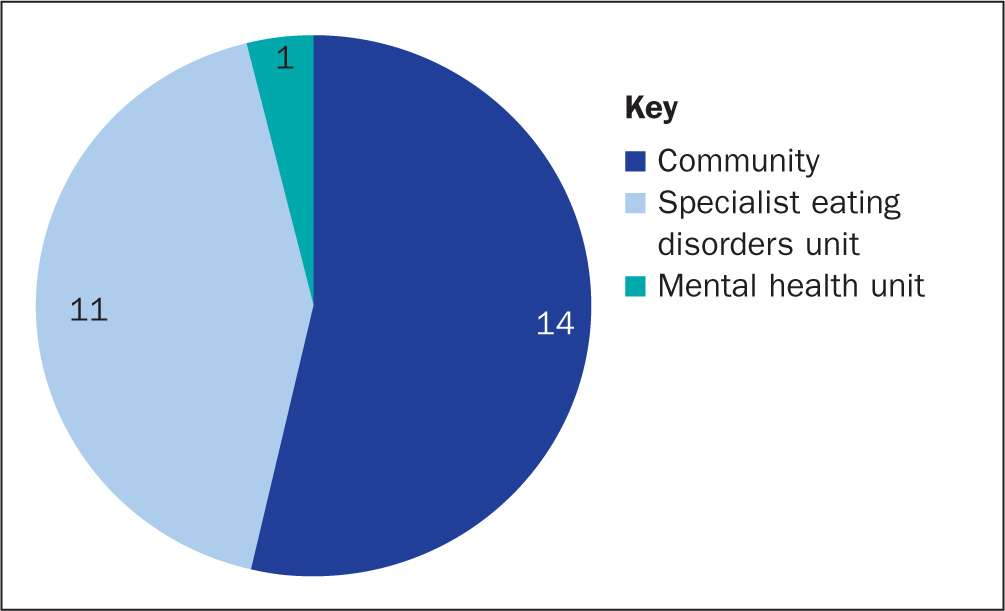
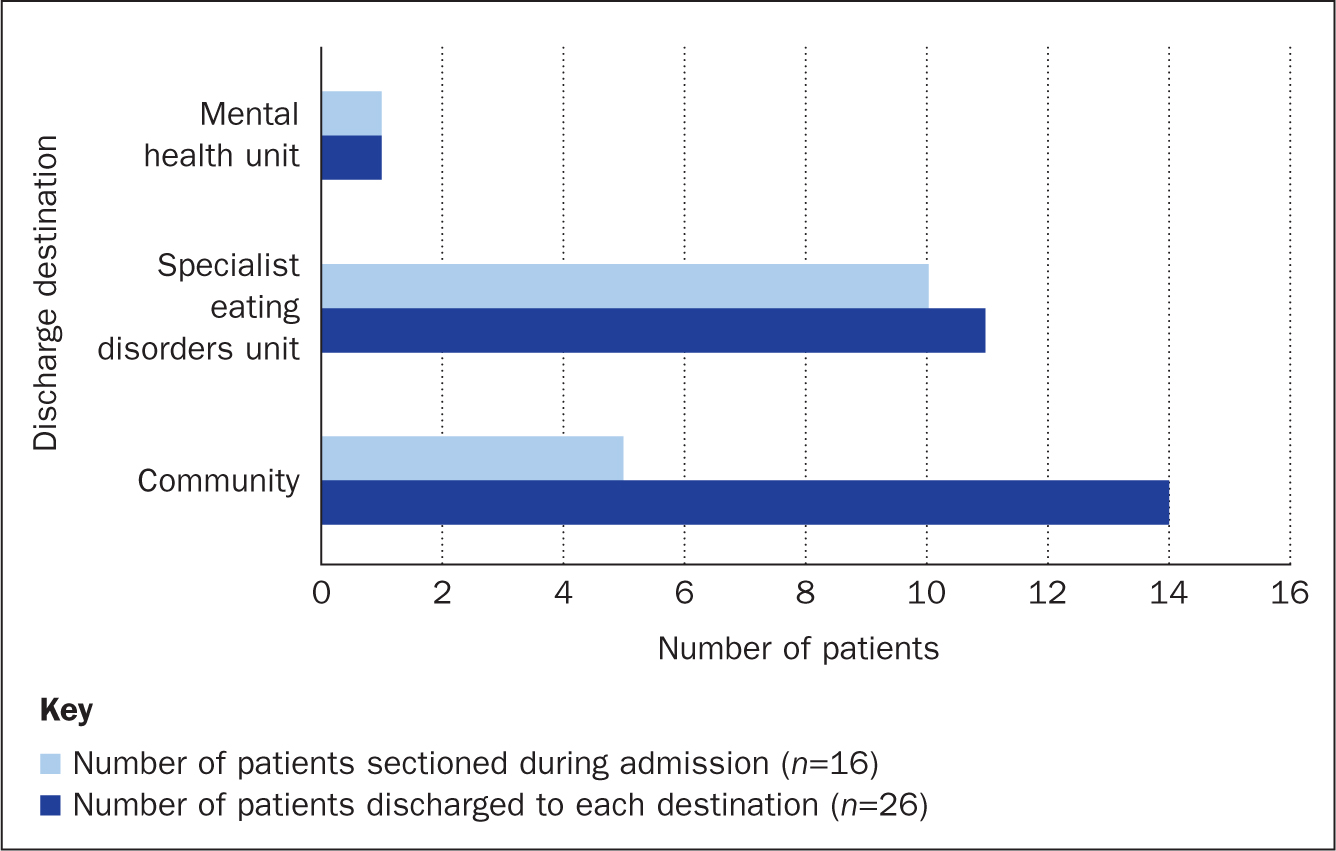
Fourteen of the 26 patients were discharged to the community, 11 to a SEDU, and 1 to a general mental health unit (Figure 2). A total of 16 patients were detained under the Mental Health Act during their admission (Figure 3): 5 of those sectioned were subsequently discharged to the community, 10 were discharged to a SEDU, and 1 patient to a mental health unit. The authors were interested to determine if there was any correlation between whether a patient had been sectioned and their discharge destination.
Red and amber flags
The highest number of red flags was six, identified in 1 patient, and the lowest was zero, seen in 2 patients. The highest number of amber flags was three, noted in 2 patients, and the lowest was zero, identified in 10 patients. When combining to create an overall score, the highest score was 6.5 out of a total of 20, seen in 1 patient, and the lowest was zero, seen in 1 patient. The mean score was 2.8 (SD=1.64), and the median score was 2.75.
Correlations between flag score and outcomes
The binomial logistic regression between overall flag score and whether a patient had been detained under the Mental Health Act 1983 showed no statistically significant correlation (P=0.243).
A binomial logistic regression between overall flag score and discharge location was also performed, which were classified as specialist inpatient unit or community care. The P value was 0.940, again showing no significant correlation between the two.
The simple linear regression performed between the number of red flags and length of stay gave a P value of 0.063, showing no significance (Figure 4).
Discussion
Demographics
When paediatric and adult populations have been taken together, age at onset was found to be younger for eating disorders compared with other mental health conditions. Solmi et al's (2022) large-scale meta-analysis suggested a mean age at onset of 15.5 years for both anorexia nervosa and bulimia nervosa, with onset before the age of 18 years 55.2% and 45.3% respectively.
In this study, the mean age of the 26 patients was 24.7 years, which is in line with findings reported elsewhere. For example, studies looking at adult patients with anorexia nervosa have reported a mean age of 24.0 years (Fairburn et al, 2013) and 27.2 years (Hiney-Saunders et al, 2021), with the largest study identified reporting a mean age of 29.6 years (Ayton et al, 2022).
In this study, the majority of patients were female, with a ratio of roughly 4:1.
Outcomes
There were no deaths or serious outcomes among the 26 study patients. The primary finding was that severity of medical compromise using a score devised according to the red and amber scoring system outlined in the MEED report did not appear to predict outcomes following admission: length of stay, likelihood of being detained under the Mental Health Act, and discharge destination. The authors recognise that this is not the focus of the MEED criteria and recommendations. There are a number of scoring tools to identify patients with eating disorders such as SCOFF (Morgan et al, 1999), and self-reported questionnaires such as the Eating Disorders Inventory (EDI) (Garner et al, 1983), but the authors did not identify a scoring tool to predict admission outcomes.
This does not mean that physical health is not crucial in monitoring eating disorders treatments. Severely medically compromised patients will need more careful medical monitoring and are at a higher risk of acute complications and death - and the red, amber, and green flags checklist was designed to assess for signs of impending risk to life. Eating disorders can be fatal, so thorough clinical assessment and treatment of medical abnormalities are vital.
Increasing incidence and association with autism spectrum conditions
There was a marked increase in admissions over the 5-year study period from 2 admissions in 2018 to 11 in 2021, which was a trend also reported in Devoe et al's (2023) systematic review. This higher number of admissions has continued, with 12 admissions identified by the end of 2023.
Of the 26 patients included in the study, 19.2% had an autism spectrum condition diagnosis. Management for these patients may require adaptation to meet their specific needs, and innovative therapies targeted at eating disorders in neurodivergent patients should be considered (Tchanturia et al, 2021). Individualised therapies can be adapted, recognising particular concerns for autistic patients, eg sensory sensitivities that aim to create a ‘more autism spectrum-friendly environment’, including use of sensory toys.
The MEED report
The MEED report (RCPsych, 2023) sets its objectives as follows:
‘… to make preventable deaths due to eating disorders a thing of the past.’
‘All patients with eating disorders should be offered NICE approved psychological treatment at the earliest opportunity.’
The red, amber, and green flags list was designed as a risk assessment tool to help admitting clinicians identify whether a patient is at imminent risk of death, rather than to correlate with patient outcomes.
For this study, the authors used the list of red and amber flags to create the flag score, as the guidance provides a reliable and up-to-date approach to evaluating patients' physical health on admission. The use of red and amber flags made it relatively simple to devise a scoring system for the physical health of each patient.
The MEED report is a comprehensive document that was found to be simple to navigate, so is not necessarily a set of guidelines for quick reference when time is limited. There is a one-.page eating disorders risk checklist in Annexe 3 (RCPsych, 2022a) that provides a comprehensive summary of important factors to consider when assessing and managing a patient with an eating disorder. The checklist also includes a summary of important management points, including re-feeding guidelines and behaviours to look out for. The report's foreword states:
‘A key objective of this report is for all clinicians likely to encounter such patients … to have practical tools at their fingertips.’
The recommendations of the report should have wide applicability. Patients with eating disorders are admitted to a variety of wards in general hospitals, where eating disorder specialists will not be readily available. For example, the patients included in this study were admitted to wards such as general medicine, upper GI surgery, surgical outliers and thoracic medicine. It is therefore important for health professionals to recognise eating disorders in patients who have been admitted for other reasons. Nurses and other clinicians who are not specialists or experienced in treating patients with eating disorders should find the report a valuable guide to use as a reference when devising a management plan for these patients. Annexe 1 of MEED, which contains guidance carried over from the original 2022 edition, has a two-page summary sheet specifically intended for nurses caring for patients with eating disorders (RCPsych 2022b:9-10).
Limitations
This was a small-scale retrospective study that had a limited sample size. If the authors had had more time, the study would have been carried out trust-wide, including the local children's hospital, which would have increased the sample size and yielded more robust results.
Future trends
The past 5 years have seen a marked increase in the number of patients diagnosed with eating disorders, with waiting times for treatment increasing. One study (Ayton et al, 2022), looking at the South-East of England, found that waiting times had increased by 21% since the start of the COVID-19 pandemic Social isolation, promotion of exercise as an essential daily activity, reduced availability of certain foods, an increased focus on cleanliness, and reduced or removed access to services are potential reasons that the pandemic may have contributed to increased eating disorder presentations and worsening of symptoms in patients already diagnosed with an eating disorder.
This highlights a need for increased funding and resources for eating disorders treatment. Longer waiting times are associated with poorer prognosis due to prolonged starvation and eating disorder habits becoming more ingrained (Allen et al, 2023). Having an increased availability of eating disorder services should lead to better patient outcomes.
Recommendations for future research
A beneficial area of research would be to determine how many clinicians are aware of, and are using, the MEED report (RCPsych, 2023) when treating patients with eating disorders. If the number of health professionals is found to be low, this would indicate the need to increase awareness of the guidelines. They are up-to-date and comprehensive and so are a useful tool for all clinicians who could be treating patients with eating disorders. Increased awareness around signs of an eating disorder is also important, as patients' eating disorders could be going unnoticed for extensive periods of time, leading to treatment delays. There is a summary sheet in Annexe 1 of the MEED report aimed at nurses that we recommend as a reference (RCPsych, 2022b:9–10).
A further area of research could look at whether there is a correlation between medical compromise and admission outcomes with a larger sample size, for example patients across an entire trust or deanery.
Conclusion
The severity of medical compromise did not appear to correlate with length of stay, discharge destination or detainment under the Mental Health Act. The study's demographic data were in line with that reported in larger studies: these showed that anorexia nervosa is most common in females under the age of 30 years. However, it is important to note that anyone has the potential to develop an eating disorder, which are not only seen in young females.
The authors have recently implemented new guidelines for the management of patients with eating disorders or suspected eating disorders in their Trust. Embedding the recommendations of the MEED report, in the light of a better understanding of their patient group, has helped in their aim to develop a better service for patients and staff.
Patients with eating disorders are admitted to a wide variety of wards, so the MEED report, which is a well-designed document, would be a beneficial tool for use by the majority of health professionals.
KEY POINTS
- Patients with eating disorders are at risk of serious complications, which can be physical and psychiatric, so predicting who is at greatest risk can be difficult
- The authors analysed data from patients admitted for an eating disorder at a large teaching hospital to determine whether there was a correlation between severity of physical compromise and three admission outcomes: length of stay, detainment under the Mental Health Act 1983, and discharge destination (specialist eating disorders unit, general psychiatric unit, or the community)
- The use of MEED toolkits and summary sheets is a useful quick reference for health professionals who may encounter patients with eating disorders
CPD reflective questions
- How often do you see patients with eating disorders?
- Could you have missed this diagnosis?
- What are the key challenges in caring for patients with eating disorders?
- Does your hospital use the MEED guidance? Could you incorporate this into your practice?


