The management of genital oedema in adults and children is not part of standard undergraduate training of nurses and allied health professionals, and postgraduate training opportunities in genital oedema are rare. Although the true prevalence of genital oedema is unknown, the condition may present in almost any arena of primary or secondary care. In particular, pelvic health physiotherapists and urology nurses regularly support patients with incontinence and impotence but the management of chronic scrotal, penile or labial oedema is rarely reported. Even within specialist lymphoedema (chronic oedema) clinics in the UK, patients with genital oedema represent only a small proportion of the caseload and the condition is thought to be under-reported by patients and professionals. There are limited opportunities for health professionals to accrue experiential learning through exposure to genital oedema. A project to encourage men to disclose genital oedema coincidentally exposed that some health professionals were as reluctant as patients to broach the subject (Noble-Jones at al, 2014; 2019a). It was suggested that low confidence may be due to a lack of specific education on genital oedema. There has been no previous investigation of the education needs of health professionals in order to manage genital oedema. In addition, given that the requirement for pertinent knowledge and skills for genital oedema management may be sporadic, the accessibility of resources for education delivery required exploration (Noble-Jones et al, 2019b).
Aim
The aim was to identify the education needs of health professionals in order to manage chronic genital oedema (lymphoedema) conservatively, and establish the medium of education delivery that most health professionals considered essential.
Method
This investigation reports the UK survey findings of a wider international project that used mixed methods (online survey and focus groups) to explore education needs (Noble-Jones et al, 2019b). The survey was developed from a literature review, evaluation of available curricula and rounds of discussion with key stakeholders (academics, lymphoedema specialists, urology and oncology nurses, pelvic health specialists and patients). This resulted in a list of topics that were currently included, or that could be included, in genital oedema education. These topics covered specific treatments for genital oedema, as well as background theory and supporting knowledge relating to care.
The survey asked respondents for their experience working with lymphoedema in general and in managing genital oedema specifically. They were asked to describe the level of confidence they had in their knowledge of genital oedema, their previous training and their education needs in relation to managing genital oedema. The scoring system used in various sections will be explained alongside the relevant findings.
Hyperlinks to the English language survey were distributed by British Lymphology Society (BLS), Lymphoedema Network Wales (LNW), and the International Lymphoedema Framework (ILF), and cascaded via social media to other health professionals in urology, oncology, community nursing and palliative care.
Health professionals in Wales had access to the survey for 4 weeks from 15 August 2019 and the remainder of the UK from 20 September 2019 to 30 November 2019.
Data analysis involved descriptive statistics and thematic analysis on open text responses, initially by the main author and subsequently by three members of the research team.
Review by Swansea Bay University Health Board (SBUHB) research and development team members found the project to be service development. SBUHB was the sponsor and funding was from Tenovus Cancer Care (a registered charity).
Findings
Respondents by profession, training and years of experience
The survey had 149 health professional respondents in the UK, of which 139 (93%), were female, 8 male and 2 declined to specify. Almost half indicated they were nurses (46%), 21% were physiotherapists and just 3% were occupational therapists, the remainder specified other roles including a uro-oncology nurse, urology surgeon, pelvic specialist physiotherapist and radiologists.
Most survey respondents reported already treating genital oedema (87%) while a further 11% anticipated doing so soon. Half (69/138) of those responding regarding supplemental education reported completing genital oedema training. Only three health professionals (2%) felt that their standard lymphoedema training (decongestive lymphatic therapy) was adequate preparation for managing patients with genital oedema.
In relation to experience of managing lymphoedema in other parts of the body, 38% (55/146) had over 10 years of experience, 25% had 6-10 years and 2-5 years' experience (36/146 and 37/146, respectively), and only 12% (18/146) had 0-1 year of experience. Cross-referencing years of experience with those who had undertaken genital oedema education (69/138) it was possible to see that those who had over 5 years' experience were more likely to have completed genital oedema education (Figure 1). Whereas in the group with 5 years or less experience of managing lymphoedema, those without genital oedema education outnumbered those with.
Figure 1. Completed genital oedema education by years' experience (n=138)
For 58% (40/69) of respondents the duration of their supplementary genital oedema education was 1-4 hours, whereas 28% (19/69) had received 5-8 hours, four respondents had 9-16 hours and six respondents had completed over 16 hours. Unsurprisingly, most of those with over 16 hours genital oedema education (5/6) had been managing other types of lymphoedema for over 10 years (Figure 2).
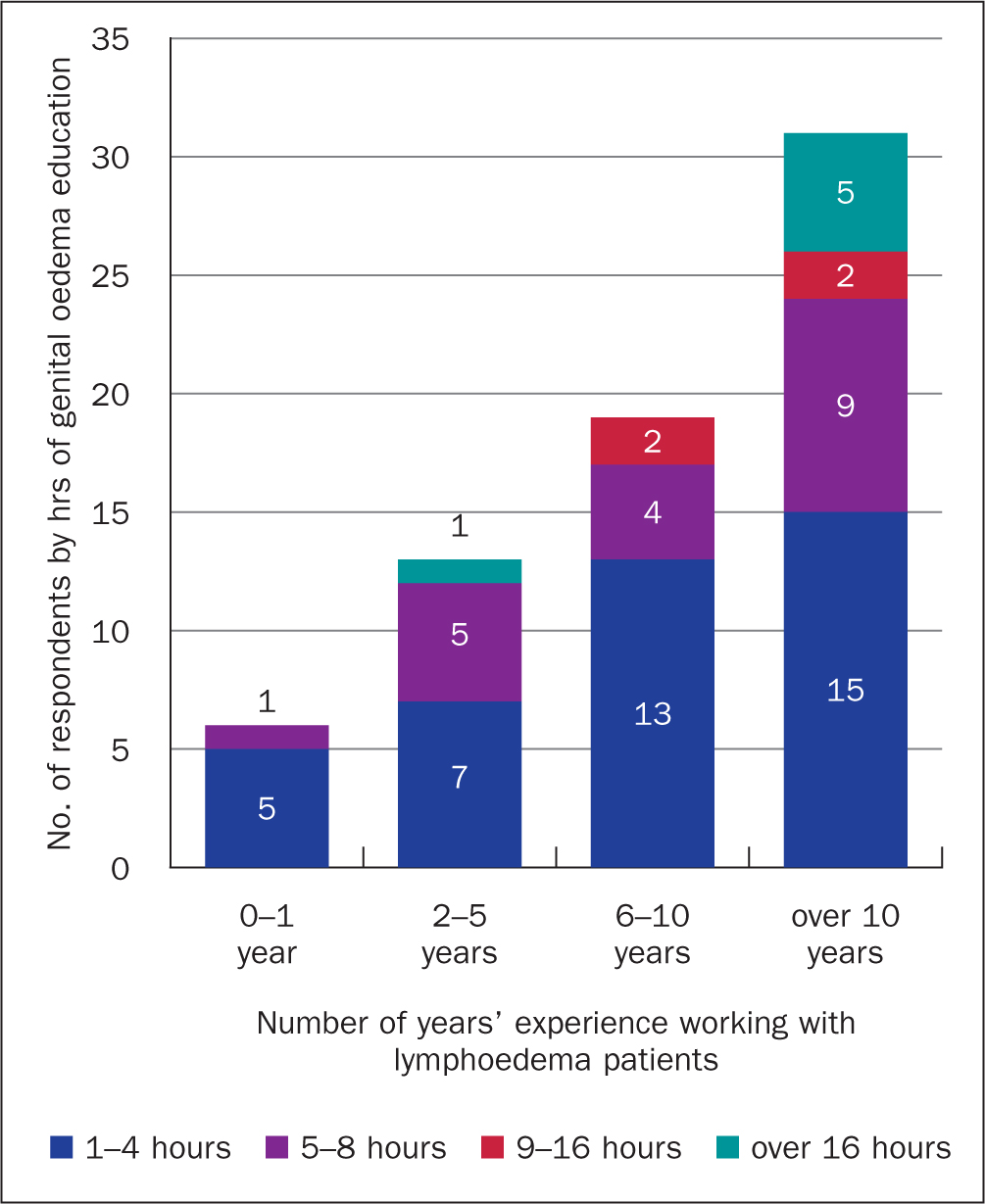 Figure 2. Hours of genital oedema education by years working with lymphoedema (n=69)
Figure 2. Hours of genital oedema education by years working with lymphoedema (n=69)
Current management of genital oedema
Only 22% (30/139) of UK health professional respondents reported using a specific genital oedema assessment tool, almost half of these using the Lymphoedema Genito-urinary Cancer Lymphoedema Questionnaire (LGLCQ) or its successor Lower Limb and Genital Lymphoedema Questionnaire (LLGLQ) (Noble-Jones et al, 2014; 2019a). The remaining 78% used generic patient assessment documentation.
The most commonly used treatment methods were skin care (to reduce infection risk) (96%), compression garments (92%) and manual lymphatic drainage (MLD/massage) (80%), followed by kinesiotaping/taping (72%), exercise (71%) and bandaging (61%) (Figure 3). Over one-third had used wound dressings (35%) on these patients and slightly more had used antibiotics (36.7%); 27.5% had used external scar work (deep massage to skin scars) but only 20% had used night bandaging.
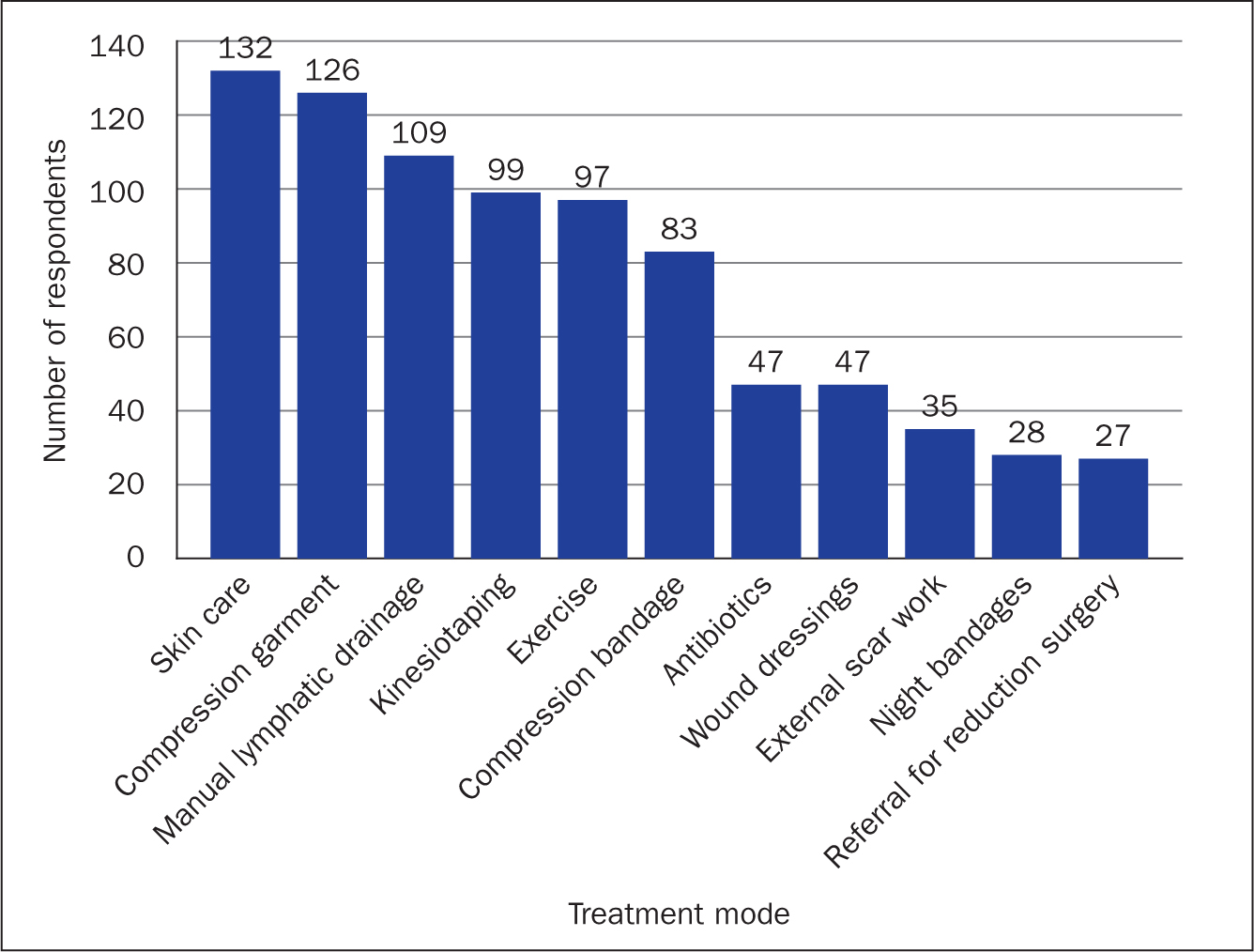 Figure 3. Treatment used for genital oedema (n=137)
Figure 3. Treatment used for genital oedema (n=137)
In relation to training received and treatments used, those using night bandaging were statistically more likely to have completed 5-8 hours of genital oedema specific training (P<0.05). There was a trend for those who had less genital oedema training to use MLD and garments, whereas those with more training were more likely to use bandaging; however, these did not reach statistical significance.
Onward referral to other services included recommendation for reductive or lymphatic surgery, compression pumps, sexual health services, dietitian, mental health, vaginal examination/treatment, referral to urology and to gastrointestinal specialists for assessment of Crohn's disease or similar.
Confidence in genital oedema-related knowledge
Respondents indicated confidence in their knowledge of background theory (eg, male and female anatomy, common pathology, legal/ethical/cultural considerations) and of treatment techniques (eg, skin care to reduce infection risk, bandaging, awareness of surgical techniques) from a list of genital oedema-related education topics. For each topic, the respondent scored 1 for ‘not confident at all’; 2 for ‘somewhat confident’ and 3 for ‘very confident’, or 0 for ‘not applicable’. An average weighted score was calculated for each topic. For example, an average weighted score of 1.42 in ‘using self-report tools for genital oedema patients’ showed that respondents (taken as a whole) had a low level of confidence in knowledge of that topic.
Confidence in knowledge of treatment techniques was generally higher than in the background theoretical topics covering: skin care, self-massage/simple lymph drainage (SLD) and compression garments, with weighted averages of 2.57, 2.46 and 2.36 respectively (Figure 4). This is emphasised by the dashed line on both Figure 4 and Figure 5 highlighting the midpoint of ‘somewhat confident’. In contrast, the average scores for theoretical background knowledge were generally lower than those for treatment techniques (Figure 5).
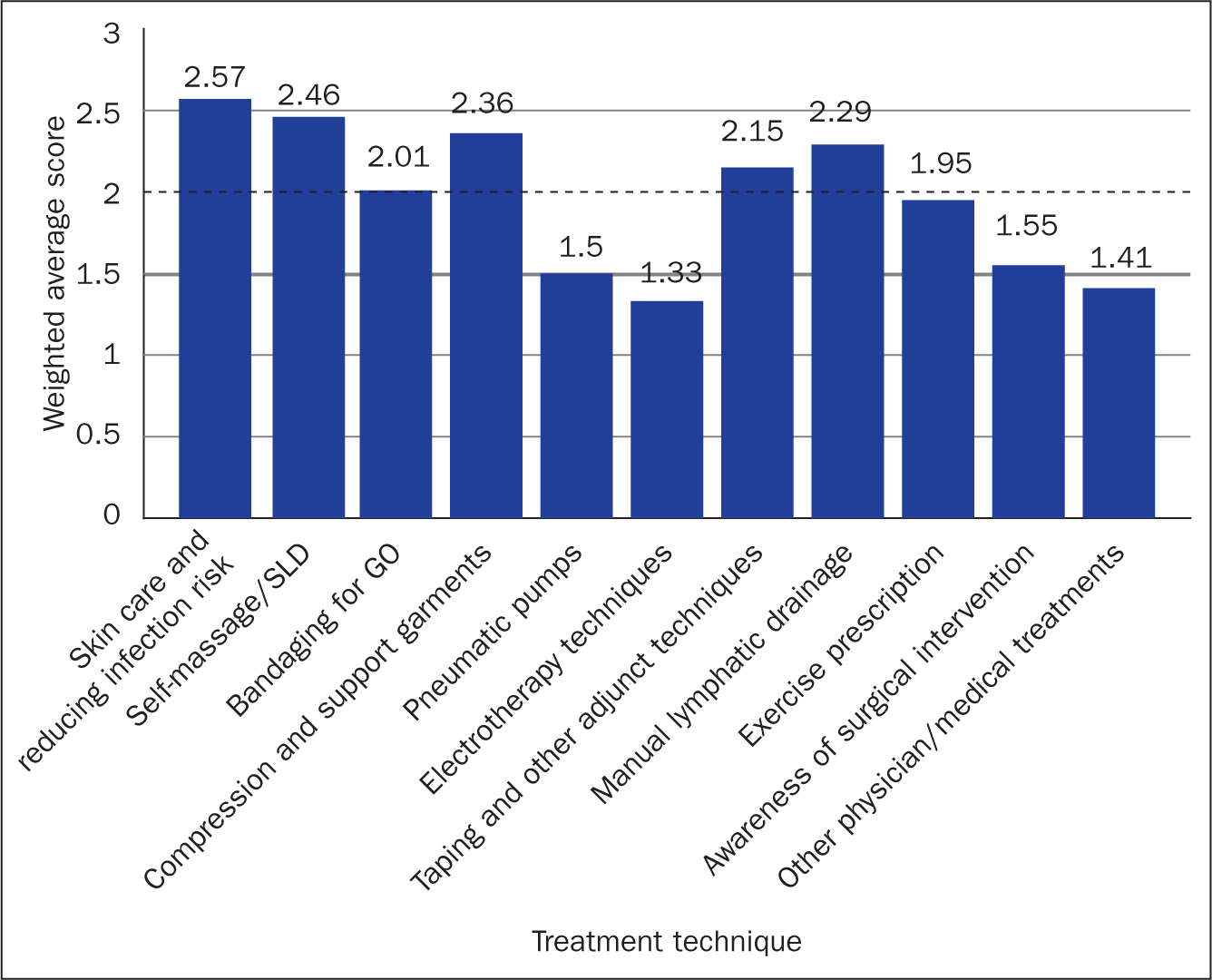 Figure 4. Confidence in knowledge of treatment techniques (weighted average scores) on a scale of 1 = not confident at all; 2 = somewhat confident; 3 = very confident (n=136). SLD=simple lymph drainage
Figure 4. Confidence in knowledge of treatment techniques (weighted average scores) on a scale of 1 = not confident at all; 2 = somewhat confident; 3 = very confident (n=136). SLD=simple lymph drainage 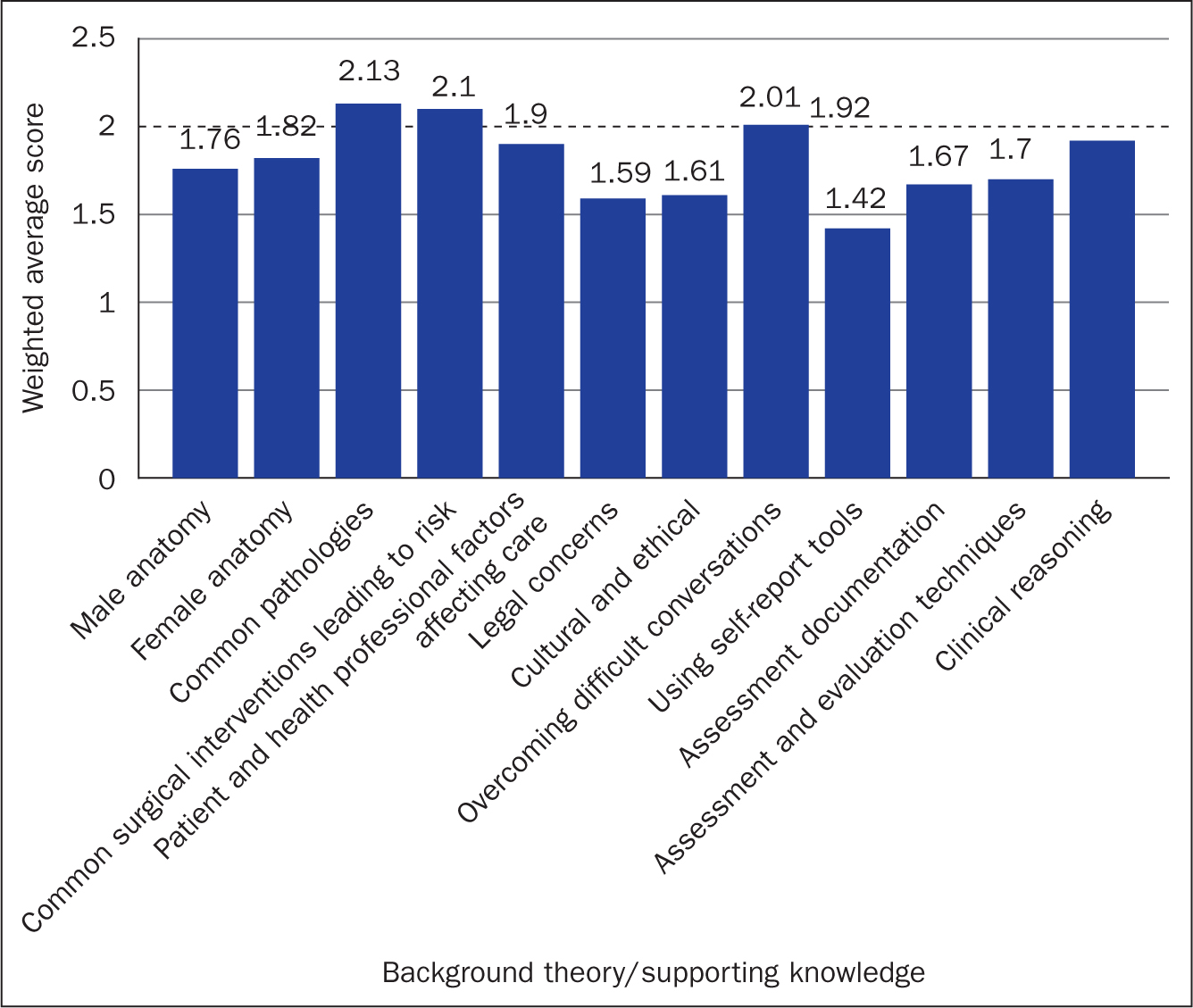 Figure 5. Confidence in supporting knowledge (weighted average scores) on a scale of 1 = not confident at all; 2 = somewhat confident; 3 = very confident (n=136)
Figure 5. Confidence in supporting knowledge (weighted average scores) on a scale of 1 = not confident at all; 2 = somewhat confident; 3 = very confident (n=136)
Confidence as impacted by education and years of experience
An average score across all topics (global score) was calculated to compare overall confidence in those with and without supplemental genital oedema education against years of lymphoedema experience (Figure 6). This exposed a difference between those with and without genital oedema education. The global average score for confidence in knowledge of all respondents was 1.88, but when split by genital oedema education the average scores become 2.02 and 1.74, respectively. When these are split by years of experience the difference was particularly significant in those with 2-5 years' experience in lymphoedema care (Figure 6). The steepness of the linear lines give an indication of the difference having supplemental education can make. This was particularly significant in those with 2-5 years' experience of lymphoedema.
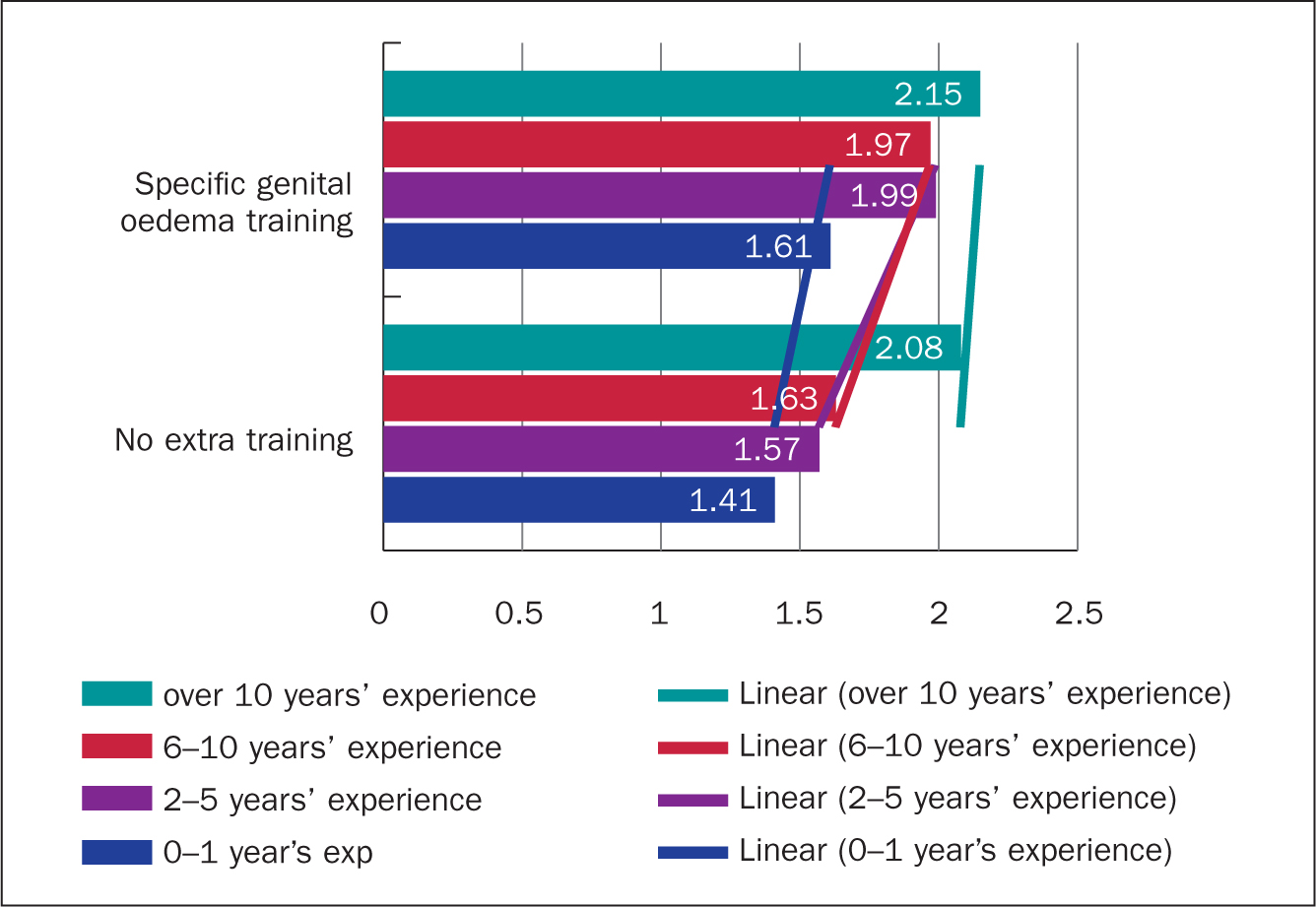 Figure 6. Comparing global scores of confidence in knowledge by years of experience and by genital oedema training (on a scale of 1 = not confident at all; 2 = somewhat confident; 3 = very confident)
Figure 6. Comparing global scores of confidence in knowledge by years of experience and by genital oedema training (on a scale of 1 = not confident at all; 2 = somewhat confident; 3 = very confident)
When analysed by topic, the difference in confidence score between those with and without genital oedema education ranged from 4.5% to 22.5% (Table 1). In all but one topic, the difference in confidence between health professionals with and without genital oedema education was statistically significant (P values ≤ 0.05).
Table 1. Percentage difference for health professionals with/without genital oedema education of confidence in knowledge score for genital oedema-related topics
| Topics of greatest percentage difference between respondents with/without supplemental genital oedema education | |
|---|---|
| Taping and other adjunct treatment | 22.5% |
| Manual lymphatic drainage | 21.5% |
| Assessment documentation for genital oedema | 19.5% |
| Exercise prescription for genital oedema patients | 18.5% |
| Bandaging for genital oedema | 18.5% |
| Pneumatic pumps in genital oedema management | 18.5% |
| Legal concerns when treating genital oedema | 16.5% |
| Self-massage/simple lymph drainage | 16.5% |
| Clinical reasoning for genital oedema-related treatment decisions | 16.0% |
| Topics of least difference (under 10%) | |
| Cultural and ethical concerns in treating genital oedema | 9.5% |
| Common surgical interventions leading to a known risk of genital oedema | 9.0% |
| Other physician/medical treatment for genital oedema | 8.0% |
| Anatomy of male pelvis and connected musculature | 6.5% |
| Anatomy of female pelvis and connected musculature | 4.5% |
Topics considered essential in education
Topics suggested as useful in supplemental education were divided into ‘treatment methods’ and ‘background theory’ (the same topics as shown in Figure 4 and Figure 5). Respondents rated the relevance of topics as ‘essential’, ‘useful but not essential’ or ‘not required’, with an option to indicate ‘I don't know’. In addition, participants could add topics via open text boxes. Of 23 topics suggested, 17 were rated ‘essential’ by over 80% of respondents. Four topics were essential for between 62% and 72%, and two topics were considered essential to fewer than a third of respondents. Background theory topics rated as essential by over 80% of respondents were: legal (99%), cultural and ethical concerns (98%), difficult conversations (93%), common pathology (94%) and surgery causing risk of genital oedema (90%), pathologies likely to cause the condition (94%), anatomy of the pelvis (male 85% and female 85%), patient and heath professional factors affecting treatment (89%), assessment techniques (88%), assessment documentation (84%), clinical reasoning (82%).
Treatment techniques rated essential by over 80% were: skin care and reducing risk (98%), compression garments (97%), self-massage (96%), manual lymphatic drainage (88%), exercise prescription (82%) and bandaging (81%). Fewer rated (kinesio) taping and adjunct treatments (72%), the awareness of surgical intervention (68%), the use of self-report tools (64%), and other physician treatment (62%). Less than a third thought that pneumatic pumps (33%) and electrotherapy techniques (31%) were essential topics for this supplemental education.
Topics rated essential compared with confidence in topic knowledge
Among the topics rated essential by over 80% of respondents, there were 5 topics that had a low confidence score (average weighted score under 2.0). The average score of respondents with genital oedema education was significantly higher than those without (Table 2). In all but two topics, the average score was less than ‘somewhat confident’ (<2.00), with or without genital oedema education. Although the level of confidence may differ between the two groups of health professionals, the data suggest education needs for all.
Table 2. Topics considered essential but where respondents reported low confidence with/without supplemental genital oedema education
| Percentage (n=134) who considered topic essential | Confidence (average weighted score) where 1=not confident; 2=somewhat confident; 3= very confident | ||
|---|---|---|---|
| with GO education | without GO education | ||
| Legal concerns | 89% (119) | 1.76 | 1.43 |
| Patient and health professional factors that impact on treatment | 88% (118) | 2.06 | 1.75 |
| Cultural/ethical concerns in treating genital oedema | 88% (117) | 1.70 | 1.51 |
| Assessment and evaluation of genital oedema | 88% (117) | 1.86 | 1.55 |
| Exercise prescription for genital oedema patients | 82% (110) | 2.14 | 1.77 |
Individual top three education needs in relation to genital oedema
Survey respondents identified their top three education needs as open text. This resulted in 370 responses (n=127) covering a wide range of needs, for example: ‘Difference in cellulitis presentation and causative bugs’; ‘Breaking down barriers—patient embarrassment’; ‘impact on patient's sexual relationships and micturition’; ‘national evidence-based/consensus guidelines’; and ‘achieving good long term, acceptable compression male and female’.
The research team allocated each response to one or more of 18 categories. Categories were not mutually exclusive since some responses described more than one issue. Some categories reflected earlier topics (eg patient assessment, compression); while other categories emerged from the responses such as protocols and pathways, context specific (eg, palliative care). Five of the 18 categories were supported by over half the respondents: compression (82/127), new content (71/127), surgery and medical interventions (67/127) and patient assessment (66/127). Suggested new content covered a broad range, for example, more information on the microbiology of relevant infections, and specific suggestions on how to demonstrate manual self-management skills without embarrassment, but only one or two respondents identified each suggestion. Of note was that a smaller but significant number of respondents (20/127) considered the means of education delivery a priority.
Format/medium of education resources
A list of 13 possible formats for education resources was given to participants with an option for open text addition. They were asked to indicate against each one whether they considered it: ‘essential’, ‘useful but not essential’, ‘not needed’ or ‘not applicable’. The format considered essential by most UK respondents was an e-learning package (94/127), followed by hard copy printed materials (85/127) (Figure 7). These were followed by video resources for themselves (80/127) and for patients (77/127). Similar numbers, over half the respondents, considered a collection of case studies (73/126) and collaborative events with allied specialists (72/127 urology; 70/127 pelvic health) to be essential (Figure 7). A mobile phone app (smartphone app) was indicated as being essential by fewer than 10% of UK health professional respondents (12/127).
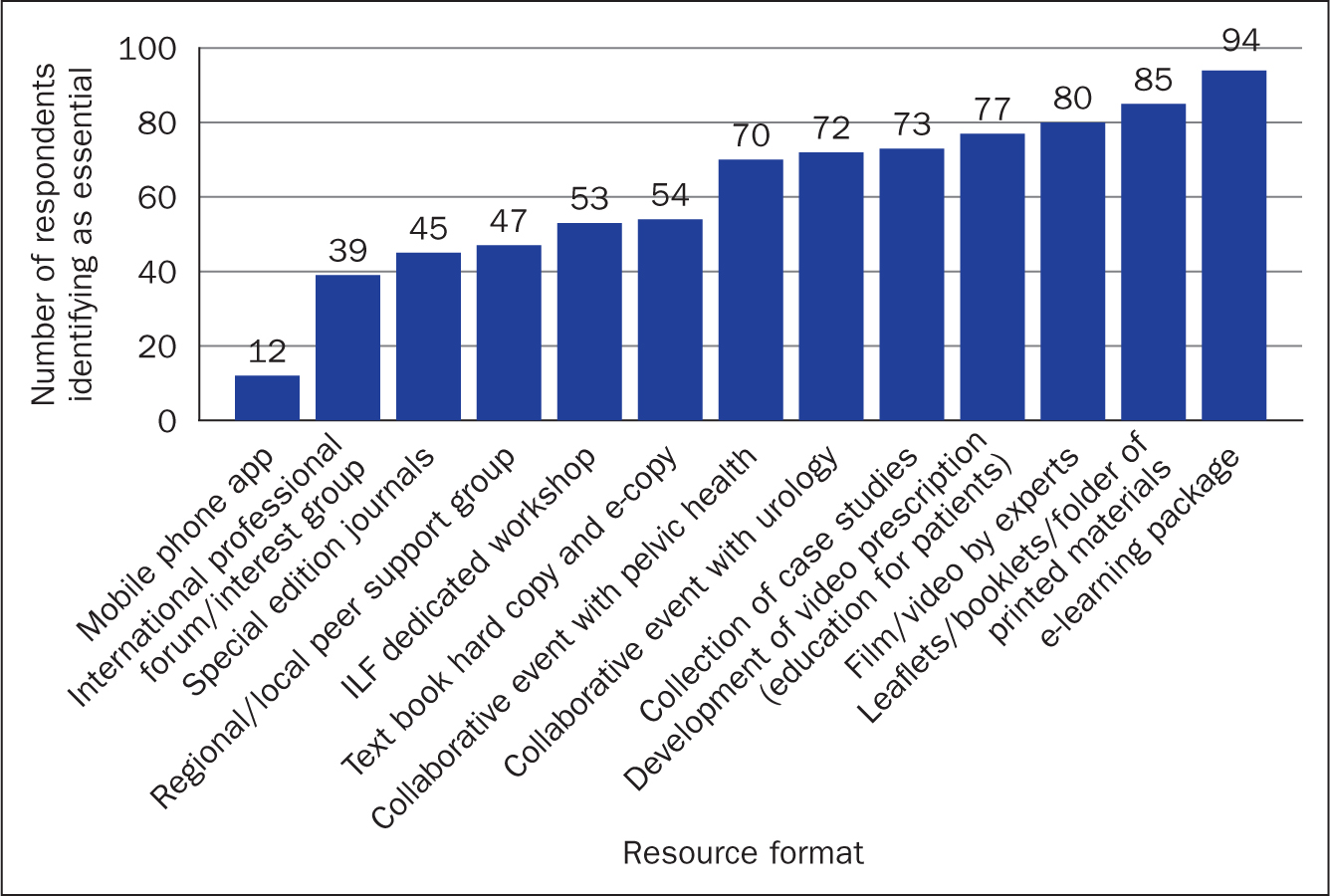 Figure 7. Resource formats indicated as essential by respondents (ILF=International Lymphoedema Framework)
Figure 7. Resource formats indicated as essential by respondents (ILF=International Lymphoedema Framework)
Discussion
Specific education needs of health professionals in relation to the conservative management of patients with genital oedema were identified in this study.
An accurate response rate for the survey is difficult to establish as the role of lymphoedema specialist nurse/therapist is not a protected title in the UK. The main professional group for lymphoedema specialists in the UK is the British Lymphology Society, which typically has over 530 members (BLS, 2020). Therefore, a response from 149 health professionals, with a completion rate of 85% (127/149), is good. The majority being female respondents is typical of the overall population of workers in this speciality. Similarly, the distribution of nurses, physiotherapists and occupational therapists showed an anticipated pattern, although the true figures for the UK are unknown.
A limitation of opt-in surveys is respondent bias. The finding that most health professionals were already managing patients with genital oedema, and that only a very small proportion (2%) felt that current education/training for lymphoedema specialists adequately prepared them, may reflect this. However, since the true prevalence of genital oedema—in men, women and children—is unknown, and there is no UK-wide national minimum data set for lymphoedema services, it is difficult to say if this is typical of the lymphoedema caseload. Overall, the respondents were very experienced in managing lymphoedema (in other parts of the body) with almost two-thirds having over 5 years' experience in this speciality and half having completed supplementary genital oedema education. Yet the overall confidence rating, of less than ‘somewhat confident’ (1.88), would seem to confirm the anecdotal reports of genital oedema management being complex and challenging (Vignes, 2018).
The duration of genital oedema education, for most respondents who had completed it, was 1-4 hours, with slightly fewer having completed 5-8 hours. Yet the difference in overall confidence in knowledge, and confidence in individual subjects, between those with and without genital oedema education was surprising. It is possible that the respondents who attended education had more confidence regardless of this specific education. However, when the data were analysed for number of years of experience the significant difference remained in all groups, except those with over 10 years in lymphoedema.
Over a fifth of respondents use the self-report tool (LGUCQ/LLGLQ) with their male patients; however, this is only part of an assessment process. Patient assessment was identified as a top education need by over half the respondents, therefore there is a clear need for specific and validated tools to support health professionals in accurate assessment of genital oedema, both male and female.
A limitation of self-reported confidence is that it could be an inaccurate perception based on having completed the education, ie health professionals may have more confidence in their knowledge simply because they have completed supplementary education, or less confident because they have not. It was important therefore to look at whether the confidence level affected practice since the original prompt for the investigation was that patients and health professionals felt practice would improve with more confidence (Noble-Jones et al, 2019a; 2019b). Overall, the treatment techniques reported by respondents are typical of lymphoedema in any part of the body and represent useful transferable skills to treat the genital area. However, compression and choice of wound care dressing can be a good indicator of health professionals' confidence (Blackburn et al, 2019). Compression of the genitals, whether with bandaging or a compression garment, is a very different proposition to application on an arm or a leg. Despite scoring high in the ‘confidence in knowledge’ score, compression remained the most popular category of individual top education need. Ensuring genital compression is comfortable and will remain in position, particularly after toileting, is a challenge. This may be reflected in the trend that those with experience of genital oedema specific education were more likely to bandage, whereas those without genital oedema education were more likely to try to manage the swelling with compression garments and MLD (massage). In treating lymphoedema, compression bandaging has repeatedly been shown to be more effective than garments and MLD, if correctly applied and maintained (King et al, 2012).
A third of health professionals had used antibiotics as part of treatment of genital oedema. Infection (cellulitis) can be problematic with genital oedema and recurrence is common (Hara et al, 2016). Hara and Mihara (2020) reported that in women with post-cancer lower limb and genital lymphoedema, 31% (9/29) of those with a history of cellulitis had antibiotic-resistant bacteria, compared with 11% (2/18) of those with no history of cellulitis (P = 0.12). Further study of cellulitis associated with genital oedema in different patient types would improve the detail of health professionals' education. Similarly, a third of health professionals had used wound dressings as part of their treatment. Little research has been done regarding the coexistence of wounds and genital oedema but surgical intervention, such as for buried penis, can be complex (Smith-Harrison et al, 2020) and incidence of postoperative wound complications high (Voznesensky et al, 2017). Management of wounds in genital oedema is rarely part of current genital oedema education and relies largely on transferable knowledge from other aspects of nursing. Although it seems likely that many lymphoedema specialists using wound dressings in these findings came from a nursing rather than a therapist background, the data were not exclusive to nurses. Deeper analysis will identify whether there are particular inter-professional differences in education need. As identified by over half the respondents, collaboration with experts in urology and gynaecology (pelvic health) would improve this knowledge base for nurses and therapists managing genital oedema.
In relation to topics that showed most (and least) difference between those with and without genital oedema education, providers/educators would probably recognise the topics ranked high in Table 1 as being the content of their courses. The much lower difference regarding male and female pelvic anatomy may indicate insufficient teaching within genital oedema education, however, this may be generic transferable knowledge, the measurement method used would not be able differentiate this. Similarly, high differences do not confer direct causality from the genital oedema education.
Reflecting the contemporary need for accessible resources and different ways of learning, almost all respondents indicated a wide range of learning formats was essential. Somewhat surprisingly, printed materials such as leaflets and booklets were second only to an e-learning package. This may suggest that learning resources are as much about sharing information with patients and enabling self-management, as they are for the health professionals to improve practice decisions. Similarly, the parity between ‘videos by experts for health professionals' and ‘video prescriptions for patients' might reflect the same shared-care approach, although they may not be the same 60% of respondents. Over half indicated that collaborative events with other specialities such as urology was essential. Despite the boundary-free space of social media and internet use, research has shown that health professionals continue to create communities of practice that reflect the tribal behaviours of clinicians, limiting potential knowledge sharing (Rolls et al, 2016). However, the findings here suggest that a significant proportion of lymphoedema nurses/therapists managing genital oedema anticipate educational benefit from collaboration. The potential patient benefit of shared learning for seamless work between urology/pelvic health and lymphoedema is worthy of evaluation.
Conclusions
In this survey of UK health professionals, lymphoedema nurses and therapists identified specific education need for the management of patients with genital oedema. Health professionals were, on average, less than ‘somewhat confident’ in their knowledge of genital oedema management. Individual education needs around compression, contemporary surgical and medical intervention and patient assessment were most common but a plethora of different topics was identified. There is a need for educational resources online, printed offline material and videos for health professionals and patients. In addition, collaborative events with urology/pelvic health specialists are considered essential to improve the quality of care for patients with genital oedema.
KEY POINTS
- Nurses and allied health professionals identified low confidence in their knowledge of the theory and practice of conservatively managing genital oedema
- In addition to current lymphoedema training programmes, specific supplemental education is needed to confidently manage patients with chronic genital oedema
- Compression of oedema in the genital area remains the most challenging aspect of managment
- Educational resources to supplement face-to face training need to be both online (e-learning, videos for patients and for professionals) and offline (leaflets, booklets and information folders)
- Collaborative events with urology/pelvic health specialists are essential to break down silos of knowledge that persist despite the development of communities on social media
CPD reflective questions
- Patients with genital oedema can present in almost any setting. Which patients in your setting are likely to have genital oedema and how might you support communication around its identification?
- How would you manage a patient with newly identified genital oedema in your work setting?
- Do you have local lymphoedema services and pelvic health services (urology and gynaecology) that you could access for advice for your patient? If not, consider how you would seek specialist knowledge and support.
- What can you do to break down silos of information in different specialities related to your work?


