A stoma is an opening in the abdomen created to divert waste matter from the digestive system or urinary tract. It may be needed to manage several conditions, including Crohn's disease, certain cancers and diverticulitis (Colostomy UK, 2022). Stomas are formed from the small intestine (ileostomy), large intestine (colostomy) or ureters (urostomy), and are prevalent in roughly 1 in every 335 people in the UK (Colostomy UK, 2022). Stoma nurses are an integral point of care for post-surgical clinical complications, which are particularly common within 1 year of surgery (Correa Marinez et al, 2021). Most frequently, these include hernia, bleeding, obstruction, necrosis, stenosis, leakage and other skin complications (Nastro et al, 2010; Shabbir and Britton 2010; Pearson et al, 2020). Stoma nurses remain essential to patients' adaptation to life with a stoma and addressing their ongoing needs, including support and empowerment for self-care (de Fries Jensen et al, 2023).
Stoma-related clinical complications have a substantial negative impact on health-related quality of life (HRQoL) (Davis et al, 2020; Jeppesen et al, 2022; Osborne et al, 2022). Peristomal skin complications (PSCs) are one of the most common post-surgical challenges (Salvadalena et al, 2020; Fellows et al, 2021; Maglio et al, 2021) and are multifactorial, including irritant dermatitis, mechanical injury, denuded skin and infection. The elevated risks of complications such as PSCs in the immediate post-discharge period after surgery are also associated with higher healthcare costs (Bassy and Libutzki, 2019).
In the UK, the lifetime stoma costs after colorectal surgery are about £8167 per person, excluding the cost of post-surgical adverse events (Pietzsch and Geisler, 2019). However, no studies in the UK have evaluated healthcare resource utilisation (HCRU) and costs in the immediate post-discharge period for people with new stomas from the perspective of the NHS. This study evaluated HCRU and costs in the 6 months following surgery for two groups of patients: those with new stomas and those with an established stoma beyond 6 months post-discharge who had had more than 6 months of follow-up.
Methods
Study design and data sources
This was a retrospective observational study. It used electronic health record data from the Clinical Practice Research Datalink (CPRD) database linked with hospital admissions data from the Hospital Episode Statistics (HES) database. The CPRD consists of anonymised health records from 397 GP practices, with coverage of about 4.6% of the UK population, considered to be representative of the population overall with respect to age and gender. The HES database provides data on all admissions to NHS hospitals and admissions to private hospitals or charitable hospitals, if paid for by the NHS. Linkage of CPRD records to HES data is available for 75% of the practices in England (equivalent to 58% of all CPRD practices). Clinical events in primary care are recorded using the ‘Read’ code clinical system for the CPRD database, and the International Classification of Diseases, Tenth Revision (ICD-10) is used in the HES database.
Study population
Adults (aged 18 years old and over) with evidence of a new or established stoma between 1 January 2009 and 31 December 2018 were included. All records were stratified by type of stoma: ileostomy, colostomy or urostomy. People ≤18 years old or those who were pregnant or had given birth during the study period were excluded, as were those with more than one type of stoma.
To focus on outcomes in the immediate post-discharge period, two cohorts were created. The New Stoma Group (0-6 months) comprised only those who had had a stoma formed during the study period; this group was observed for 6 months after discharge. Records had to include a procedure code for a new stoma, coding for the type of stoma, and a prescription for a stoma appliance. The index date for this group was the date of the surgery. The follow-up period started 1 day after discharge from hospital, and continued over 6 months post-discharge or until stoma reversal, death, last prescription for a stoma product or end of the study period, whichever occurred first. The follow-up period for the group did not include the hospital stay related to the stoma formation: this was because the dataset did not provide adequate details in the coding for stoma-specific product usage and procedures.
The Established Stoma Group (>6 months) comprised those with a stoma that had been created before or during the study period and who had had more than 6 months of follow-up time during the study period. Records had to have evidence of stoma product use during the study period and coding for type of stoma. The index date for the Established Stoma Group was the date of stoma surgery for those receiving a new stoma, or 1 January 2009 for those with established stomas (who had evidence of stoma product use but no coding for a new stoma procedure during the study period). The follow-up period started 6 months after the index date for those with a new stoma and 1 July 2009 for those with an established stoma, until stoma reversal, death, last prescription for a stoma product or the end of the study period, whichever occurred first.
Age- and sex-matched comparison groups were created for each stratified cohort (ileostomy, colostomy, urostomy) within the New Stoma and Established Stoma groups. The comparison groups were meant to represent the general population in the dataset who had no record of any stoma procedure or product use, and no record of pregnancy or childbirth during the study period. Candidates for the control groups could not be derived from comparable surgical cohorts as those used for the stoma groups due to informational limitations in the database and sample size concerns. Fifty matched controls per stoma patient were derived with the same analysis period as the corresponding stoma patient, based on the stoma patient's index date to end of follow-up, to account for temporal and contextual factors.
Variables and outcomes
Demographic and clinical characteristics included age, sex, ethnicity, reason for and timing of stoma creation, Charlson Comorbidity Index (CCI) score, comorbidities, number of people with temporary ileostomies or colostomies (indicated by reversal during the study period), follow-up time and records of deaths. Clinical variables included prevalence of cancer, renal failure (acute or chronic), skin conditions (including PSCs), mental health challenges, stoma appliance-related complications, fluid-related complications (including dehydration), sepsis, inflammatory bowel disease (including Crohn's disease and ulcerative colitis), and stoma-related complications (bleeding from inside stoma, ulcers on stoma).
HCRU and associated costs were based on visits to the emergency department (ED), all-cause and stoma-related healthcare provider visits (GP, nurse, psychiatrist, psychologist, physiotherapist, dietitian), inpatient admissions (elective or non-elective) and 28-day readmissions. HCRU and costs were reported for the 6-month post-discharge period for the New Stoma Group and annualised for the Established Stoma Group due to the inherent variability in follow-up time.
Stoma-related encounters were defined as those with a stoma-related code in the primary diagnosis position or a stoma procedure in any field for that encounter. Diagnostic urinalysis was captured, as were medications used to manage skin issues (topical corticosteroids, antifungals and antibiotics, and systemic antifungals and antibiotics), pain (opioids), and mental health issues (antidepressants).
Primary care costs from encounters in the CPRD were linked with corresponding unit costs from the Unit of Social and Healthcare Costs 2018/2019 (Curtis and Burns, 2018). Secondary care costs from the HES database were calculated using the Healthcare Resource Use Grouper Software linked with NHS 2018/2019 reference costs (NHS England, 2020). Costs of stoma products were not included because they were not available or could not be clearly defined in the databases (eg it was not possible to distinguish between use of a single product versus a box of products).
Statistical analysis
Descriptive statistics were used to summarise demographic and clinical characteristics, clinical outcomes, HCRU and costs. Records with missing age or sex were excluded from the analysis. Records with no HCRU were assumed to have no corresponding healthcare encounters and remained in the analysis; therefore, proportions of people with HCRU (and associated cost calculations) included all records in the denominator.
Mean differences in HCRU and costs were compared between stoma groups and matched controls using Student's t test (after normality was determined) with 95% confidence intervals (CIs). No imputation of missing data and no bootstrapping were performed. Analyses were performed using Db Visualizer v10.0.10 (www.dbvis.com) and R v3.5.1 (www.r-project.org).
Findings
Study population
A total of 8533 people were included in the New Stoma Group (<6 months), most of whom had a colostomy (61%; n=5237) followed by ileostomy (31%; n=2622), and urostomy (8%; n=674). People with a colostomy or urostomy were slightly older than those with an ileostomy (median age, 69 years versus 63 years, respectively (Table 1).
Table 1. Demographics and clinical characteristics, New Stoma Group (0-6 months) (n=8533)
| Colostomy | Ileostomy | Urostomy | ||||
|---|---|---|---|---|---|---|
| Colostomy (n=5237) | Controls (n=261 850) | Ileostomy (n=2622) | Controls (n=131 100) | Urostomy (n=674) | Controls (n=33 700) | |
| Age, median (years) | 69 | 69 | 63 | 63 | 69 | 69 |
| Sex, male, n (%) | 2639 (50) | 131 950 (50) | 1497 (57) | 74 850 (57) | 453 (67) | 22 650 (67) |
| Race/ethnicity, n (%) | ||||||
| White | 2637 (50) | 84 676 (32) | 1230 (47) | 39 369 (30) | 500 (74) | 11 251 (33) |
| Black | 22 (<1) | 1285 (<1) | 9 (<1) | 720 (<1) | 4 (<1) | 163 (<1) |
| Asian | 32 (1) | 2368 (1) | 33 (1) | 1323 (1) | 4 (1) | 292 (1) |
| Other, unspecified | 22 (<1) | 1416 (1) | 10 (<1) | 814 (1) | 5 (1) | 167 (<1) |
| Unknown | 2524 (48) | 172 105 (66) | 1340 (51) | 88 874 (68) | 161 (24) | 21 827 (65) |
| Stoma reversals, n (%) | 23 (<1) | – | 33 (1) | – | – | – |
| CCI score, mean | ||||||
| At index date | 1.51 | 0.38 | 1.30 | 0.32 | 0.58 | 0.38 |
| End of follow-up | 1.70 | 0.39 | 1.46 | 0.32 | 0.71 | 0.39 |
| Comorbidities recorded during study period, n (%) | ||||||
| Hypertension | 786 (15) | 2550 (1) | 242 (9) | 984 (1) | 121 (18) | 355 (1) |
| Dyslipidemia | 182 (3) | 819 (<1) | 67 (3) | 325 (<1) | 30 (4) | 107 (<1) |
| Ischaemic heart disease | 144 (3) | 1193 (<1) | 51 (2) | 513 (<1) | 20 (3) | 169 (1) |
| Diabetes | 303 (6) | 1746 (1) | 111 (4) | 737 (1) | 44 (7) | 255 (1) |
| Atherosclerosis | 6 (<1) | 26 (<1) | 6 (<1) | 13 (<1) | 0 | 3 (<1) |
| Anaemia | 50 (1) | 165 (<1) | 28 (1) | 57 (<1) | 5 (1) | 13 (<1) |
CCI=-Charlson Comorbidity Index
NB Proportions may not sum to 100% due to rounding. Stoma reversals refer to temporary stomas reversed within the study period
The Established Stoma Group (>6 months) included 9397 people, most of whom had a colostomy (65%; n=6076) followed by an ileostomy (26%, n=2464) and a urostomy (9%; n=857). The median follow-up time in the Established Stoma Group ranged from approximately 19 to 28 months across stoma types, and most people had coding for an established stoma (range, 60-71%) (Table 2).
Table 2. Demographics and clinical characteristics, Established Stoma Group (>6 months) (n=9397)
| Colostomy | Ileostomy | Urostomy | ||||
|---|---|---|---|---|---|---|
| Colostomy (n=6076) | Controls (n=303,800) | Ileostomy (n=2464) | Controls (n=123,200) | Urostomy (n=857) | Controls (n=42,850) | |
| Age, median (years) | 71 | 71 | 63 | 63 | 70 | 70 |
| Sex, male, n (%) | 2968 (49) | 148 400 (49) | 1344 (55) | 67 200 (55) | 575 (67) | 28 750 (67) |
| Race/ethnicity, n (%) | ||||||
| White | 3189 (52) | 100 165 (33) | 993 (40) | 36 785 (30) | 654 (76) | 14 259 (33) |
| Black | 17 (<1) | 1374 (<1) | 4 (<1) | 710 (<1) | 2 (<1) | 180 (<1) |
| Asian | 24 (<1) | 2507 (1) | 23 (1) | 1147 (1) | 5 (1) | 358 (1) |
| Other, unspecified | 16 (<1) | 1531 (1) | 8 (<1) | 783 (1) | 4 (<1) | 235 (1) |
| Unknown | 2830 (47) | 198,223 (65) | 1436 (58) | 83,775 (68) | 192 (22) | 27,818 (65) |
| Follow-up time, median, months | 24.1 | 24.1 | 18.9 | 18.9 | 28.0 | 28.0 |
| Stoma procedure timing, n (%) | ||||||
| Within study period | 1931 (32) | – | 704 (29) | – | 343 (40) | – |
| Outside study period | 4145 (68) | – | 1760 (71) | – | 514 (60) | – |
| Stoma reversal, n (%) | ||||||
| Within 6 months of index date | 75 (1) | – | 115 (5) | – | – | – |
| ≥6 months after index date | 22 (<1) | – | 24 (1) | – | – | – |
| CCI score, mean | ||||||
| At index date | 1.64 | 0.38 | 1.19 | 0.29 | 0.68 | 0.37 |
| End of follow-up | 1.99 | 0.45 | 1.39 | 0.34 | 0.98 | 0.44 |
| Comorbidities recorded during study period, n (%) | ||||||
| Hypertension | 685 (11) | 5104 (2) | 130 (5) | 1493 (1) | 114 (13) | 827 (2) |
| Dyslipidemia | 165 (3) | 1555 (1) | 37 (2) | 503 (<1) | 36 (4) | 270 (1) |
| Ischaemic heart disease | 182 (3) | 2333 (1) | 40 (2) | 732 (1) | 35 (4) | 391 (1) |
| Diabetes | 371 (6) | 3172 (1) | 89 (4) | 1042 (1) | 61 (7) | 544 (1) |
| Atherosclerosis | 12 (<1) | 59 (<1) | 1 (<1) | 18 (<1) | 1 (<1) | 12 (<1) |
| Anaemia | 60 (1) | 358 (<1) | 15 (1) | 90 (<1) | 6 (1) | 43 (<1) |
CCI=-Charlson Comorbidity Index
NB Proportions may not sum to 100% due to rounding. Index date was the date of the stoma surgery
Clinical outcomes
In the New Stoma Group, cancer was most prevalent among those with a colostomy or ileostomy (19% and 15%, respectively); renal failure was most prevalent in the urostomy subgroup (12%). In the Established Stoma Group, renal failure was most prevalent across all stoma types (ileostomy, 10%; colostomy, 11%; urostomy, 18%), followed by cancer in the colostomy (7%) and ileostomy (6%) subgroups. Skin conditions were prevalent in people in the Established Stoma Group, across stoma types (ileostomy, 4%; colostomy, 6%; urostomy, 7%).
Healthcare resource utilisation
Overall, significantly more people with stomas had at least one medical encounter compared with those in the matched control groups.
New Stoma Group
In the New Stoma Group, all-cause ED visits, GP visits, nursing visits, inpatient admissions and 28-day readmissions were all significantly more prevalent with all three stoma types compared with the matched controls (all P<0.0001; Figure 1a). Across all stoma types, around 20% of patients had coding for stoma-related nursing visits. All-cause nursing visits were observed in 67% of people with a colostomy, 66% with an ileostomy, and 72% with a urostomy (Figure 1a). Mean differences in all-cause nursing visits compared with controls ranged from 52% to 56%. People with colostomies and ileostomies in the New Stoma Group had significantly more visits to a specialist health professional than matched controls. The proportion of individuals in the stoma group requiring medication for skin issues was also much greater compared with the controls (colostomy, 19% versus 4%; ileostomy, 18% versus 3%; urostomy, 19% versus 4%), as was the proportion requiring systemic medications (colostomy, 75% versus 14%; ileostomy, 71% versus 12%; urostomy, 75% versus 15%).
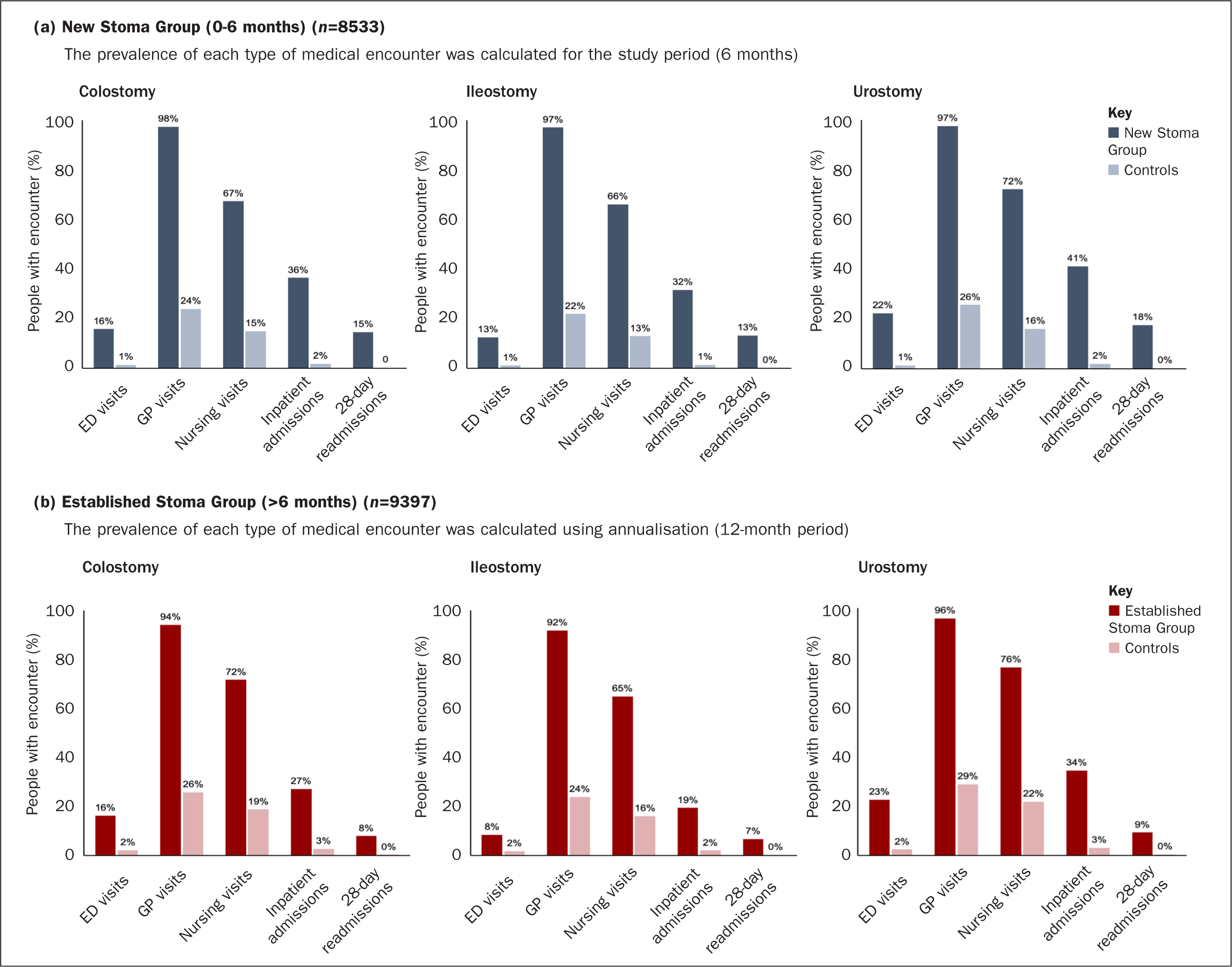
Established Stoma Group,
In the Established Stoma Group, all HCRU outcomes were significantly higher for people with a stoma compared with matched controls across all three stoma groups (all P<0.01; Figure 1b). Across stoma types, 14–18% of patients had coding for stoma-related nursing visits (colostomy, 18%; ileostomy, 14%; urostomy, 16%), and around three quarters had all-cause nursing visits (colostomy, 72%; ileostomy, 65%; urostomy, 76%) (Figure 1b). Mean differences in all-cause nursing visits compared with controls ranged from 49% to 54%. Nearly all individuals with stomas had all-cause GP visits (colostomy, 94%; ileostomy, 92%; urostomy, 96%), and between one fifth and one third had inpatient admissions (elective and non-elective) (colostomy, 27%; ileostomy, 19%; urostomy, 34%) during the study period. As with the New Stoma Group, those with stomas received more medications for skin issues than the controls (colostomy, 24% versus 5%; ileostomy, 22% versus 4%; urostomy, 25% versus 6%) and for systemic medications (colostomy, 73% versus 17%; ileostomy, 66% versus 14%; urostomy, 73% versus 18%).
Costs
Costs were significantly higher for people with stomas compared with matched controls in both the New and Established stoma groups, driven primarily by inpatient admissions (Figure 2a; Figure 2b). Costs in the New Stoma Group were £3227 per person for colostomy versus £99 for controls; £2576 per person for ileostomy versus £78 for controls, and £2850 per person for urostomy versus £110 for controls. Inpatient admissions accounted for 69% to 72% of all costs for people with stomas, compared with 43% to 46% of costs for matched controls, which had greater proportions of costs attributable to GP visits (25-27% for controls versus 8-10% for people with stomas).
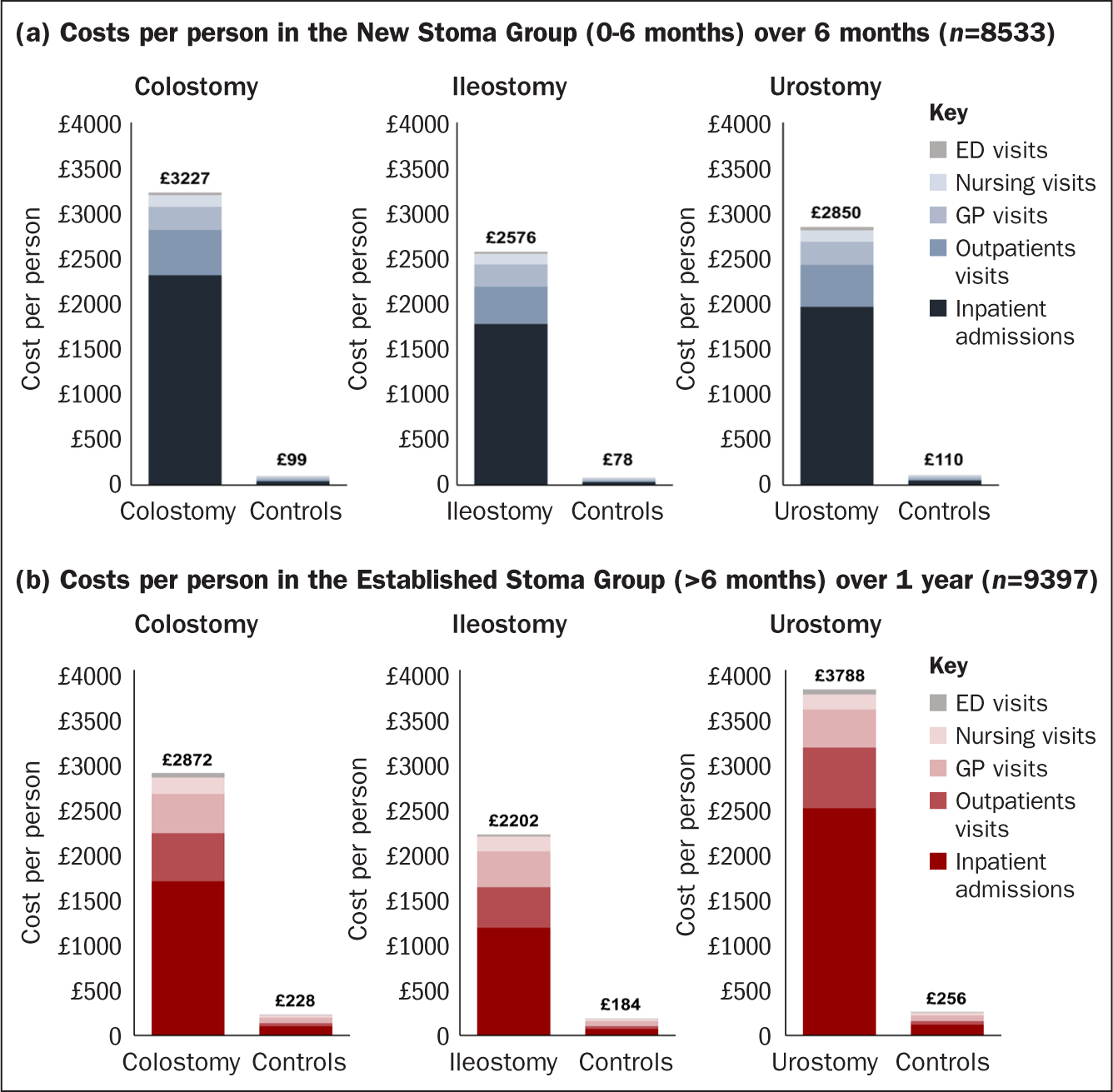
New Stoma Group
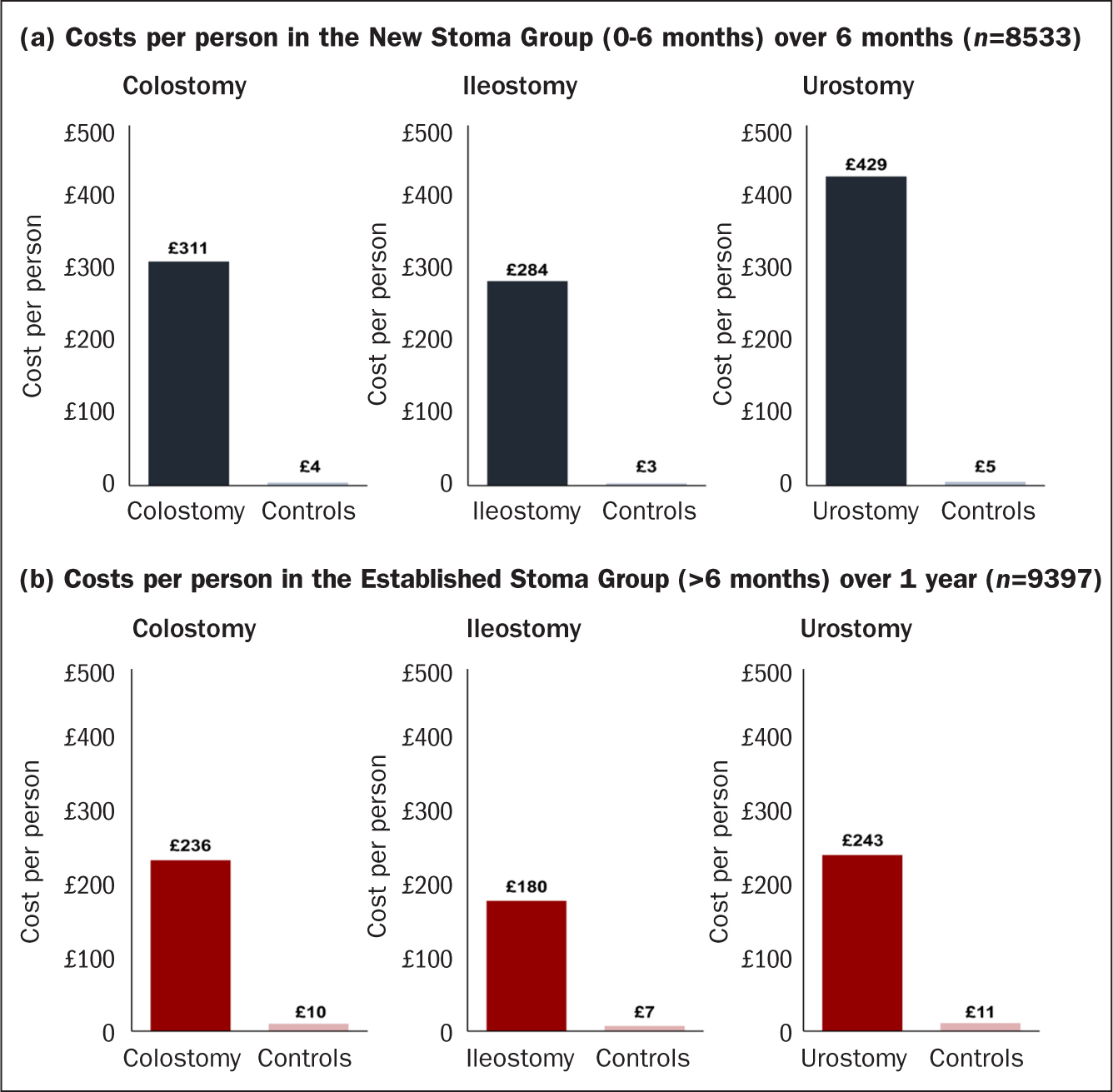
Despite the high occurrence of nursing visits, costs associated with all-cause nursing visits in the New Stoma Group were low, ranging from £120 to £128 per patient across stoma types. In the New Stoma Group, costs by stoma type versus controls per person over 6 months of care are illustrated in Figure 2a. Costs per person associated with 28-day readmissions were significantly higher for people with stomas across all types (Figure 3a).
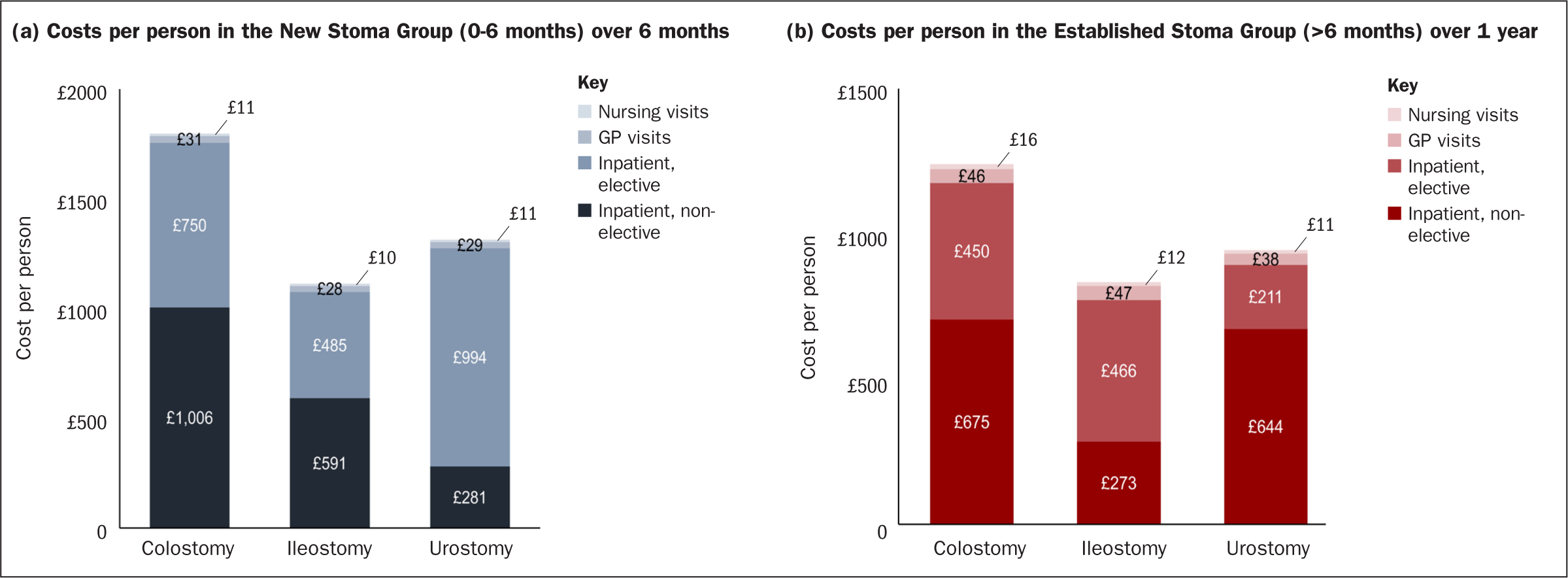
Non-elective inpatient admissions made up the greatest proportion of stoma-related costs among those with colostomies (56%) and ileostomies (53%), while for those with urostomies, the greater proportion of costs was for elective inpatient admissions (76%) (Figure 4).
Established Stoma Group
In the Established Stoma Group, total costs were significantly higher for people with stomas compared with the matched controls, and highest among those with a urostomy. As with the New Stoma Group, admissions costs were primarily driven by inpatient admissions: 54-66% of the total for individuals with stomas compared with 40-46% of total admissions costs for matched controls. Annualised costs associated with all-cause nursing visits were low, ranging from £160 to £179 per patient, despite the high occurrence of nursing visits across stoma types.
Costs per person associated with 28-day readmissions were significantly higher for the stoma groups than for the matched controls in the colostomy group (£236 versus £10; mean difference, £226; P<0.0001), ileostomy group (£180 versus £7; mean difference, £173; P<0.0001);, and the urostomy group (£243 versus £11; mean difference, £232; P<0.0001) (Figure 3b). Non-elective inpatient admissions comprised the greatest proportion of stoma-related costs for people with colostomies (57%) or urostomies (71%), and for those with ileostomies the highest costs were for elective inpatient admissions (58%) (Figure 4).
Discussion
This study used linked health record and hospital admissions data to estimate the post-discharge and ongoing HCRU and healthcare costs associated with stomas in the UK. Compared with age- and sex-matched controls from the general population, people with stomas required significantly more health services, with higher associated costs. Although this finding may be expected, the economic burden of stomas in the UK has not been well quantified in the literature. In the immediate 6-month post-discharge period, all-cause healthcare costs were driven primarily by inpatient admissions.
Despite a high occurrence of nursing visits across stoma types, the associated costs were low, suggesting that this is likely a high-value post-discharge point of care for people with new or established stomas. Indeed, people with stomas require substantial ongoing support from stoma nurses, and have reported a need for a greater frequency and longer duration of stoma-related nursing visits (Bowles et al, 2022). Even remote consultation visits between the stoma nurse and individuals with stomas, particularly those with new stomas, may provide additional support that could minimise more costly office or hospital visits (Augestad et al, 2020; Oliquiano et al, 2021; Brewer and Coleman, 2022).
These findings are consistent with prior reports, which have collectively suggested a potential need for improved stoma management in the community setting. Clearer post-discharge clinical management pathways may help to prevent complications, which is consistent with historical reports of the impact and requirements of having a new stoma and the importance of prevention (O'Connor, 2003; Borwell 2009; Taylor et al, 2012). For example, Tyler et al (2014) reported stoma patients to be substantially more likely to have an acute-based encounter within 30 days of discharge compared to those without stomas, most often due to post-surgery infection, renal failure and dehydration, particularly among those with ileostomies (Tyler et al, 2014). Similarly, a US study reported that people with new stomas were three times more likely to be readmitted 30 days after colorectal surgery due to difficulties with managing the new stoma or an increased risk of dehydration/fluid depletion problems (Wick et al, 2011).
Dehydration has been cited as a prominent reason for 30-day readmissions following ileostomy, and skin-related complications as a substantial post-discharge complication in large systematic literature reviews (Steinhagen et al, 2017; Justiniano et al, 2018; Vogel et al, 2022). This further emphasise the value of nursing care for this cohort of patients, particularly in the post-discharge setting, which can contribute to a reduction in complications and associated costs, including 28-day readmissions. Greater detail in coding practices would likely be required to further elucidate the detailed impact of primary care on patient outcomes and subsequent HCRU and costs.
It should be noted that findings from this study related to PSCs and leakage appeared to be slightly different from previous studies, possibly due to the differences in methods used to identify and quantify skin-related complications. The prevalence of skin-related HCRU in this study was approximately 5% across stoma types. Previous studies have reported prevalence estimates of PSCs ranging from 18% to 60%, also likely attributable to differing definitions of PSCs, administrative coding, and variability in patient reports (Herlufsen et al, 2006; Taneja et al, 2019). The latter study reported that 36% of people with stomas had a PSC within 3 months of surgery, and had a higher incidence of readmissions and extended hospital stays (Taneja et al, 2019).
These findings should be considered in the context of certain strengths and limitations. A large study sample with real-world data from health records and hospitals via the linked CPRD-HES data set offered a holistic approach to capturing healthcare activity and costs. The CPRD database is representative of the UK/England population with respect to age and sex, which supports generalisability to the larger population.
Challenges related to specific aspects of the CPRD data set should be noted, including incomplete or missing data due to imperfect coding practices and varying definitions of diagnoses and other clinical details (Herrett et al, 2015; Wolf et al, 2019). As a result, stoma product costs in the acute and community settings could not be accurately identified and therefore could not be included, which would be an important component of future work. Specifically, use and costs of stoma products were missing, and there was inconsistency in the recording of quantities (whether the coding referred to a single item or a box of items), which prevented the creation of a clean, reliable dataset of stoma products for analysis. Accurate quantification of stoma product use and understanding the subsequent HCRU and costs would be of particular interest for future data sources and analyses.
Some HCRU activity for both the stoma and control groups may have been underestimated due to coding issues and because some data collected in the community setting may not be captured in the HES database. However, the underestimation of stoma-related costs would likely have been disproportionately greater due to the level of morbidity observed in the stoma groups. The underestimation of both stoma-related and all-cause outcomes due to coding bias was expected.
The comparison groups were included in this study to contextualise the overall economic burden associated with people with a new or established stoma. Deriving the comparator groups from matched individuals with comparable underlying conditions and/or those who had undergone anterior resection was considered. Although these populations would likely be more homogenous in terms of baseline demographics, the sample sizes would have been much smaller and unfeasible for some of the cohorts. People undergoing stoma surgery would still be expected to have more severe underlying conditions compared to those without a stoma. Therefore, the ability to attribute HCRU and cost differences to the stoma alone would have remained difficult since potentially unobservable differences in underlying disease, comorbidities and other factors would almost certainly have been present.
Conclusions
This study demonstrates the substantial economic burden associated with stomas in the UK from an NHS perspective, driven largely by non-elective hospital care. Future research exploring potential improvements to post-discharge follow-up and access to specialised stoma care in the community is warranted. The economic burden of stomas characterised in this study emphasises the high value of primary care in the post-discharge setting for people with stomas, their families and society.
KEY POINTS
- People with stomas require significantly more healthcare services, and incur higher associated costs, than age- and sex-matched controls
- In the immediate 6-month post-discharge period, all-cause healthcare costs were driven primarily by inpatient admissions
- This study reported significantly more interactions with psychiatrists and psychologists, and greater use of antidepressants, by people with stomas compared with matched controls
- Nurses are integral in the post-discharge care of people with stomas, but stoma-specific healthcare resource utilisation and associated costs may not be adequately captured in health records and hospital encounter data
CPD reflective questions
- How can the nursing community help to reduce healthcare resource utilisation and costs related to follow-up care within the first 6 months following new stoma surgery?
- How does the incidence of complications observed in this dataset compare with your experience, and how might coding practices impact any disparity between real-world research and practice?
- How can you, as a nurse, help address the likely underestimation of stoma-specific care in medical records and hospital encounter data?


