Urinary catheterisation is used across a range of clinical indications in a variety of patients. To provide optimal care for patients, it is necessary to consider their suitability for catheterisation and constantly review the need for catheter usage (Royal College of Nursing (RCN), 2021). Catheterisation incidence varies between hospital and community (Shackely et al, 2017); therefore, it is essential to carefully plan the transition of care between settings as it can be problematic if nursing staff have not received appropriate education to manage this (Seymour, 2007).
Across healthcare, most hospital discharges proceed as intended, but issues can and do occur. Patient information passed from the hospital to community care can be incomplete, unclear and/or delayed (Hesselink et al, 2013). Incorrect discharge may be a contributing factor for hospital readmission. In 2017, a report from the charity Healthwatch showed that between 2012/2013 and 2016/2017, the number of emergency readmissions rose from 372 805 to 457 880 in England, and emergency readmissions within 24 hours of discharge rose from 49 529 to 63 964 (Healthwatch, 2017). Recent data from the NHS Clinical Commissioning Group Outcome Indicator Set indicate that the indirectly standardised percentage rate of emergency readmissions within 30 days of discharge from hospital was 14.4% for England, and this figure has been increasing over the past 5 years (NHS Digital, 2020a).
The recent policy and operating model from the NHS Hospital Discharge Service establishes four distinct pathways for discharging patients. These range from pathway 0, which encompasses 50% of people (simple discharge, no formal input from health or social care needed once home) to pathway 3, which includes 1% of people (patients require ongoing 24-hour nursing care, often in a bedded setting). Patients receiving urinary catheterisation would typically use pathway 1: support to recover at home; able to return home with support from health and/or social care. This discharge pathway includes 45% of people (Department of Health and Social Care, 2021).
With the aim of determining the different opinions of nursing staff on the discharge process and its associated challenges, a survey was created and sent to a wide range of nurses and to subscribers of three nursing journals. The aim of the survey was to gain insights into the structure/flow of the patient journey and to identify the challenges and frustrations that exist on the journey between hospital and community care.
Methods
Qualitative interviews
To determine applicable content for the survey, a series of invitational qualitative interviews were performed to gauge opinion of relevant health professionals. Invitations for the qualitative interviews were sent to a range of acute and community stakeholders across roles including ward nurses, continence advisers/managers, operational/clinical service leads, urology nurse specialists, clinical improvement leads, directors of continence services and district nurses/leads. Twenty-three interviews were performed by the authors and additional members of the BD team using Microsoft Teams across a period of 8 weeks.
Survey creation
Using the outputs of the qualitative interviews, the authors, along with additional members of the wider BD urology and continence team, created an anonymous 11-question questionnaire to gain insight into the perception differences between community and hospital staff.
Survey delivery
The survey was sent out by the BD team to a wide range of acute/community nurses and to the subscriber list of the Journal of Community Nursing, the Journal of General Practice Nursing and Wound Care Today from 26 January 2021. The survey was accessed via an email to the subscribers of those journals. The survey link was accessible for 2-3 weeks after receipt of the email.
Survey data
Results from the survey were correlated by the authors and additional members of the BD team. Results from the correlation were overseen by an independent market research professional.
Results
Demographics
The online survey was sent out to 56 818 health professionals from 26 January 2021. The survey questions are shown in Box 1. Survey recipients included subscribers to the Journal of Community Nursing, the Journal of General Practice Nursing and Wound Care Today and personally emailed acute/community nurses. The survey was closed on 8 February 2021 and usable responses were received from 505 respondents. This equated to a survey response rate of 0.89%. Of the 505 respondents, 76% classified their place of work as community, 17% hospital and 7% both community and hospital.
Box 1.Example survey
- Where do you work?
- Please briefly describe the discharge process for patients requiring urology/continence products (catheters, bags but not pads) in your organisation.
- What role do you play in the discharge process?
- In your organisation, who is the ultimate decision-maker for the hospital discharge process involving catheter patients? (eg Discharge Coordinator, Lead Nurse, Urology Dept, Medicines Management, Director of Nursing etc)
- What are your top 3 challenges and frustrations with hospital discharge? (patients with a catheter only)
- How would you rate the quality and completeness of the patient documentation? (eg information supplied on discharge letter)
- Does your organisation use catheter passports?
- What self-care support is provided to the patient? (such as how to change a leg bag, catheter care etc)
- On discharge, how would you rate the supply of stock that patients are provided to take home? (leg bags etc)
- Would you use a free home delivery service for on-going patient supplies? (catheters, bags etc)
- Is there any other feedback or thoughts you would like to share on hospital discharge?
Overview of the discharge process
Survey participants were asked to describe the discharge process for patients requiring urology/continence products (including catheters and bags but excluding incontinence pads) within their organisation. Nearly a third of all respondents (141 of 489 responses) mentioned the word ‘referral’, 17% used the phrase ‘some supplies’ and another 17% mentioned ‘a process’. Eleven percent of responders indicated that there were ‘poor supplies’ and 8% of responders referred to a ‘dispensing appliance contractor/DAC’. A small number of respondents mentioned additional words such as ‘varied experience’, ‘passport’, ‘limited advice’ and ‘poor information’ (<5% each). Responses mentioning ‘referral’ were most common across community, hospital and hospital/community responders. Perceptions around the levels of provided supplies differed between community and hospital responders; 14% of community responders mentioned ‘some supplies’ and 14% of community responders mentioned ‘poor supplies’ whereas 29% of hospital responders mentioned ‘some supplies’ and 0% of hospital-based responders mentioned ‘poor supplies’.
Responders' role in the discharge process differed based on their place of work. For community-based responders, 37% (136 of 371 responses) accepted the patient's referral and 32% indicated they had no role in the discharge process. For hospital-based responders, a third of responses (28 of 85 responses) indicated that they were involved in the assessment of patients, 19% were involved in providing advice and/or education, 19% were involved in another role and 11% of responders were involved in overall care. The highest proportion of hospital and community staff stated their role was to discharge patients (35%).
The role of hospital, community and combined hospital and community staff in the discharge process is shown in Figure 1.
Figure 1. Role of the responder in the discharge process
Urology decision making
On the question of who is the ultimate decision maker for the hospital discharge process for urinary catheter patients, just over a quarter of hospital responders (22 of 86 responses) considered the ultimate decision maker for the hospital discharge process to be the discharge coordinator. Some 24% of hospital responders considered the ultimate decision maker to be the lead nurse and less than a fifth of responders considered the ultimate decision maker to be a doctor/consultant. Ten percent of hospital responders considered the multidisciplinary team to be the ultimate decision maker in the discharge process, while 9% classified the urology department as the ultimate decision maker. The highest proportion of community responders (114 of 366 responses) did not know who was the ultimate decision maker for discharge. Some 17% believed that the ultimate decision maker for discharge was the discharge coordinator, 12% assumed that it was the lead nurse and 13% of community responders indicated that the ward/hospital was the ultimate discharge decision maker. Overall, nearly a quarter of all responders (118 of 486 responses; n=86 hospital, n=366 community and n=34 hospital and community) did not know the ultimate decision maker within their organisation, 19% believed that the ultimate decision maker was the discharge coordinator and 15% indicated that the ultimate decision maker was the lead nurse.
Challenges/frustrations with hospital discharge
Recipients were asked for their top three challenges and frustrations with hospital discharge. The most frequently described challenges and/or frustrations are shown in Table 1.
Table 1. Challenges associated with the discharge process
| Challenges | Percentage of overall responders |
|---|---|
| Product supply issues | 29% |
| Information issues | 28% |
| Lack of advice/education | 21% |
| Referral issues | 11% |
| Time pressures | 4% |
| Passport issues | 4% |
| Trial without catheter issues | 4% |
Regarding perception of the quality and completeness of patients' documentation (eg the information supplied with the discharge letter), 70% (261 of 375 responses) and 30% of community staff categorised the documentation as ‘poor’ and ‘adequate’ respectively. In the hospital setting, some responders classified the patient documentation as excellent (13 of 85), but most responders (65%) classified the documentation as adequate. For the remaining 20%, documentation was considered poor. In staff working across both hospital and community settings, most respondents classified the documentation as adequate (50%) or poor (38%).
Seventy per cent of community responders (263 of 378 responses) indicated that they used catheter passports within their community setting, 26% of responders indicated that they did not use catheter passports and 5% were unsure. In the hospital setting, just over half of responders (47 of 85) used catheter passports within their centre, 31% did not and 14% did not know. In responders who worked in both settings, 59% (20 of 34 responses) indicated their organisation did use catheter passports, 24% of responders' organisations did not and 18% were unsure about their use within their organisation. Overall, two thirds of respondents' organisations used catheter passports (330 of 497 respondents), 26% of respondents' organisations did not use catheter passports and 7% of respondents did not know if their organisations used catheter passports.
Product supply concerns
Across all responders, very few rated the supply of product stock with which patients are provided on discharge as excellent (2%) or good (3%). Some 11% of responders rated discharge stock as adequate, while the greatest number (64%) of responders rated the stock as minimal. A fifth of responders indicated that patients were provided with no stock on discharge. There were different opinions of stock issues between community and hospital staff. Only one of the community responders rated the supply of stock as either ‘excellent’ or ‘good’, and 7% (6 of 87) and 16% of hospital responders rated the supply of stock as ‘excellent’ and ‘good’ respectively. The rating of the opinions across supply stock by responders is shown in Figure 2.
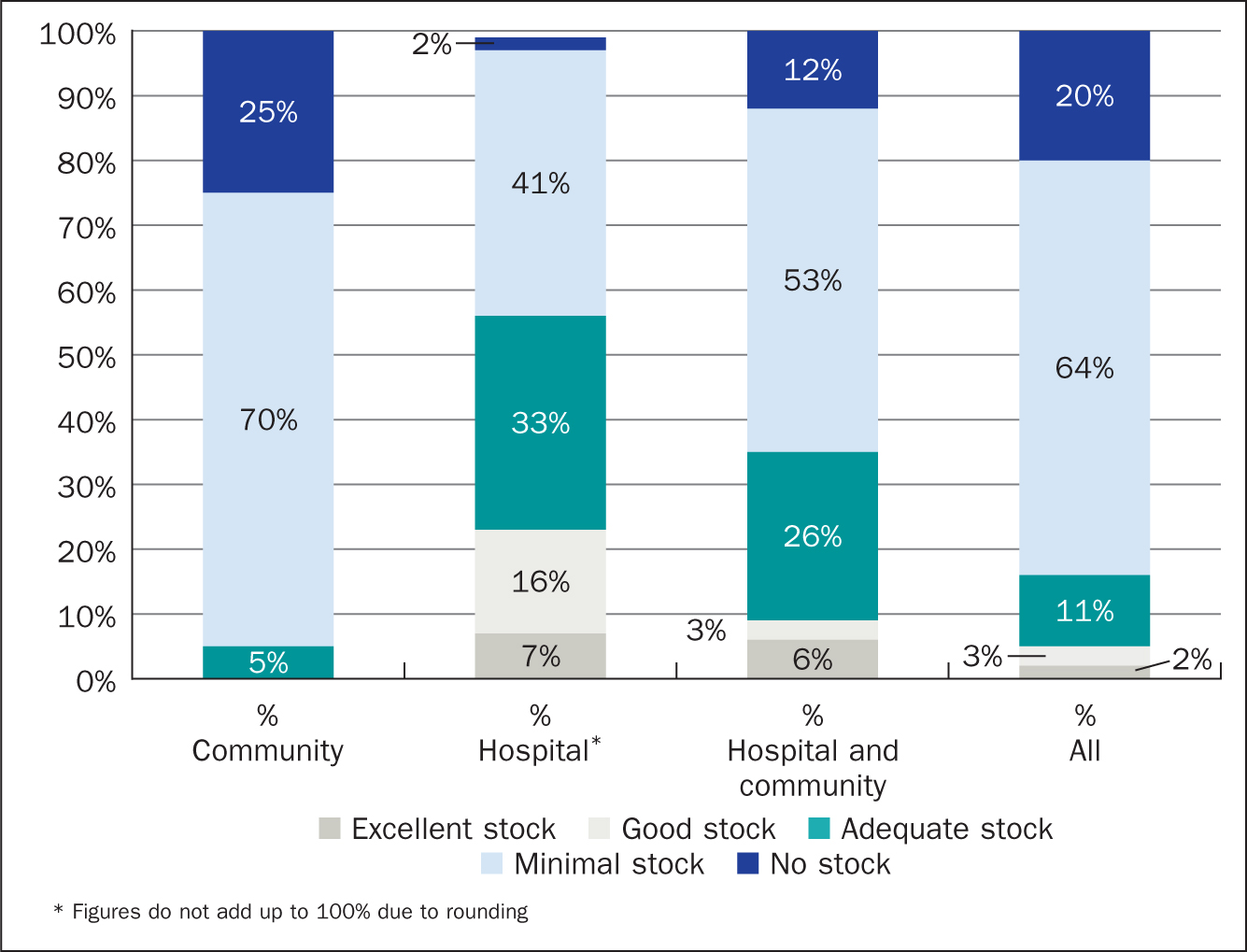 Figure 2. Perception of stock supplied to patients across survey responders
Figure 2. Perception of stock supplied to patients across survey responders
Across both community and hospital-based responders, there was an overall positive opinion towards a free home delivery service for ongoing patient support and supplies such as catheters/bags as shown in Table 2. Some 76% of community-based responders (286 of 376 responses) indicated that they would use a free home delivery service, although some would not (6%). Some 18% of community responders answered ‘maybe’. Sixty-eight per cent of hospital-based responders (59 of 87) indicated that they would use a free home delivery service, although 9% stated that they would not use a free home delivery service. In responders who work across both hospital and community settings, over half of responders (19 of 34) indicated that they would use a free home delivery service, although 9% suggested that they would not use a free home delivery service (35% of responders answered maybe to this question). Overall, 73% of responders (364 of 497 responses) indicated that they would use a free home delivery service for ongoing patient support and supplies.
Table 2. Attitudes of survey responders towards a potential free home delivery service
| Overall | Hospital | Community | Hospital and community | |
|---|---|---|---|---|
| Yes | 73% (364/497) | 68% (59/87) | 76% (286/376) | 56% (19/34) |
| No | 9% (32/497) | 9% (8/87) | 6% (21/376) | 9% (3/34) |
| Maybe | 20% (101/497) | 23% (20/87) | 18% (69/376) | 35% (12/34) |
Patient self-care advice/education
The perception of the responders was of an overall lack of advice/education regarding self-care for patients. On the question of what self-care support is provided to the patient, 24% of all responders (120 of 498 responses) categorised support as minimal, 11% of responders indicated there was no support provided and a further 11% indicated the level of advice varied. Few responders indicated that either ‘some’ (8%) or ‘good’ self-care advice was provided (6%). Thirteen per cent of responders mentioned the community team with respect to self-care support and 15% of responders provided a description of the materials for self-care available to patients. Community and hospital responders differed in their opinion regarding self-care provided. Some 12% (46 of 378 responses) and 28% of community-based responders classified the self-care support provided as ‘none’ and ‘minimal’ respectively, whereas only 6% (5 of 86) and 7% of hospital responders classified provided self-care support as ‘none’ or ‘minimal’, respectively.
Discussion
This invitational survey assessed opinion from a range of nurses across the UK to gauge their perspective of the process of hospital discharge and its associated challenges and the transition into community care. The management of urinary catheters is a significant component of the time burden on nurses in the community (Prieto et al, 2020). As would be expected, opinions differed between hospital and community staff. Overall, the opinions of community staff were more negative around the discharge process and post-discharge care and materials compared with hospital staff.
In this study, 13% of community nurses mentioned that patients were discharged with poor supplies and 33% of community nurses raised a lack of supplies as their biggest challenge. On examination of individual response data, it is of concern that within the individual responses from community nurses, it was mentioned that a number of patients were discharged with no products. The usual recommendations for hospital discharge indicate that patients should have sufficient products to last for at least 7 days (Birmingham NHS Foundation Trust, 2018) and RCN guidelines state that ordering of catheter equipment should be guided by local policy (RCN, 2021). The response from community staff was in contrast with hospital nursing staff where none of the responders highlighted the issue of poor supplies in the discharge process. Larger disparities in opinion were noted around the perception of the quality and completeness of patient documentation. Seventy per cent of community responders classified the quality and completeness of patients' documentation as poor compared with 20% of hospital responders. Community responses were noted around an absence of documentation/passport, staff not documenting whether the catheter is short or long term, an absence of transfer documentation and incomplete documentation around rationale for catheterisation and timings and procedural aspects. Despite these responses, it is important to highlight that the opinions of community staff may not match those of the patients in the care of the community nursing teams. A study by Oswald et al (2021), which examined the perceptions of 69 community nursing staff and 29 long-term catheter users, showed general satisfaction with the catheter service by both patients and staff.
Examination of the key frustrations and challenges for responders demonstrated the ongoing concerns around lack of product supply for community-based nurses (raised by 33% of responders). Individual comments from community nurses indicated that they are required to remedy issues that they feel are not necessarily within the remit of community care, notably an inadequate provision of initial stock. Additionally, community nurses felt that the information that they receive about patients is inadequate, with this being of particular concern regarding the provision of ongoing care. Despite these opinions, the perception of use of catheter passports was high across all settings' responders, with 66% of responders noting that catheter passports were used within their organisation. Data from the recent Community Urinary Catheter Management study, which included 49 575 patients (with 5352 patients with an indwelling catheter) showed that only 13% of patients had a catheter passport in place, but these patients were significantly more likely to have an active removal plan (Prieto et al, 2020).
The results from the survey show the difficulties and challenges associated with the discharge process Figures 3aandb provide an overview of the particular challenges for nurses at different stages of the discharge and ongoing care process. Responding to these challenges is a key focus for improving patient care and a number of strategies are available. A more connected discharge process may have the potential for benefits across healthcare resourcing. A study of patients attending secondary care services showed that a proportion of patients with long-term catheters who attended the accident and emergency department for catheter issues could have been treated in the community (Tay et al, 2016).
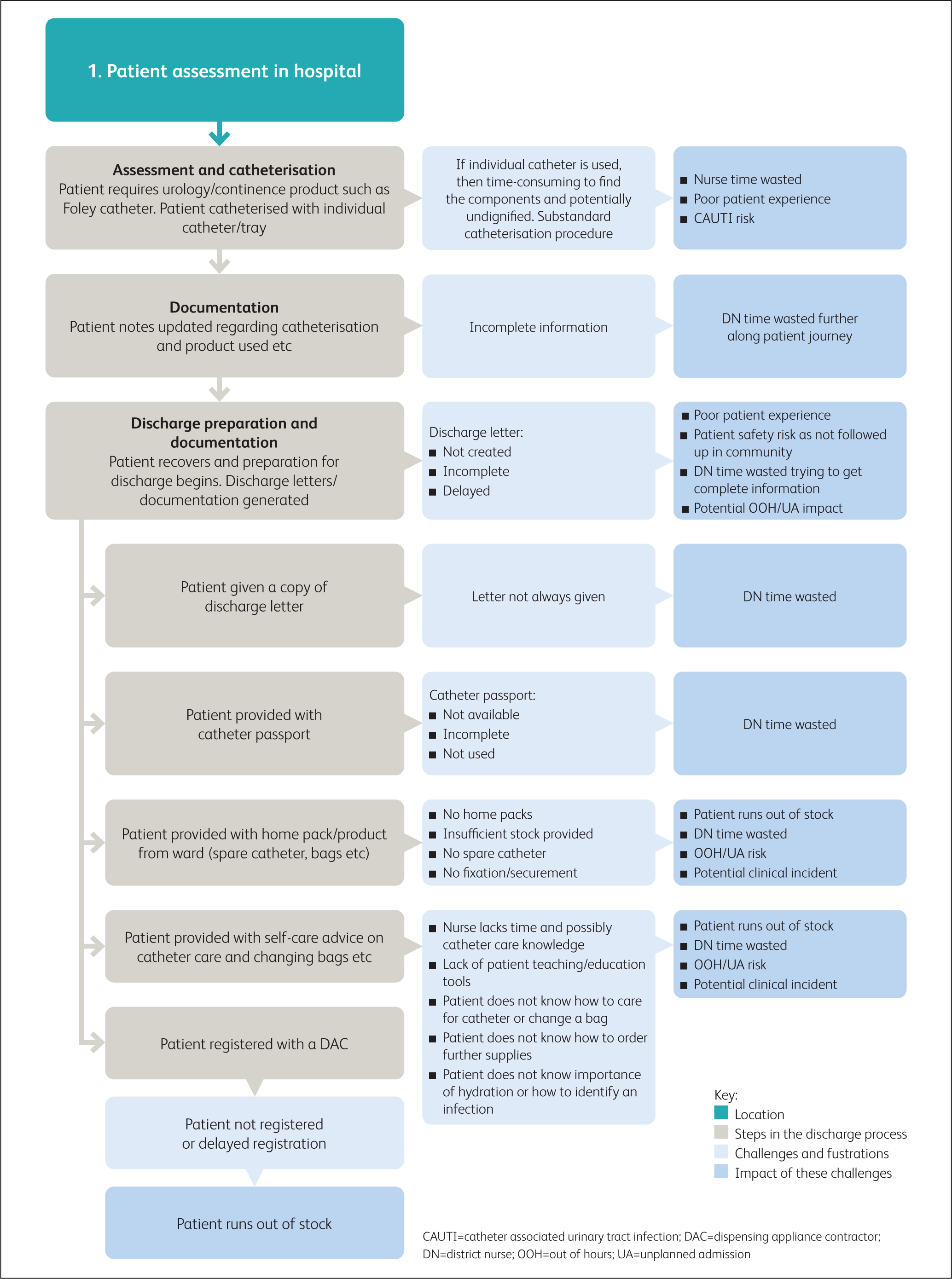 Figure 3a. Overview: Patient assessment in hospital
Figure 3a. Overview: Patient assessment in hospital 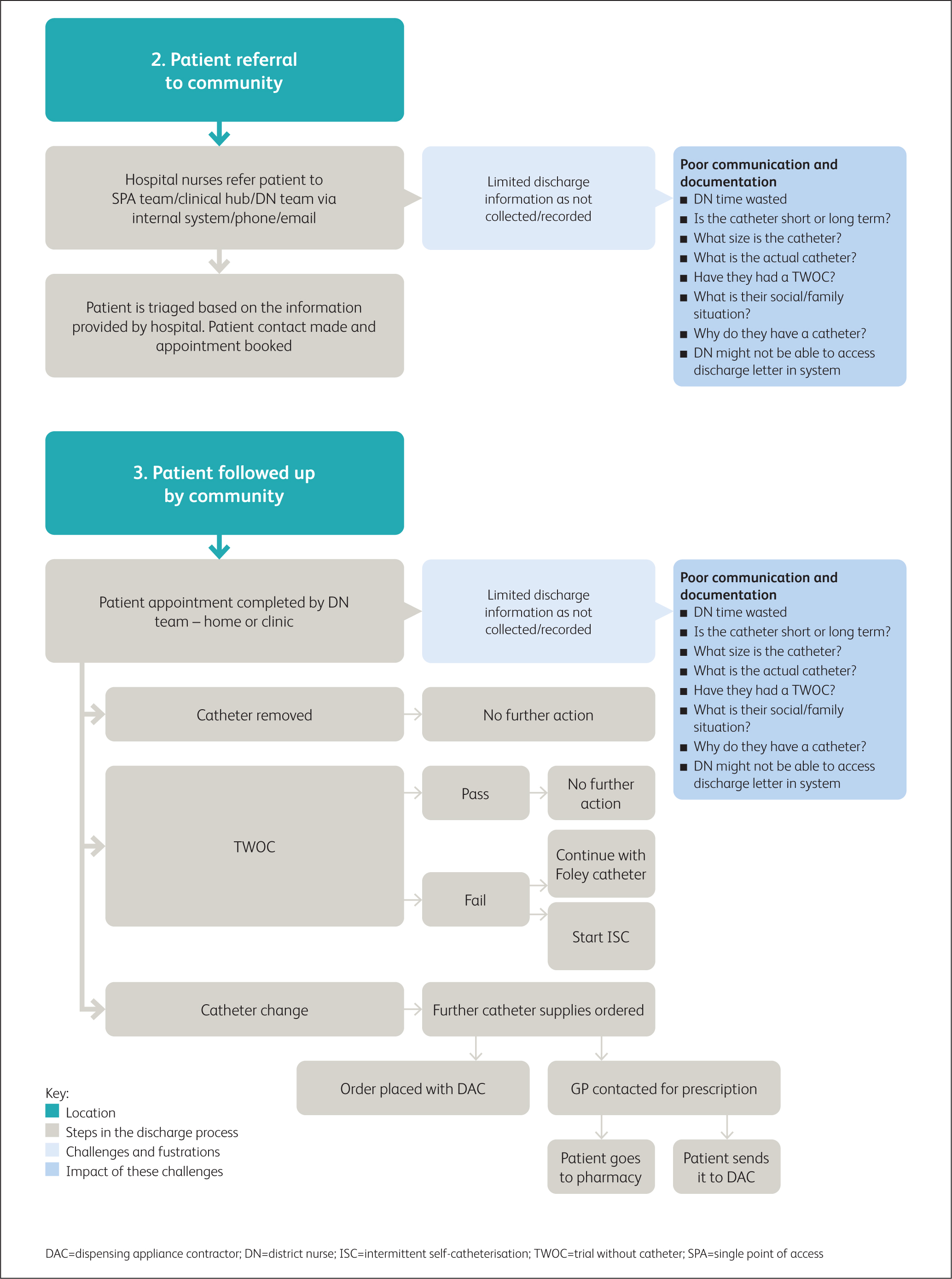 Figure 3b. Overview: Patient referral to community
Figure 3b. Overview: Patient referral to community
A key perspective on the discharge process not covered within the remit of this survey is the perception of the patient. Despite being present in all hospital discharges, data indicate a lack of patient involvement throughout the discharge process (Bullock et al, 2017). Data examining the patient's perspective of the discharge process demonstrate an unmet need with respect to individualising the discharge process and focusing more on the patient's home situation (Ubbink et al, 2014; Krook et al, 2020).
This survey has certain limitations. The uptake rate for the initial qualitative interviews and the response rate for the survey were both very low. However, it must be taken into account that both the survey and the qualitative interviews were carried out during the COVID-19 pandemic which had a profound impact on healthcare resourcing and priorities throughout the world. A global survey on the impact of COVID-19 on urology services showed that 41% of hospital staff members had been diagnosed with COVID-19, which would have an obvious impact on urology services and their priorities (Teoh et al, 2020).
Results of this survey help to determine the perceptions of community and hospital nurses regarding the challenges that exist with the general hospital discharge process for patients with a urinary catheter. Through building a patient safety culture/system with healthcare workers, the combination of innovative and unique products with specialist clinical support and training will help to improve future patient journeys and avoid preventable infections (CAUTIs) and unplanned hospital admissions.
KEY POINTS
- A series of 23 qualitative interviews with a range of acute and community staff were carried out to determine applicable content for a survey
- The resultant survey was sent to the subscriber list of the Journal of Community Nursing, the Journal of General Practice Nursing and Wound Care Today; 505 usable responses were provided
- Overall, the opinions of community staff were more negative around the discharge process and post-discharge care and materials compared with hospital staff
- Product supply issues, information issues and lack of patient advice or education were the main challenges noted by the nurses with the discharge process
- There was a significant difference in perception of quality and completeness of patient discharge information between hospital and community staff
CPD reflective questions
- How do you feel the discharge process could be improved within your organisation?
- Do you feel the answers provided in this survey mirror your opinions as an acute or community nurse?
- What do you feel is your biggest challenge with the discharge process?


