Peripheral intravenous (IV) cannulation is the most frequently performed invasive hospital procedure globally, with peripheral IV catheters (PIVCs) being the most commonly used vascular access devices, which are vital in providing hospital treatment (Alexandrou et al, 2018; Davis et al, 2021). PIVCs provide peripheral access when there is no indication for central venous access (Moureau and Chopra, 2016). They are indicated for short-term peripheral IV access for up to 5 days, or 6–14 days if inserted using ultrasound guidance, a period that can be further extended in the absence of complications and removed when clinically indicated (Hallam et al, 2021). Despite the benefits, PIVCs continue to report high failure rates in the range of 35-50% (Helm et al, 2015). In addition, in the context of the authors' practice, prior to the implementation of extended-length PIVCs, local surveillance data demonstrated that 35% of patients were being referred to the vascular access team for a midline or peripherally inserted central catheter (PICC) solely because of poor access. These patients had experienced failed cannulations and required peripheral IV access for up to 7 days, prompting consideration for an alternative device.
PIVC failure can result in treatment delays, repeated cannulation attempts, depletion of veins, patient distress, avoidance of hospitals (Marsh et al, 2021) or the need for rescue procedures, which can include peripheral midlines (Moureau and Chopra, 2016), internal jugular cannulation, IV devices, central venous catheters or ultrasound-guided PIVCs (Pare et al, 2019). Importantly, up to one-third of adults who require a PIVC have difficult intravenous access (DIVA) (Whalen et al, 2017), putting the issue at the centre of practice. Obesity, oedema, chronic illness, hypovolaemia, IV drug use and vascular pathology predispose patients to DIVA (Egan et al, 2013). These patients require more cannulation attempts, more time to gain access and may need specialist intervention to obtain vascular access (Whalen et al, 2017). However, multiple failed cannulation attempts alone may not indicate DIVA, because success or failure can also be influenced by the skill of the inserter (Egan et al, 2013).
When no visible or palpable veins are present, the use of ultrasound guidance for cannulation is recommended (Gorski et al, 2021), and this is frequently used to insert PIVCs in patients with DIVA (Au et al, 2012; Fields et al, 2012; Duran-Gehring et al, 2016). Ultrasound provides vein visualisation beneath the surface of the skin (Moureau and Chopra, 2016), enabling vein identification, assessment of vessel characteristics and correct positioning of the catheter within the vessel. Despite the use of this technology, some studies continue to report variances in the success of ultrasound-guided PIVCs. More specifically, differences are reported on how long an ultrasound-guided PIVC can remain in place, improvements in time to cannulation and improving patient outcomes, casting doubt on the effectiveness and reliability of ultrasound-guided PIVC insertion (Fields et al, 2012; Duran-Gehring et al, 2016; Bahl et al, 2020).
Healthcare workers with specific training and experience in PIVC insertion such as vascular access teams, as discussed by Helm et al (2015), have higher first-time success rates and reduced complication rates. In addition, Whalen et al (2017) supported the view that dedicated difficult vascular access teams have increased insertion success, which reduces delays in treatment.
This article explores the implementation of an extended-length PIVC, inserted using ultrasound guidance, by a vascular access team for patients with DIVA. The use of extended-length devices enables deeper vessels to be reached and a greater length of catheter to reside in the vessel (Fields et al, 2012; Duran-Gehring et al, 2016). This article details success rates, device dwell times, complication rates and discusses the key factors in successful implementation.
Method
This evaluation took place across Aintree Hospital, Liverpool University Hospitals NHS Foundation Trust, in 2019, when the B Braun Deep Access longer length (50 mm and 64 mm) peripheral IV catheters became available – and these are the two devices discussed in this article. Data collection was undertaken between 2019 and 2022, with patients who had been referred to the vascular access team due to DIVA being offered an extended-length PIVC inserted using ultrasound guidance. Those referred included patients who required short-term peripheral IV access and had no visible or palpable veins, or those who had undergone multiple failed cannulation attempts. Patients were assessed by the IV specialist nurses according to the UK Vessel Health and Preservation Framework (Hallam et al, 2021). If no suitable veins for cannulation were identified with ultrasound, and central venous access or frequent blood sampling was required, an alternative vascular access device was placed.
The members of the vascular access team were nurses with 3–10 years of experience in ultrasound-guided vascular access device placement. The method of insertion was the catheter-over-needle technique using ultrasound, which involves following the needle tip while advancing the cannula and ultrasound probe alternately (Duran-Gehring et al, 2016), which reduced the risk of misplacement or dislodgment. The ultrasound probe was used in the transverse plane during placement, where the catheter tip was continuously visualised until at least two thirds of the catheter was inside the vessel, at which point the cannula was released into the vessel.
Correct placement was verified using the clinical judgement of the inserter and confirmed by flushing the catheter without resistance or the patient reporting pain. Blood return from the cannula and ultrasound visualisation of the catheter tip post insertion were also used to further validate correct placement. Patients were reviewed daily by a member of the vascular access team until device removal for any reason; during review the cannula insertion site was assessed using the Trust phlebitis scoring assessment tool, and the function of the device was assessed. In addition to documentation of the PIVC insertion in the Trust care plan, the vascular access team's existing surveillance database was adapted to collect information on:
- Inpatient or outpatient insertion
- Insertion date
- Device type
- Departmental location
- Insertion site location
- Device indication
- Removal date
- Reason for removal.
Complication rates and catheter days were generated from this information. The documenting of the number of attempts to insert the device successfully was added part way through the evaluation period, and started in 2021.
To ensure that complication rates remained within acceptable limits, device outcome data were reviewed weekly, using as a benchmark the cannula complication rates reported by Helm et al (2016), who specifically reported the incidence of reported PIVC complications. Any introduction of a new vascular access device should also be monitored for an increase in device-related infection (Loveday et al 2014). During this process, complications were discussed and inserter technique was adapted to improve success. During the initial period of the evaluation, cannula dislodgement was higher than expected. To reduce this a stabilisation dressing (BD Statlock™ IV Ultra Stabilization Device) was added to secure the catheter hub underneath the semi-permeable IV dressing, which reduced dislodgement. Six months after the evaluation began, the frequency of patient reviews was reduced from daily to weekly, once it was clear that complication rates remained within acceptable limits.
The IV support workers within the vascular access team were then trained by the IV specialist nurses to insert extended-length PIVCs. This process included:
- Completion of Trust standard cannulation training and competency assessment
- Basic ultrasound theory and practical application
- Simulation practice using a training phantom and direct supervision of practice until consistent success and confidence was achieved. The number of successful cannula insertions required under supervision was not a specific number – it was based on the consistent success and confidence of the inserter.
Cost impact analysis in this study used the following; equipment costs: £3.30 for standard catheters; £12.63 for extended-length catheters; and £85 for midline devices. This comparison was drawn to demonstrate the potential reduction in wastage and resources that can be made when the use of extended-length PIVCs is successful. Prior to this evaluation, patients with DIVA underwent multiple failed cannulation attempts, with subsequent referral to the vascular access team for a midline insertion if standard peripheral cannulation was not feasible. Total clinician time per procedure was estimated to be 20 minutes for a short or extended-length catheter insertion, and up to 1 hour for a midline.
Clinician hourly rate was taken from the unit Costs of Health & Social Care (Curtis and Burns, 2020). No additional funding was obtained to implement the extended-length PIVC, with the costs of the evaluation supported by existing resources within the service: the cost of devices was covered by the existing budget and the time of health professionals was covered by vascular access team's resources.
Data were collected between 2019 and 2022 and analysed on SPSSv27. All data were checked for normality and the appropriate median or mean reported. This study is not classed as research and did not require ethical approval, according to the Health Research Authority guidelines (2023).
Results
Between 2019 and 2022, 1485 individual extended-length peripheral catheter insertions were performed, 1385 for inpatients and 100 for outpatients. Table 1 shows the indications for all extended-length PIVC individual insertions.
Table 1. Indication for ultrasound-guided peripheral intravenous cannulation
| Percentage (%) | |
|---|---|
| Outpatient insertions | |
| Indication | |
| IV therapy | 57 |
| CT scan | 37 |
| Unknown | 5 |
| MRI scan | 1 |
| Inpatient insertions | |
| IV therapy | 97 |
| CT scan | 2.2 |
| Unknown | 0.3 |
| MRI scan | 0.01 |
In terms of device removal, the reason(s) were recorded for 1117 inpatient and 59 outpatient insertions. Treatment completion was recorded for 79% of inpatients and 87% of outpatients (Table 2). The remaining 21% and 13% of removals consisted of device failures and are detailed in Table 2.
Table 2. Distribution of treatment completion and treatment failure
| Percentage (%) | |
|---|---|
| Inpatients | |
| Treatment complete, excluding death | 75.2 |
| Patient death (unrelated to PIVC) | 3.9 |
| Total treatment complete | 79.1 |
| Complication | |
| Phlebitis | 5.8 |
| Infiltration | 2.9 |
| Dislodgment | 3.3 |
| Patient accidental removal | 3.1 |
| Pain | 1.8 |
| Other reasons | 3.4 |
| Reason not recorded | 0.4 |
| Total failures | 20.7 |
| Outpatients | |
| Total treatment complete | 87 |
| Complication | |
| Phlebitis | 1 |
| Infiltration | 9 |
| Dislodgment | 1 |
| Patient accidental removal | 1 |
| Not flushing | 1 |
| Total failures | 13 |
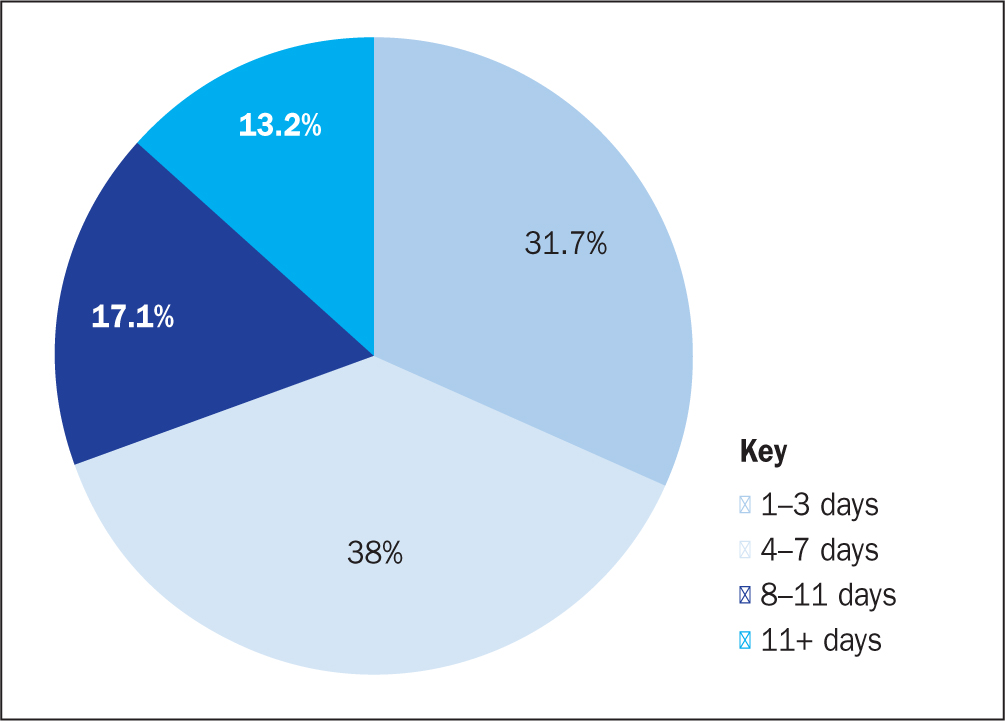
Out of 1485 recorded insertions, 1078 inpatient insertions had a dwell time recorded, summarised in (Figure 1). The median device dwell time, regardless of therapy success, was 6 days with almost 70% of devices remaining in situ for up to 7 days and 13.2% of devices still in use after 11 days.
There were substantially more insertions in the forearm compared with the upper arm, with 76% of all insertions made in the forearm over the course of the evaluation. In total, 90.7% insertions of extended-length cannulas were successful on first attempt and a further 8.7% were successful on the second attempt (Table 3).
Table 3. Overall insertion success rates, inclusive of inpatient and outpatient data (n=1078)
| Insertion attempt | Success rate (%) |
|---|---|
| 1 | 90.7 |
| 2 | 8.7 |
| 3 | 0.6 |
Finally, a cost impact analysis was made to describe the benefit of introducing extended-length PIVCs (Table 4). Analysis revealed that the cost of each extended-length PIVC insertion was £32.63, that per standard length PIVC was £19.97 and that for per midline insertion was £145. Alternatively, if a patient had to have three consecutive standard PIVCs inserted and then a subsequent midline, the total cost would mount to around £204.91. Using this calculation, it was estimated that one extended-length PIVC inserted would potentially save £172.28, avoid multiple needle punctures and any midline-associated complications. The cost of 1485 extended-length PIVC insertions was calculated at £48 456, providing a significant saving; this compares with 1485 patients potentially having to have undergone three failed standard PIVCs at a cost of £88 966, or 1485 midline insertions at a cost of £215 325. The cumulative cost of the three failed standard PIVCs and midlines would have totalled £304 291, demonstrating that the extended-length PIVC was a cost-effective alternative.
Table 4. Cost impact analysis of using a standard short peripheral intravenous cannula (PIVC) versus an extended-length for patients with difficult intravenous access
| Short PIVC | Midline | Extended-length PIVC | ||||
|---|---|---|---|---|---|---|
| Attempts | 1 | 2 | 3 | 4 | Attempts | 1 |
| Equipment costs | £3.30 | £3.30 | £3.30 | £85 | Equipment costIncluding single extension | £12.63 |
| Clinician costs | £16.67 | £16.67 | £16.67 | £60 | Clinician cost | £20.00 |
| Total costs | £19.97 | £19.97 | £19.97 | £145 | Total cost | £32.63 |
| Cumulative costs | £19.97 | £39.94 | £59.91 | £204.91 | ||
Discussion
This study has reported the results of implementing extended-length PIVCs for short-term vascular access in patients with DIVA. All 1485 extended-length PIVCs were inserted for patients with no visible or palpable veins and multiple failed PIVCs inserted. The majority of inpatient insertions (97%) were for IV therapy; for outpatients, insertions were more evenly divided between IV therapy (57%) and access required for a CT scan (37%).
Insertion success
This evaluation reported on a high number of inserted cannulas (1485) with consistently low complication rates of 21% and 13% for inpatient and outpatients respectively. This is favourable considering that up to 90% of PIVCs are reported as failing prematurely (Alexandrou et al, 2018), demonstrating that extended-length PIVCs are effective and reliable in patients with DIVA. The first-time success rate in this evaluation was 91% and 9% on the second attempt. These are positive results when compared with other ultrasound-guided PIVC studies in DIVA populations, which have reported first-time success rates of 69% (Au et al, 2012) using a standard length catheter, while extended-length devices studies have been reported as having success rates of 87% (Duran-Gehring et al, 2016), 73% (Bahl et al, 2019) and 97% (Bahl et al, 2020).
This evaluation has provided evidence of consistently successful ultrasound-guided cannulation in patients with DIVA, without any adverse effects associated with implementation of an extended-length catheter. This is a patient group in which cannulation can be extremely difficult (Miles et al, 2021).
Extended-catheter length
Long PIVCs are defined by Pittiruti et al (2023) as catheters that are 6–15 cm in length; Gorksi et al (2021) describe long PIVCs as being inserted in deep or superficial veins in instances when standard length catheters are not adequate to cannulate the vein. All devices included in this evaluation were extended-length PIVCs as they meet one of these criteria. Long PIVCs are advocated within the Infusion Therapy Standards of Practice (Gorski et al, 2021) to increase catheter vein ratio, enabling two-thirds of the catheter to reside within the vessel, even in vessels that lie deeper below the skin surface.
In a study of patients with DIVA, Bahl et al (2020) found that to increase PIVC survival, the optimum length of catheter in the vein was 2.75 cm or more. This was strongly associated with increased survival and a median survival time of 129 hours was reported. In addition, Fields et al (2012) discussed the importance of ensuring that adequate catheter length resides in the vein to reduce PIVC failure. The use of extended-length catheters in this evaluation meant that the length of catheter positioned within the vein was increased, suggesting that this contributed to increased survival, as evidenced by extended catheter dwell times.
Device survival
The inclusion of device outcomes, dwell times and complication rates reported in this article provide insight into how well the extended-length PIVC device performed. The evaluation collected data from insertion to removal through detailed surveillance. This included face-to-face reviews rather than documentation alone, providing assurance regarding the reliability of the data. This is vital in order to demonstrate that the patients' vascular access needs were met by the device, as premature failure continues to be a reported problem in 35-50% of cannulations (Helm et al, 2015). In the authors' hospital, treatment completion rates of 79% and 87% for inpatients and outpatients respectively indicated that the extended-length PIVC is a safe and effective device.
Treatment completion rates of extended length versus standard length peripheral catheters in patients with DIVA have previously been explored. For example, two US studies (Bahl et al, 2019; 2020) published success rates of 48% and 69% and 27% and 58% in their standard and extended-length PIVC groups respectively. In addition, an Italian study (Fabiani et al, 2017) reported a success rate of 59% with extended-length catheters in patients with DIVA after cardiac surgery. The therapy completion rates of 79% and 87% in the authors' evaluation are higher than this, clearly demonstrating that extended-length PIVCs are effective for short-term peripheral IV therapy in DIVA patients. This is important when considering the variability reported on PIVC success in other studies, and the real-world setting of this evaluation.
Catheter dwell times provide an indication of the length of time that a device maintains its function safely (Helm et al, 2015). The median dwell time achieved in this evaluation was 6 days. A comparison of the findings of this study with the results of similar PIVC studies in the DIVA population shows a substantial improvement from the 26 hours, as reported by Dargin et al (2010), and the 4.04 days, as reported by Bahl et al (2019). The 6 days reported here are consistent with 5.7 days reported Bahl et al's (2020) later study and 6.4 days reported by Pare et al (2019), achieved using extended-length PIVCs. This is also significantly longer than the 1.25 and 3.8 days median dwell time found in studies by Bahl et al (2019) and Bahl et al (2020) using a standard-length PIVC and 2.39 days, which was reported by Miles et al (2021) using PIVC of varying lengths.
The extended dwell times, high treatment completion rates and low complication rates presented in this article are evidence that this device is safe and reliable for patients with DIVA.
Device location
PIVCs placed in the forearm are reported as superior, with occurrence of less dislodgement and occlusion (Alexandrou et al, 2018), and improved survival (Fields et al, 2012). The extended-length PIVC also avoids the deep vessels, preserving them for future health needs (Moore, 2013). Alexandrou et al (2018) reported that only one-third of all PIVCs are inserted in the forearm, but in this evaluation this was the site used for 76% of insertions, which is significantly higher, with the remaining PIVCs (24%) inserted in the upper arm. This demonstrates successful extended-length PIVC insertion in the optimum IV insertion sites away from areas of flexion, even in patients with DIVA.
Taking into account vessel health preservation (Hallam et al, 2021) and recognised standards of practice (Gorski et al, 2021), the findings reported in this article are noteworthy, because in some studies exploring the insertion of PIVCs guided with ultrasound the devices were placed only in the upper arm or antecubital fossa (Bahl et al, 2020; Miles et al, 2021). This evaluation provides evidence that extended-length PIVCs can be successfully inserted at optimum peripheral cannulation sites, in superficial upper extremity vessels, avoiding the basilic and brachial upper arm veins.
Patient impact
Prior to introducing ultrasound-guided extended-length PIVCs at Aintree Hospital, Liverpool Hospitals NHS Foundation Trust, patient treatments or procedures were delayed or cancelled when PIVCs repeatedly failed. Ordinarily, patients with failed devices were escalated to the vascular access team and a peripheral midline insertion was the only suitable alternative that could be provided. Extended-length PIVCs are an alternative that reduces the need to use midlines, improving the patient experience and benefiting the healthcare organisation.
As a result, pathways have been developed with radiology and outpatient day-case services, allowing patients with DIVA to attend the vascular access team for extended-length PIVC insertion immediately prior to their procedure or treatment, ensuring reliable, timely vascular access. PIVCs are more cost-effective and less invasive than the alternatives used prior to this and avoid any additional procedural risks. The use of these devices also reduces resources and time wasted on failed attempts and the subsequent impact on the patient journey. In addition, this intervention has evolved into the provision of ultrasound-guided phlebotomy, reducing the number of failed phlebotomy attempts for patients with DIVA. These services have emerged gradually, precipitated by patient need, reflecting the prevalence of this patient cohort, with more than one-third of adults reported to have difficult IV access (Whalen et al, 2017). The pain and anxiety associated with undergoing multiple, painful needle punctures, are also reduced as patients are reassured that they can access a service that meets their vascular access needs, which are more complex for these patients than for those who do not have DIVA.
Strengths
This evaluation included the placement of a large number of extended-length PIVCs and used comprehensive surveillance. It demonstrated high success rates and low complication rates. The study has demonstrated that safe, effective peripheral access can be achieved in the DIVA population with extended-length PIVCs, which are effective in the real-world clinical setting, not only during insertion, but post insertion also.
Limitations
This study collected real-time data from many health professionals. As such, there is a risk of erroneous data entry and/or data recall. It did not collect data on:
- The number of patients who were assessed but did not have a PIVC inserted
- The number of failed attempts prior to the patient being referred to the vascular access team
- The first-attempt success rate during the initial phase of the evaluation
- The number of rescue procedures that were avoided.
In addition, no comparative data were collected on patients with DIVA who had standard-length peripheral catheters inserted, nor were any clinical data available on patient parameters that may have affected device dwell time, such as patient weight or age.
Conclusion
To the authors' knowledge this is the first study within an NHS setting to explore the effectiveness of extended-length PIVCs placed in patients with DIVA. Taking into account all the data presented, the authors consider that the introduction of extended-length catheters in their hospital has improved the quality of life for patients with DIVA, reduced the number of failed cannulation attempts and delays in IV therapy, as well as reducing the number of cancelled procedures and investigations.
It is also important to highlight that the introduction of extended-length PIVCs has reduced the necessity to use more costly invasive lines for cannulation, has improved the delivery of therapy and procedures, and improved first-attempt insertion rates for patients with DIVA.
KEY POINTS
- Extended length peripheral intravenous catheters (PIVCs) provide reliable access in patients with difficult intravenous access (DIVA)
- Ultrasound-guided PIVCs can be successfully implemented in a vascular access team
- Extended dwell times and low complication rates can be achieved in patients with DIVA
CPD reflective questions
- Do any patients in your current practice have difficult intravenous access?
- Does the failure of peripheral intravenous catheters impact your practice?
- Can you implement extended-length PIVCs into your practice or that of others, and what actions do you need to take to make this happen?


