
In response to a report from the Law Commission (2017), Parliament enacted the Mental Capacity (Amendment) Act 2019, which will introduce a revised, less bureaucratic scheme to safeguard adults and young persons who are deprived of their liberty in care settings. This will replace the current deprivation of liberty safeguards under schedule A1 of the Mental Capacity Act 2005.
The 2019 Act introduces schedule AA1 to the Mental Capacity Act 2005, which makes provision for a revised scheme to authorise the deprivation of liberty of vulnerable people in any care setting. The purpose of the revised schedule is to enable the care or treatment of a cared-for person that gives rise to a deprivation of liberty and that does not conflict with any mental health arrangements the person may be subject to. The arrangements can include requiring the cared-for person to reside in a particular place or to receive care and treatment in that place. It also can include the means and manner of transport for the cared-for person to, from or between places (schedule AA1 2(3)).
In June 2019, the Care Minister gave 1 October 2020 as the implementation date for the provisions, but before then a revised code of practice and regulations that will provide the detail to operationalise the liberty protection safeguards need to be consulted on and approved by both Parliament in England and the Senedd in Wales (Haynes, 2019).
To properly prepare for the implementation of the liberty protection safeguards, it is essential that nurses become familiar with the new provisions so that they can inform the consultations on the revised code of practice and regulations and judge the impact of the revised safeguards on their practice. Nurses will also have to become familiar with the new terms set out in the revised schedule (Box 1).
Cared-for person
The revised provisions will provide for an administrative system that will be able to authorise the deprivation of liberty of a cared-for person in any care setting, not just hospitals and care homes covered under the current deprivation of liberty safeguards process.
A cared-for person for the purpose of the schedule AA1 will be someone who:
Responsible body
A responsible body will have a duty to authorise arrangements that amount to a deprivation of liberty if the conditions set out in schedule AA1 are met.
In England a responsible body can be:
In Wales a responsible body can be:
Duty to authorise arrangements
The responsible body with the duty to authorise arrangements that amount to a deprivation of liberty depends on the status and care setting of the cared-for person.
Under the provisions of the Mental Capacity Act 2005, schedule AA1 (6), the hospital manager is the responsible body where the cared-for person's arrangements are mainly in an NHS hospital. For independent hospitals, the responsible body in England is the local authority and in Wales it is the local health board. Clinical commissioning groups are the responsible body for cared-for persons subject to continuing healthcare arrangements in England whereas local health boards fulfil that role in Wales.
For all other care settings the local authority is the responsible body.
Right to information
Hospital managers, clinical commissioning groups, health boards and local authorities all have a duty to publish information in a form that is accessible to a cared-for person and that includes details on:
That duty extends to ensuring that, as soon as practicable, they take practical steps to ensure that the cared-for person and any appointed appropriate person understands the arrangements and other information they have a duty to provide.
Process of authorisation
The process of authorisation is set out in Figure 1. Before a responsible body can authorise arrangements that amount to a deprivation of liberty, it must be satisfied that there is sufficient evidence that:
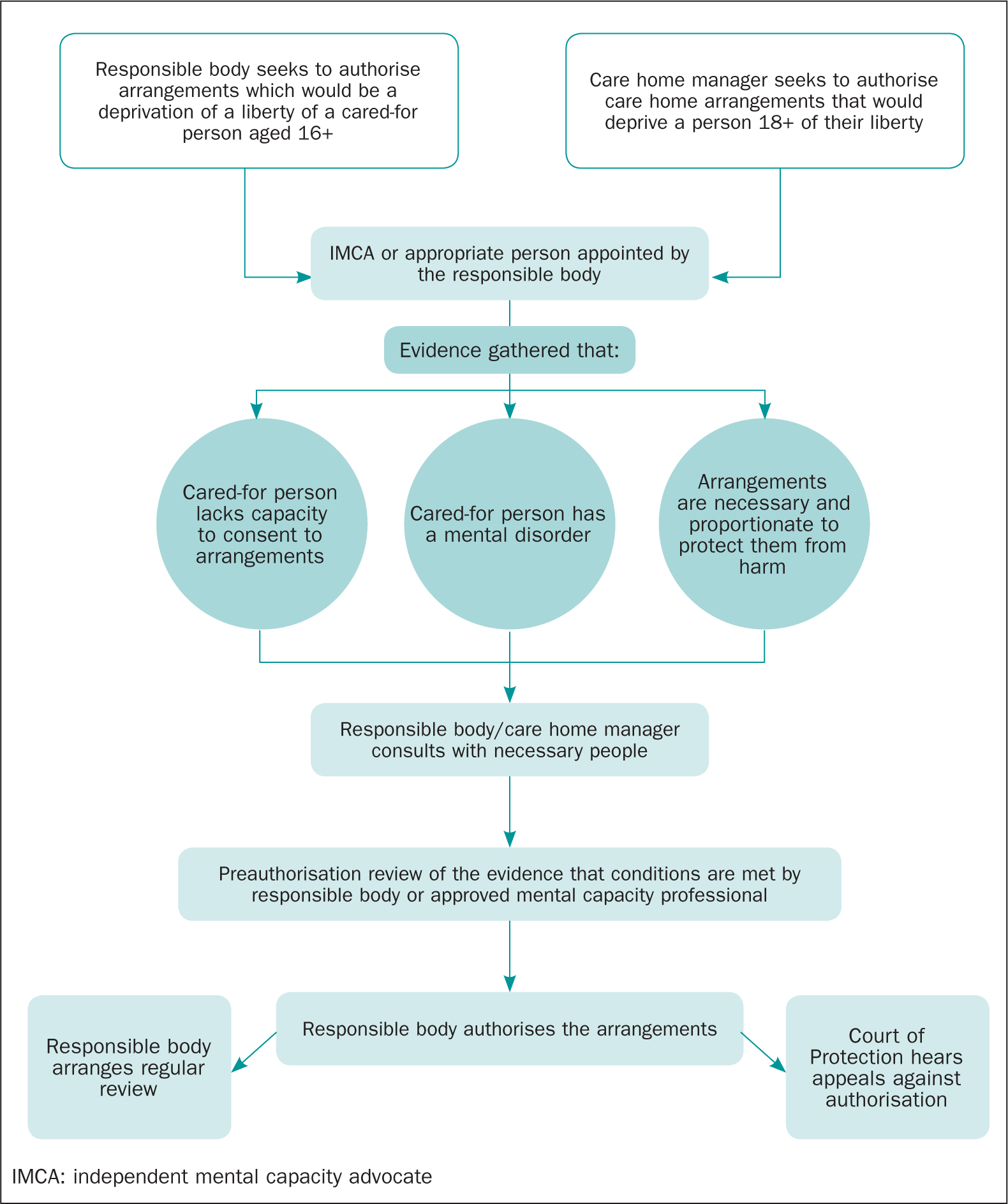
In the case of adults in care homes, the responsible body may ask the care home manager to provide a statement that they are satisfied they have evidence that the conditions for authorisation are met and to submit a draft authorisation record to the responsible body for them to sign.
Preauthorisation review
Evidence that a cared for person meets the conditions for their arrangements to be authorised will be subject to a preauthorisation review by a person from the responsible body who is not someone involved in the day-to-day care or providing treatment to the cared-for person and if satisfied they will prepare a draft authorisation record for a responsible body authoriser to sign.
Approved mental capacity professionals
Where the cared-for person:
Then the preauthorisation review must be undertaken by an approved mental capacity professional (AMCP). The Mental Capacity Act 2005, schedule AA1 requires every local authority in England and Wales to make arrangements for the approval of AMCPs and ensure they have sufficient numbers of AMCPs for their area.
In undertaking a preauthorisation review AMCPs must:
Authorisation of a deprivation of liberty
A responsible body can authorise a deprivation of liberty once the preauthorisation reviewer or AMCP confirms they are satisfied that the conditions are met and submit a draft authorisation record to be signed off by the responsible body authoriser.
The document then becomes the authorisation record and will detail:
The responsible body has a duty to provide a copy of the authorisation record to the cared-for person and their IMCA or appropriate person. That duty must be discharged with 72 hours of authorisation or the responsible body must review and record why this has not happened. Responsible bodies must also take practical steps to ensure that the cared-for person and any appointed appropriate person understands the arrangements that have been authorised.
The duration of authorisation will depend on the individual circumstances of the each cared-for person. The Mental Capacity Act 2005 schedule AA1 allows maximum authorisation periods of
Reviews of authorisation
The responsible body must set out a programme of regular reviews for every authorisation to ensure that the arrangements continue to be necessary and proportionate and that the conditions for authorisation continue to be met.
Responsible bodies must also hold a review under any of these circumstances:
Excluded arrangements
The safeguards set out in the Mental Health Act 2005, schedule AA1 do not apply to the following mental health arrangements where the cared-for person is:
Arrangements under the schedule would also be excluded if they did not accord with:
Lawful deprivation of liberty in an emergency or while awaiting authorisation
The provisions of the Mental Capacity Act 2005, section 4B will allow a cared-for person to be lawfully deprived of their liberty without authorisation where this is necessary for the provision of life-sustaining treatment or to perform a vital act.
Section 4B of the 2005 Act applies in an emergency or when waiting for a court or responsible body to authorise arrangements that amount to a deprivation of liberty. The 2005 Act does not impose a time limit on section 4B.
For the purpose of section 4B a vital act is one that prevents serious deterioration in a person's condition. An emergency means there is an urgent need to give life-sustaining treatment or perform a vital act and it is not reasonably practical to wait for authorisation or detain the person under the MHA 1983.
Revised code of practice and regulations
Before the liberty protection safeguards can be implemented a revised Mental Capacity Act 2005 code of practice needs to be approved and regulations need to be passed by Parliament and the Senedd that set out the requirements for the operation of the safeguards.
As Parliament could not agree a statutory definition of a deprivation of liberty, the Mental Capacity (Amendment) Act 2019 instead requires that guidance on what kinds of arrangements amount to a deprivation of liberty must be set out in the revised code of practice.
In addition, Parliament in England and the Senedd in Wales will decide through regulations:
Conclusion
Although the Mental Capacity (Amendment) Act 2019 sets out the framework for replacing the current deprivation of liberty safeguards with more streamlined and less bureaucratic safeguards, it can be seen that much of the regulation needed to implement the new safeguards is still outstanding. To achieve the planned implementation date of 1 October 2020 the regulations will have to be available for consultation and final approval in the spring of 2020 together with a revised code of practice. To ensure a meaningful consultation on the proposed regulations and code of practice it is essential nurses are familiar with the revised safeguards framework so that they can gauge their impact on practice and provide well-informed feedback before the new safeguards are adopted.

