Lung cancer is the third most common cancer in the UK, with 47 235 newly diagnosed cases recorded between 2014 and 2016 (Cancer Research UK, 2019). Surgery remains the first choice of curative treatment for individuals with stage 1 and stage 2 non-small cell lung cancer who are medically fit and who wish to have surgery (Lim et al, 2010). Between 2014 and 2015 the number of patients undergoing surgery in NHS hospitals in the UK rose from 5657 to 6000, an increase of 5% (Royal College of Physicians, 2017). Although postoperative complications are well recognised (Agostini et al, 2010; Stéphan et al, 2000), there is limited data that focuses on readmission rates following thoracic surgery.
Readmission to hospital after surgery impacts on patients' physical and psychological wellbeing while increasing health costs (Tsai et al, 2013). Studies that have explored readmission following pulmonary resection have primarily compared surgical technique (Freeman et al, 2013; Boffa et al, 2014), enhanced recovery programmes (Salati et al, 2012), the impact of postoperative pulmonary complications (Lugg et al, 2016) and length of hospital stay (Freeman et al, 2013).
Members of the UK Thoracic Surgery Group (TSG), a subgroup of the National Lung Cancer Forum for Nurses, proposed undertaking a multicentre review to understand the factors surrounding readmission rates in patients undergoing curative lung cancer resection.
Aims
The aims of the multicentre review were to identify:
Method
The review involved six UK thoracic surgical centres. Prospective data were collected between 1 May and 31 July 2017 from patients undergoing primary lung cancer surgical resection (excluding carcinoids). Data collection parameters were decided by TSG members, and a standard data collection sheet/questionnaire was designed for use across each centre. Individual patient qualitative information was collected and reported verbatim for each individual.
Each patient received information regarding the review and consented appropriately. Data were collected from patients' clinical notes and through telephone calls made by the authors one month post-discharge, and included information regarding demographics, social situation, intra- and postoperative outcomes and readmission details. Qualitative information (patients' opinion of their readiness for discharge, support in the community, and overall experience) was also collected at this time by the authors and documented on the data collection sheet. Completed forms were uploaded to an online data collection system and analysed centrally by one of the centres.
Statistical analysis
We used Student's t test for normally distributed variables to compare means, the Mann-Whitney test to compare non-normally distributed variables, and the chi square test to compare categorical data. A P value of less than 0.05 was considered statistically significant. All analyses were performed using GraphPad Prism v7.0 (GraphPad Software, San Diego, CA).
Results
Across the six thoracic surgical centres, 268 patients with primary lung cancer had had thoracic surgery between 1 May and 31 July 2017. Baseline demographics are presented in Table 1.
| Patient characterics | Overall total | Non-readmission group | Readmission group | P value | ||||
| n=268 | % | n=238 | % | n=30 | % | |||
| Gender | Female | 143 | 53 | 124 | 52 | 19 | 63 | |
| Male | 125 | 47 | 114 | 48 | 11 | 37 | 0.33 | |
| Age (years) | 20-39 | 2 | 2 | 1 | - | - | ||
| 40-59 | 33 | 12 | 27 | 11 | 6 | 20 | ||
| 60-79 | 206 | 77 | 183 | 77 | 23 | 77 | ||
| 80+ | 27 | 10 | 26 | 11 | 1 | 3 | 0.33 | |
| Social situation | Lives with family and friends | 192 | 72 | 169 | 71 | 23 | 77 | |
| Lives alone good support | 59 | 22 | 54 | 23 | 5 | 17 | ||
| Lives alone no support | 9 | 3 | 7 | 3 | 2 | 7 | 0.45 | |
| No data | 8 | - | 8 | 3 | ||||
| Smoking history | Never been a smoker | 37 | 14 | 33 | 14 | 4 | 13 | |
| Ex-smoker | 153 | 57 | 140 | 59 | 13 | 43 | ||
| Current smoker | 78 | 29 | 65 | 27 | 13 | 43 | 0.18 | |
| ECOG*/WHO† scale to evaluate cancer patients' functional status | 0 | 124 | 46 | 109 | 46 | 15 | 50 | |
| 1 | 116 | 43 | 103 | 43 | 13 | 43 | ||
| 2 | 20 | 8 | 18 | 8 | 2 | 7 | 0.95 | |
| 3 | 1 | - | 1 | 0.4 | - | - | ||
| No data | 7 | - | 7 | 3 | - | - | ||
| Comorbidities | None | 47 | 18 | 41 | 17 | 6 | 20 | |
| 1 | 87 | 32 | 76 | 32 | 11 | 37 | ||
| 2 | 65 | 24 | 59 | 25 | 6 | 20 | ||
| 3 | 42 | 16 | 38 | 16 | 4 | 13 | ||
| 4+ | 27 | 10 | 24 | 10 | 3 | 10 | 0.95 | |
Just over half of the operations (150; 55%) were performed using a minimally invasive approach, although this varied across the six centres (range 34–79%). Lobectomy was the most common procedure performed (209; 78%) and adenocarcinoma was the most common cell type (168; 68%). Most patients 198/221 (90%) had attended a preadmission clinic, although one centre does not have this service.
Under half the patients (111; 41%) had had no postoperative complications. In most of the centres, the most common postoperative complications were persistent air leak (PAL) (centres A, B, D, E, F) and persistent postoperative pain (centres A, C, D, E, F). Of the 268 patients, 48 (18%) went home with a pleural drainage system for a PAL; their average length of stay was 7 days.
The overall median length of hospital stay was 6 days (range 1–28) although this varied across the six centres (range 4–8). Current smokers' average length of stay was 8 days. Patients who had minimally invasive surgery had, on average, a shorter length of stay than those who had had a thoracotomy incision, 6 days versus 8 days respectively. The number of postoperative complications increased mean length of stay: 6 days for patients with no complications versus 13 days for patients experiencing 4+ postoperative complications. Operative mortality was 0% and 30-day mortality 1%.
Overall, 30 (11%) patients were readmitted within 30 days of discharge, although this varied across the six centres (3–24%) (Figure 1).
The data show that 14/30 (47%) readmissions occurred within 7 days of discharge, with 13/30 (43%) patients being readmitted to a hospital that had not performed the surgery. The length of stay following readmission was longer than patients' initial surgical stay: median 8 days (range 0–94) versus 5 days (range 2–27). The causes of readmission were primarily pulmonary related (19/30; 63%) (Figure 2).

Information on whether patients considered themselves to be ready for discharge showed that 87% (234/268) felt ready for discharge versus 12% (32/268) who did not (Figure 3). Of these 32 patients, 9 were readmitted. Therefore, within the readmissions group, one third of patients stated that they did not consider themselves to have been ready for discharge.
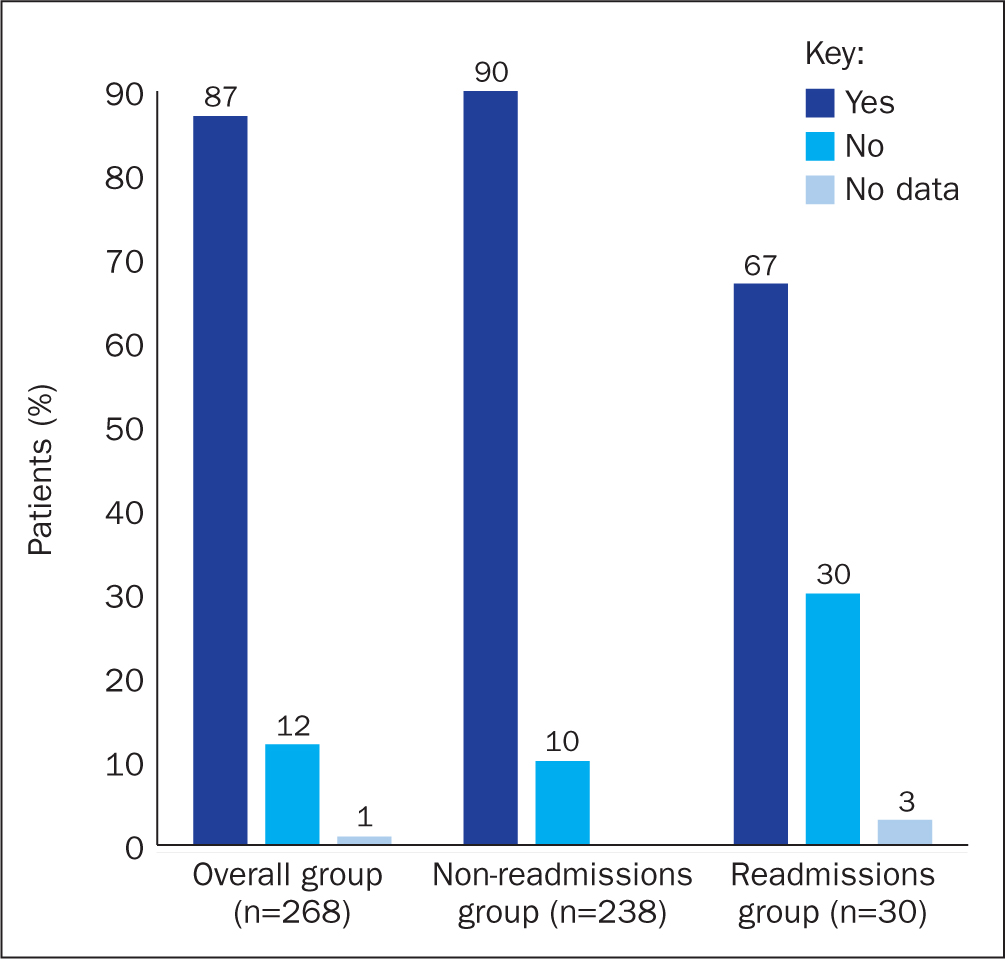
Figure 4 shows that 88% (236/268) of patients stated that they had not felt supported in the community. Of the 9 individuals in the readmissions group who had not felt ready for discharge, 5 also felt that they were unsupported in the community.

Readmission was associated with being discharged with a pleural drain (11/30; 37%) (P<0.01), having two or more postoperative complications (11/30; 37%) (P<0.01), patients' length of stay post-surgery and their readiness for discharge (9/30; 30%) (P=0.001). There was a trend toward an association with smoking (13/30; 43%) (P=0.18).
Discussion
Readmission rates
There is limited literature on readmission after thoracic surgery. Boffa et al's (2014) analysis of data from the Society of Thoracic Surgeons database for 2001–2010 identified a readmission rate of 6% after lobectomy for clinical stage 1 lung cancer. Assi et al (2015) found readmission rates of 10% following pulmonary resection, irrespective of the surgical approach used (minimally invasive surgery or open thoracotomy). Readmissions following the introduction of enhanced recovery have been reported at 5.5% (Salati et al, 2012). Stiles et al's (2016) analysis of American databases (states of California, Florida and New York) identified 22 645 lobectomies performed in 2009-2011: they found the 30-day readmission rate to be 11.5%, and this was strongly associated with an individual's comorbidities. These researchers also found that 26.6% of patients who were readmitted within 30 days were admitted to hospitals that had not performed the primary surgery.
Within this prospective multicentre review, analysis of the 268 lung cancer resections identified an overall readmission rate of 11% within 30 days of discharge. This varied between the six centres between 3% and 24%. Readmission in this review was correlated with two or more postoperative complications; pleural drainage system; length of stay post-surgery; and the patient's readiness for discharge. Like Assi et al's (2015) study, the authors' review did not find that the surgical approach was a factor associated with readmission and, in keeping with Stiles et al (2016), the findings presented in this article also reflect that a percentage of patients (43%) were readmitted to hospitals that had not performed the original operation, suggesting that the true readmission rate may be underestimated.
Reasons for readmission
All the readmissions appear to be clinically necessary and primarily pulmonary related. Freeman et al (2013) found that patients discharged after an initial length of stay of less than 5 days were readmitted due to sterile pleural effusion, pneumothorax and atelectasis. Our findings were similar to Freeman's, in that 16/30 (53%) patients were readmitted following an initial stay of 5 days or shorter and were predominately readmitted for the same reasons as identified by Freeman.
The management and threshold for chest-tube removal varied between consultants, individual preferences and hospital protocols. This highlights an area for a future audit to identify possible areas in which practice may be improved or changed to reduce readmission rates.
For patients readmitted after an initial length of stay longer than 7 days, several causes for readmission were identified, the most common being deterioration in overall condition; shortness of breath; chest infection; pneumonia; bronchopleural fistula; wound infection; and deep vein thrombosis/pulmonary embolism.
Smoking
In keeping with published research (Agostini et al, 2010; Seok et al, 2014), the findings of this review show that patients who were current smokers at the time of their thoracic surgery had a prolonged length of stay and were more likely to be readmitted. Factors contributing to this may include sputum retention, delayed improvement in inflammatory responses, and possible reduction in irritant-induced coughing (Moller et al, 2002).
Although an optimal interval of smoking cessation has not been identified, studies suggest that cessation should occur at least 4 weeks prior to surgery and that 8 weeks is preferable (Nakagawa et al, 2001; Moller et al, 2002). Due to the impact of smoking on length of stay and readmission, a more structured counselling service is required to increase the chances of smoking cessation prior to thoracic surgery.
Postoperative complications
Within our review, postoperative complications increased the likelihood of an unplanned readmission, a finding that was consistent with evidence from other studies (Rajaram et al, 2015). The most common postoperative complications in our review were PAL, chest infections, pain and arrythmias. It may be that patients who experience a complicated recovery require extra monitoring following discharge and that a strategy of planned early return to an outpatient clinic is needed to prevent emergency department visits and readmission.
Pleural drainage system
Persistent air leak (PAL) is defined as a leak that persists for more than 6 days after lung resection (Elsayed et al, 2012). However, with the introduction of more minimally invasive surgery, the definition of PAL is likely be revised. The findings of this review are that PAL was the most common postoperative complication. Forty-eight (18%) patients went home with a pleural drainage system, and 11/48 (23%) of whom were readmitted; therefore, in the readmission group, patients with a pleural drainage system accounted for 37% (11/30).
Patients discharged with a pleural drainage system need there to be effective communication and coordination with local community services. This raises questions regarding the importance of effective discharge planning, the importance of education and the establishment of an effective network in the community to address and monitor patients discharged with a pleural drain.
Length of stay
In this review, the initial length of stay appeared to be influenced by a patient's current smoking status, the surgical approach and the number of postoperative complications, correlating with published research findings (Rajaram et al, 2015; Stiles et al, 2016).
Enhanced recovery programmes aim to reduce hospital length of stay and cuts costs by:
All these factors play a role in successful early discharge. However, the findings of the authors' review appear to suggest a correlation between a shorter length of stay and readmission. We found that 16/30 (53%) patients who were readmitted had a length of stay shorter than 5 days, suggesting that patients with a shorter length of stay may have a higher risk of readmission. The median length of stay is shorter in the readmissions group (5 days) by 1 day compared with the non-readmissions group (6 days).
Across all centres, for patients who had been readmitted there appeared to be a correlation between a short initial length of stay (median 5 days), and protracted readmission length of stay (median 8 days). This may be more significant when considered alongside patients' comments on their feelings on their readiness for discharge.
Qualitative analysis
Patients' comments regarding why they did had not felt ready for discharge were analysed through the grounded theory method using an inductive approach. The comments were carefully read, and relevant findings highlighted and moved into subcategories and then categories. Relationships between the categories were then identified and integrated together with the following four themes emerging (Figure 5):

Patient's discharge
One third of patients in the readmissions group commented that they had not felt ready for discharge. Actively listening to patients' assessment of their readiness for discharge is crucial, because this may identify issues that need to be addressed in order to facilitate patient compliance with discharge and their confidence in community carers. However, the authors acknowledge that the fact that patients had been asked retrospectively whether they had been ready for discharge may have influenced their answers due to how their recovery had progressed.
Hospital discharge is a complex and challenging process for health professionals, patients and carers, which is further complicated by pressures on length of stay. Research shows that having a structured discharge plan in place tailored to individual patient needs reduces readmission (National Institute for Health and Care Excellence, 2015). Effective discharge, therefore, must be supported by good communication between the hospital and community-based professionals involved in the patient's care.
Conclusion
This review has provided a broad overview of the pattern of readmissions to hospital within 30 days of discharge following lung cancer resection. All six thoracic centres included in this review share the aim of providing excellent patient care and reducing readmission rates.
The review found that readmission was associated with individuals being current smokers, having two or more postoperative complications, being discharged with a pleural drainage system, on their length of stay post-surgery and on their readiness for discharge.
Although not every readmission can be avoided, there is the opportunity to reduce readmission-related risk factors by:
The ethos of the enhanced recovery is that patients are active participants in their care and recovery, therefore one of our main considerations when discharging patients should be to incorporate their feedback related to their overall experience and readiness for discharge.

