The demand for developing new protocols for inpatient care to make better use of hospital services has increased rapidly (Charles et al, 2019). For selected patients in hospitals, outpatient parenteral antimicrobial therapy (OPAT) has emerged as a feasible option that not only contributes to cost-effective inpatient management but is also a popular patient preference (Tu et al, 2023). With substantial hospital bed and resource-related pressures, OPAT can contribute to providing care for patients and avoid hospital admission (Soni et al, 2024).
OPAT was first developed in 1970 for patients with cystic fibrosis in the USA and was subsequently adopted by other countries, including the UK (Durojaiye et al, 2018). As part of developing OPAT services across the UK, the British Society for Antimicrobial Chemotherapy (BSAC) launched the OPAT National Outcomes Registry System (NORS), which allows data from local patient management systems to contribute to a national registry (Hatcher et al, 2019). The use of OPAT has significantly transformed the management of infections, reducing the need for prolonged hospitalisations and establishing an antimicrobial agent administered once daily or weekly; this has also contributed to reducing financial pressures on the NHS (Chapman et al, 2019). The service offers an innovative solution that benefits both patients and providers (Durojaiye et al, 2018).
King's College Hospital NHS Foundation Trust in London is one of the UK's largest and busiest teaching trusts, with a £1 billion turnover, more than 1.5 million patient contacts annually, and a workforce of more than 15 000 staff distributed across southeast London. It offers a comprehensive range of both general and specialist services at its five sites, including haematology, maxillofacial surgery, complex cardiac surgery, obstetric emergencies, neurosurgery, hepatology, hepatobiliary and liver transplantation services. It attracts patients from the entire southeast area of England, especially as a major trauma centre serving the region.
King's OPAT service was launched in September 2022 as a pilot programme lasting 6 months, supported by the Southeast London Integrated Care System. Over 2 years, the service has successfully accommodated 391 patients, offering both intravenous and complex oral antimicrobial treatments, resulting in the saving of 9516 hospital bed days. These bed days include early inpatient discharge and admission avoidance. King's OPAT service is collaborating with Baxter and Bionical Health Ltd, a home-care provider, to extend the reach of the service from southeast London to Kent, Surrey and Sussex.
In this article, the authors present the outcomes of a retrospective service review spanning from 1 September 2022 to 31 September 2024. The review was conducted to assess the advantages of the OPAT service, with a particular focus on reducing inpatient bed days, and improving clinical efficacy and patient satisfaction.
Methods
A set of inclusion and exclusion criteria was devised to ascertain the suitability of patients for inclusion in the OPAT programme. The criteria (Table 1) were formulated with careful consideration of aligning with the Trust's Equality and Diversity Risk Assessment standards.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
|
Eligibility for OPAT extended to individuals aged 16 years and above requiring antimicrobial treatment exceeding 1 week in duration. It is imperative to note that this service was not confined exclusively to King's College Hospital's inpatients and outpatients; rather, it was made available to patients within the service catchment area, including those affiliated with other NHS trusts to facilitate admission avoidance. All eligible patients who were referred to the OPAT service between September 2022 and September 2024 were reviewed. Data were anonymised to ensure patient confidentiality.
OPAT suitability and patient pathways
A referral system was instituted to streamline the assessment process for potential OPAT patients. The OPAT team collaborated closely with the Trust's consultant microbiologist and infectious diseases consultants to promptly identify patients who might be suitable candidates. All eligible patients undergo a comprehensive evaluation conducted by a multidisciplinary team comprising infectious disease/microbiology consultants, specialist nurses, and an antimicrobial pharmacist. This holistic assessment is conducted to identify any obstacles to discharge, encompassing various factors such as:
OPAT administration methods
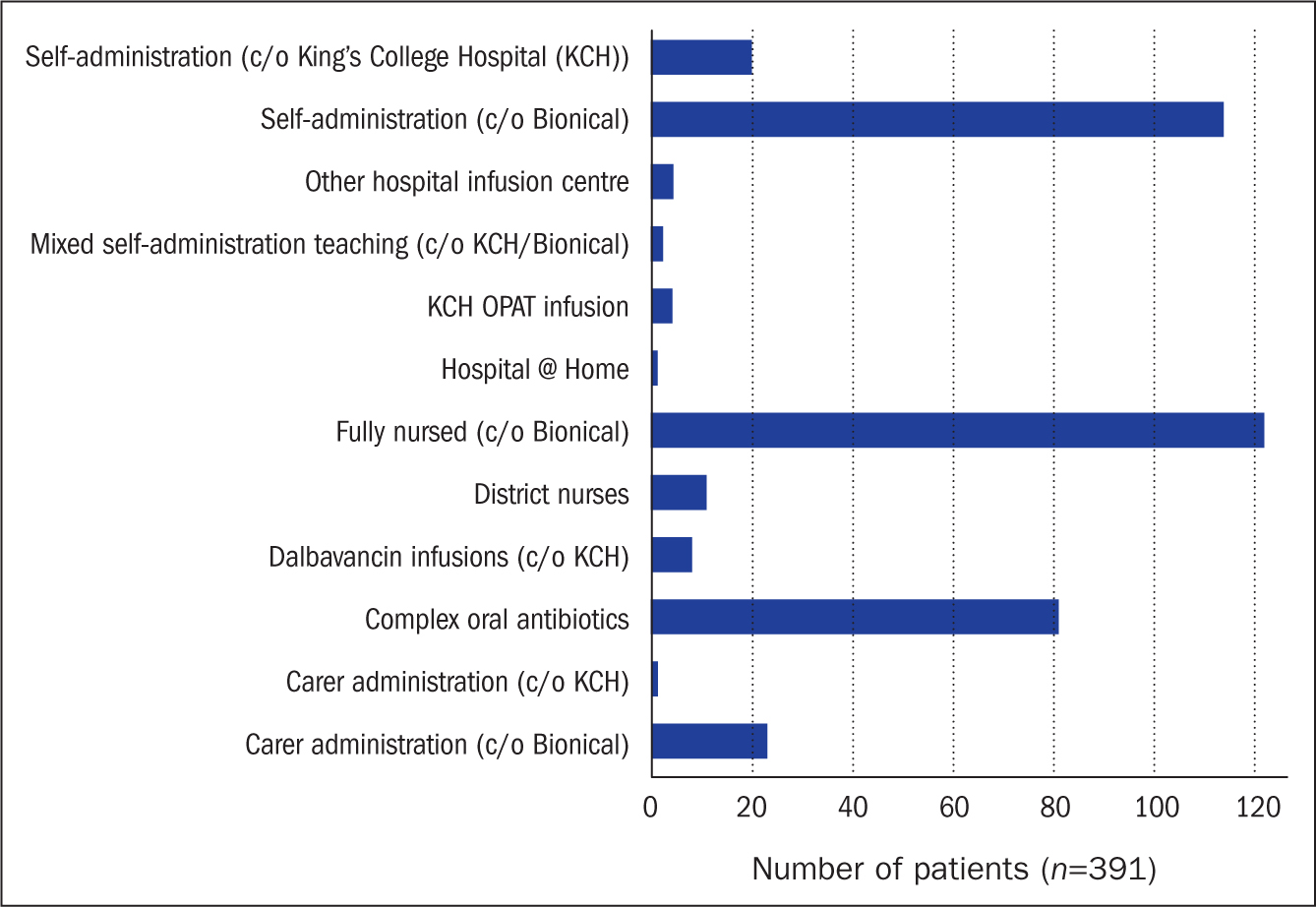
Patients admitted for OPAT undergo assessments to determine the most suitable method for administering therapy. As part of the review, each patient's eligibility for self-administration or requirement for caregiver assistance was evaluated based on family support, manual dexterity, cognitive function and visual acuity criteria. These were the primary factors influencing enrolment in self/carer-administration. Patients not meeting these criteria were designated to have their therapy administered by a nurse.
The assessment encompasses the patient's or the caregiver's proficiency in both traditional antibiotic mixing methods, involving syringes and needles, or the use of premixed elastomeric devices sourced from an external pharmaceutical provider.
Figure 1 shows the administration methods used with patients requiring intravenous administration of their antibiotics, as well as those who were solely on complex oral regimens. For patients referred for a period exceeding 48 hours, training in conventional administration methods was provided. However, those who were expected to be discharged within 48 hours were automatically directed towards using premixed elastomeric devices. Training for self/carer administration using these devices was conducted at the patient's home by the Bionical Health nursing team.
Intravenous infusions given three times a week (eg liposomal amphotericin B infusion) or once every 2 weeks (eg dalbavancin infusion) are given during the patient OPAT follow-up clinic.
OPAT cases and referrals
The King's OPAT service relies on a multidisciplinary approach, involving collaboration between infectious disease specialists/microbiologists, pharmacists, specialist nurses, and home health providers. This co-ordinated team approach ensures that patients are thoroughly monitored and supported, resulting in improved clinical results and lowering the risk of complications or the need for hospital readmission.
Between September 2022 and September 2024, King's OPAT service has managed a diverse range of cases, with the majority involving diabetic foot osteomyelitis, infected cranioplasty, epidural abscesses, endocarditis, discitis, and cerebral abscesses. Patients were referred from 26 different specialties, with the highest number of referrals originating from general medicine, neurosurgery, and diabetic foot services.
OPAT bed days saved and financial savings
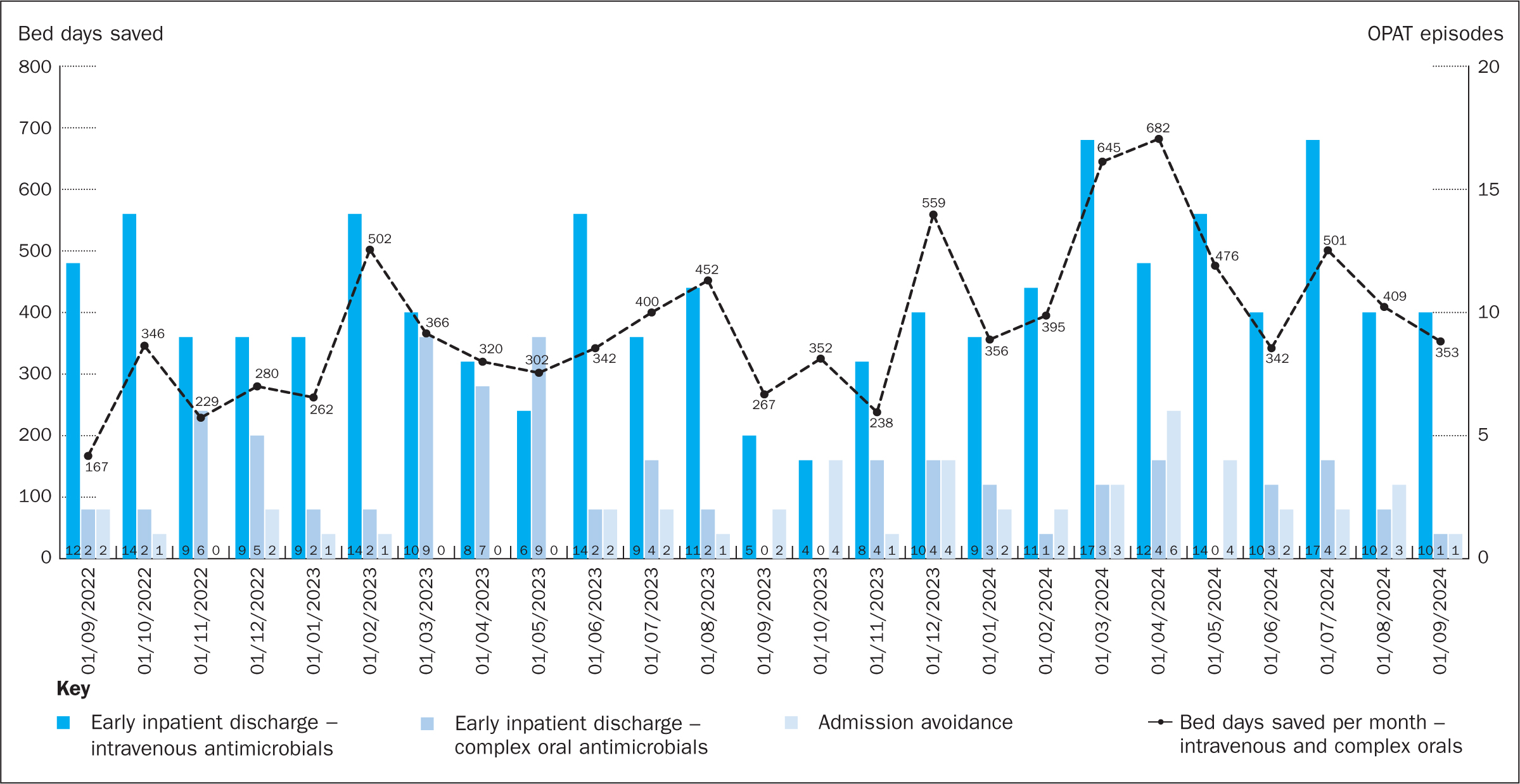
High hospital occupancy rates place significant pressure on resources, creating a demand for strategies to shorten hospital stays (Page et al, 2024). OPAT offers a practical alternative option for those who are medically stable and able to handle their treatment at home (Mohammed et al, 2024; Peter et al, 2024). This reduces the risk of healthcare-associated infections, improves patient comfort and quality of life, and lowers readmission rates and hospital length of stay, leading to better overall outcomes (Williams et al, 2015; Al Shareef et al, 2022). This also results in freeing up critical resources, such as beds and staff, to manage and care for more acute cases (Reidy et al, 2024). Figure 2 shows the number of bed days saved between 2022 and 2024 at King's College Hospital as identified in the review undertaken by the authors.
OPAT is widely recognised to be safe and cost-effective (Jones et al, 2015). Financial analyses consistently highlight the role of OPAT in reducing expenditure related to prolonged hospitalisations and resources use, with estimates putting potential annual cost savings at millions for large healthcare networks where OPAT protocols have been implemented (Alexander et al, 2020).
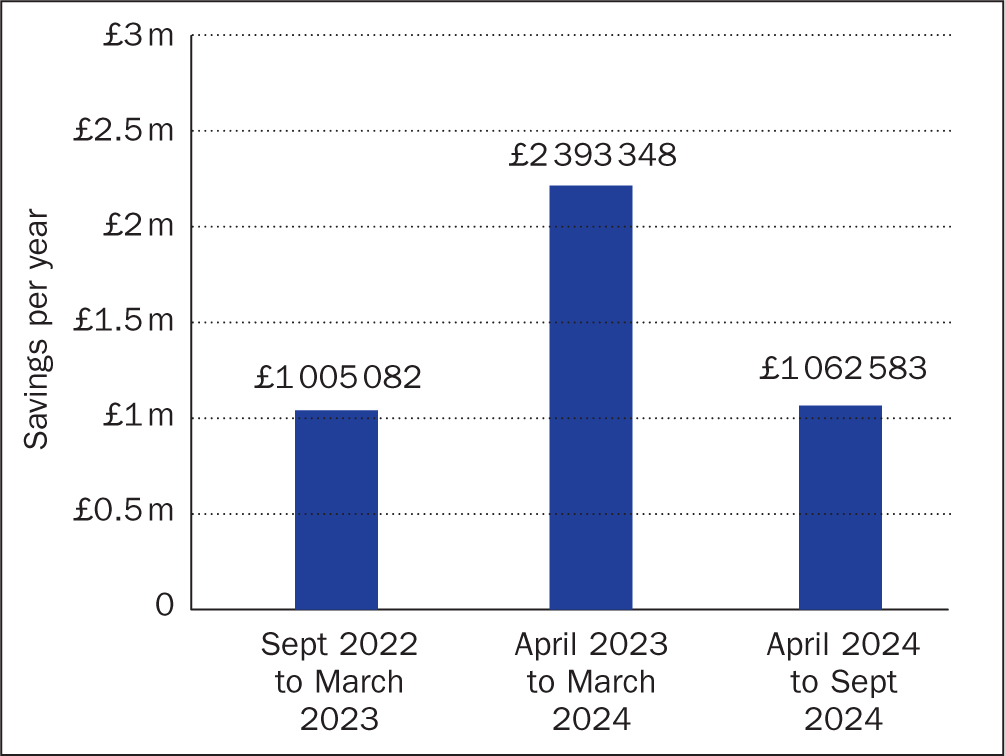
The financial savings based on hospital bed cost per day, which have been enabled by the implementation of the OPAT service at King's College Hospital are substantial: Figure 3 shows the estimated financial savings between September 2022 and September 2024.
OPAT patient satisfaction
Figure 4 provides an overview of the 2-year King's College Hospital OPAT patient experience survey, spanning September 2022 to September 2024. The findings indicate that patients who participated in the OPAT programme reported high satisfaction levels and expressed a preference to continue their intravenous antibiotics treatment at home. However, certain groups, such as patients with complex social circumstances and those experiencing anxiety about home-based treatment, expressed a preference for completing their antibiotic courses within the hospital setting.
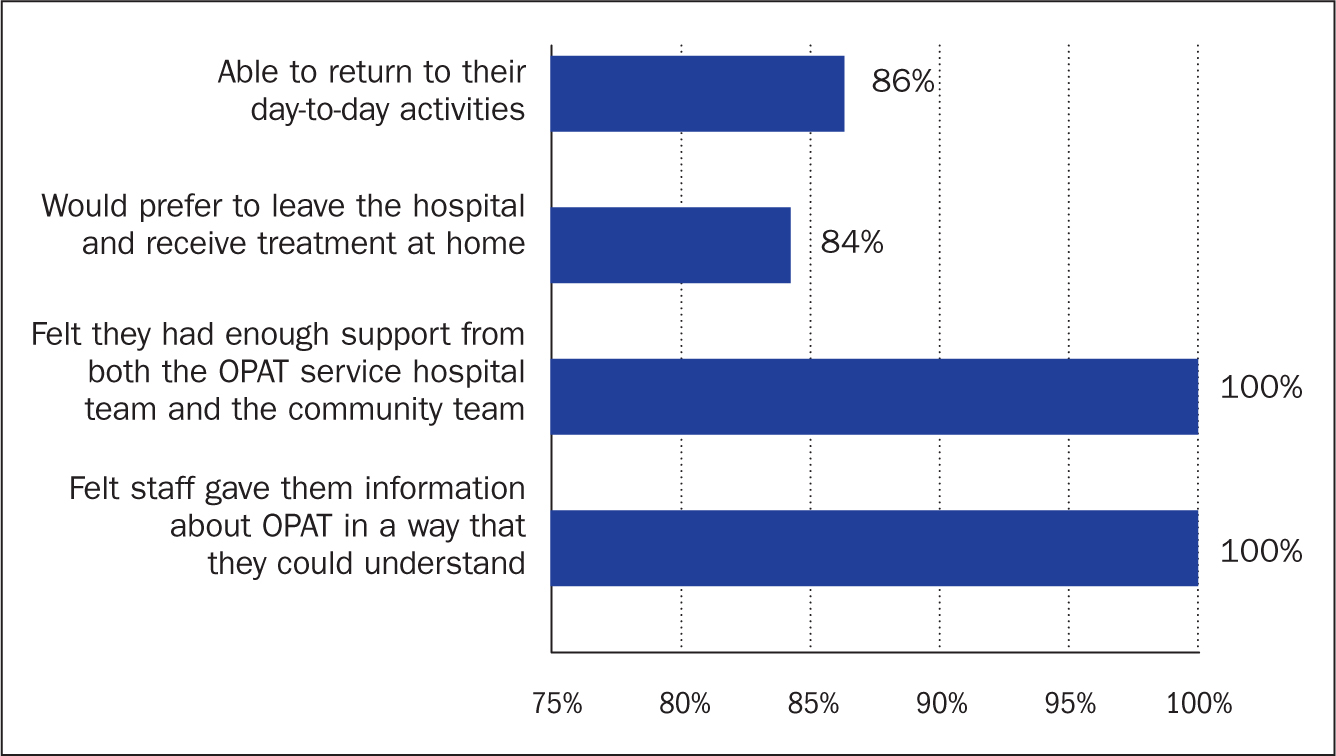
Twiddy et al (2018) has highlighted areas of patient dissatisfaction, such as the scheduling of nursing visits, restrictions on lifestyle due to strict antibiotic regimens, and anxiety associated with managing illness at home. These insights underscore the importance of addressing logistical and emotional challenges to enhance the overall patient experience and satisfaction with OPAT services.
Patients' ability to continue treatment at home or in a less restrictive setting contributes to a better patient experience, with positive feedback on the relevant information provided and on the support patients have had despite not being physically in the hospital (Soni et al, 2024). This has been shown to improve treatment adherence and enhance their overall recovery (Hamad et al, 2020). Below are some of the patient feedback received, which was collected from patients attending follow-up clinics between September 2022 and September 2024, collected through the hospital's online survey.
‘I am getting in control of my own time because I am now doing the antibiotics by myself. I have more time to spend on my family.’
‘Service received was professional and made me feel as if I was the only patient.’
‘I really appreciate their service and care towards us. The appointment process has [been] co-ordinated in a good and easy manner.’
‘It's been really helpful for me, as it has helped me avoid a long hospital stay.’
‘Very supportive workers and communication is frequent, so I know what is happening.’
‘The service [that] nurses provide is great, but they need to arrive in time as they recommend, sometimes we do need to be out but cannot go.’
‘I am so pleased to be able to go home before Christmas. Team has made the transition so smooth and was very thorough in the explanation of what I should be expecting. The home nurse was brilliant as well in teaching me, and I am now able to do my antibiotics myself. I know I am in good hands with the OPAT service.’
‘The OPAT team have been fantastic. Very communicative, clearly explaining things and very supportive. They've made the treatment a lot easier to manage with their support.’
‘Reliable timing for nursing visits [is important]. It varies every day. It would be good to have it at the same time every day.’
‘The video tutorial was extremely helpful in preparing me to run through self-administered antibiotics, more helpful than the paper copies, I would say.’
‘Having the OPAT team and helping me to get back home earlier by self-administered antibiotics was fantastic for me and my family.’
‘They supported me with learning how to take the antibiotics and their positivity has really helped make the illness much more manageable.’
OPAT patient outcomes
King's OPAT programme has demonstrated significant success in its patient outcomes. Figure 5 presents patient outcomes for the period between September 2022 and September 2024. The data showed that 73% ofpatients experienced an uncomplicated course of treatment through OPAT. However, 19% of cases were classified as complicated due to factors such as unplanned changes in antimicrobial therapy, adverse events, including brief readmissions of less than 24 hours related to the OPAT episode, and vascular access complications.
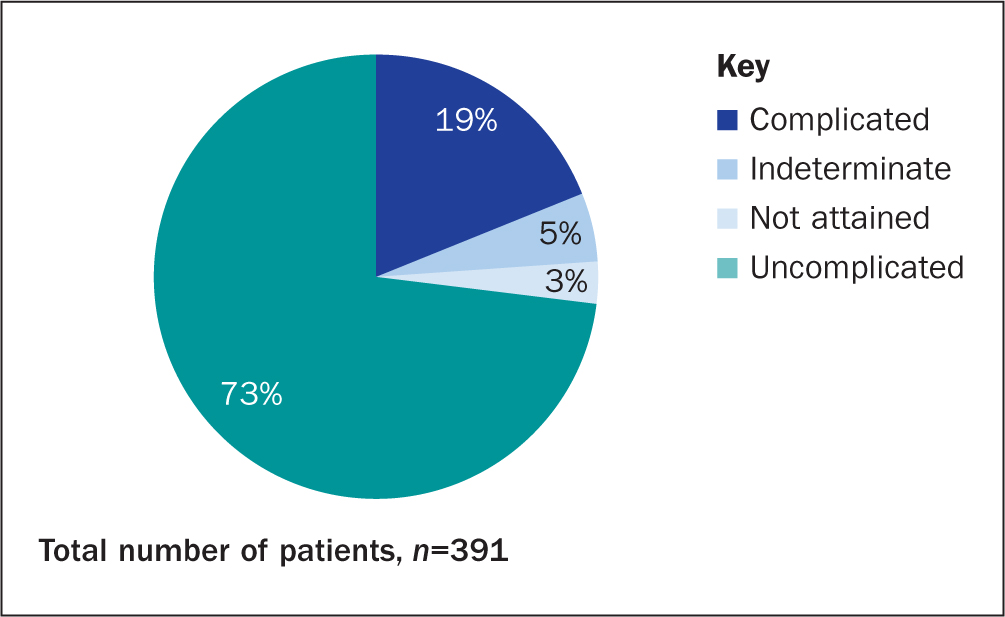
Notably, only 3% ofpatients did not achieve their anticipated OPAT treatment outcomes. These cases were attributed to failure to complete the planned therapy for reasons other than unrelated readmissions, worsening infections necessitating hospital readmissions, or readmissions lasting 24 hours or more for causes directly related to OPAT, including adverse events. These findings highlight the programme's efficacy while underscoring areas where further improvements are warranted to enhance patient outcomes.
Discussion
The implementation of OPAT at King's College Hospital NHS Foundation Trust represents an innovative approach to healthcare delivery, offering cost-effective and patient-centred alternatives to traditional inpatient care. This retrospective review highlights the programme's ability to save resources, enhance patient outcomes, and provide significant financial benefits to the NHS. Over 2 years, OPAT saved 9516 hospital bed days, demonstrating its capacity to alleviate pressures on healthcare infrastructure while achieving annual savings of £1—2 million.
Multidisciplinary collaboration: a foundation for success
King's OPAT success lies in its robust multidisciplinary framework, which integrates infectious disease specialists, microbiologists, pharmacists and specialist nurses to deliver personalised and safe care. This collaborative approach ensures that a thorough patient assessment takes place, addressing not only medical stability but also social and logistical factors that may impact treatment outcomes (Durojaiye et al, 2018). By applying carefully defined inclusion and exclusion criteria, the programme effectively identifies suitable candidates for OPAT, minimising the risk of complications and hospital readmissions (Hatcher et al, 2019).
The programme's partnership with external providers, such as Baxter and Bionical Health, has further expanded its reach, enabling seamless transitions from hospital to home-based care. These collaborations highlight the importance of integrating external resources to optimise service delivery and maintain high standards of care.
Tailored approaches to patient care
OPAT's adaptability to diverse patient needs is a key strength. The programme accommodates both self-administration and fully nursed care, depending on a patient's capabilities. Training patients in traditional antibiotic preparation methods or premixed elastomeric devices empowers them to self-administer their therapy and enables them to take control of their treatment, aligning with modern healthcare principles that prioritise patient autonomy (Soni et al, 2024).
However, not all patients are eligible for self-care. Barriers such as mental health challenges, unstable home environments, and lack of family support prevent some individuals from participating in OPAT. Addressing these barriers is critical for ensuring equitable access and outcomes. Strategies such as providing additional social support, establishing community care hubs, or exploring hybrid care models that combine outpatient and inpatient care may enhance accessibility for underserved populations.
Financial Impacts of OPAT
A key advantage of OPAT is its ability to reduce healthcare costs significantly (Alexander et al, 2020). Prolonged inpatient stays, which can cost the NHS between £300 and £600 per day, place a considerable strain on limited healthcare resources (Guest et al, 2020). By shifting care to outpatient settings, OPAT reduces these costs, while maintaining high-quality care (Dimitrova et al, 2021).
The financial burden of inpatient care, including the costs associated with hospital infrastructure, nursing care, and daily stays, is much higher than the costs of providing outpatient therapy (Bouzigard et al, 2024). OPAT enables healthcare systems to allocate resources more efficiently, lowering overall treatment costs while maintaining high-quality care (Vargas-Palacios et al, 2017).
The programme's financial benefits extend beyond direct cost savings. By freeing hospital beds and staff, OPAT enables hospitals to allocate resources more effectively, focusing on acute cases requiring intensive care. This capacity optimisation is especially critical for addressing systemic challenges such as rising patient volumes and staff shortages. The demonstrated financial savings at King's highlight OPAT's potential to contribute significantly to NHS sustainability.
Enhancing patient satisfaction
Patient satisfaction is a vital indicator of OPAT's success. Many patients have reported improved quality of life and greater autonomy due to the flexibility and comfort of home-based care in other studies (Hamad et al, 2020). At King's, positive feedback emphasises the programme's ability to empower patients and improve their overall treatment experience. For example, patients expressed gratitude for the freedom to manage their schedules and spend more time with family, which would not have been possible with prolonged hospital stays.
Nonetheless, some patients reported challenges related to nursing visit schedules and the anxiety associated with managing treatment at home. These insights suggest areas for improvement, such as offering more consistent visit timings and enhanced support systems. Digital tools, including telehealth platforms for remote monitoring and consultations, could further enhance the patient experience while reducing the burden on healthcare providers.
Clinical safety and efficacy
The clinical outcomes of OPAT underscore its efficacy as a safe alternative to inpatient care. About 73% of patients experienced uncomplicated treatment courses, while 18% faced complications such as adverse events or unplanned antimicrobial changes. Only a small percentage (3%) failed to complete treatment, reflecting the programme's stringent safety measures and multidisciplinary oversight (Chapman et al, 2019).
To further enhance safety, ongoing monitoring of vascular access devices and proactive management of potential complications are essential. The incorporation of advanced technologies, such as automated infusion systems and wearable devices for real-time monitoring, may help reduce the incidence of complications and improve overall outcomes.
Broader implications and future directions
The success ofOPAT at King's College Hospital NHS Foundation Trust highlights its potential for broader implementation across healthcare systems. Scaling up OPAT services can significantly reduce hospital occupancy rates, improve resource allocation, and enhance patient outcomes. However, achieving this requires key challenges to be addressed, including standardising protocols, ensuring equitable access, and investing in infrastructure and training.
Future research should focus on evaluating the long-term outcomes of OPAT, including its impact on population health, healthcare system efficiency, and patient satisfaction. Investigating the role of emerging technologies, such as telemedicine and remote monitoring tools, can also provide valuable insights into how OPAT can be further optimised.
Overall, the OPAT programme at King's demonstrates a transformative approach to infection management, achieving substantial savings in hospital bed days, financial costs, and healthcare resources. Its multidisciplinary, patient-centred model ensures high levels of clinical safety, efficacy and patient satisfaction, making it a benchmark for resource-efficient healthcare delivery.
Although challenges remain, such as addressing social barriers and patient preferences, the programme's success underscores the need for continued investment and expansion. By adopting similar models across healthcare systems, OPAT has the potential to revolutionise outpatient care, contributing to sustainable healthcare solutions and improved patient outcomes.
Recommendations
The successful implementation of OPAT at King's College Hospital NHS Foundation Trust highlights its value in reducing hospital stays, lowering healthcare costs, and enhancing patient satisfaction. Given the documented savings of 9516 hospital bed days and estimated financial benefits of £1—2 million annually, expanding OPAT services across additional NHS trusts is recommended. Such expansion should emphasise comprehensive eligibility assessments and a multidisciplinary approach, ensuring patients receive safe and effective care at home. Further investment in training and resources for self-administered OPAT could maximise accessibility, ultimately supporting the NHS goals of efficient resource utilisation and improved patient outcomes.
Conclusion
The OPAT programme at King's College Hospital NHS Foundation Trust demonstrates a powerful model for reducing hospital demand, improving patient outcomes, and achieving significant cost savings. Through its innovative approach, OPAT has effectively decreased the strain on inpatient resources, saving thousands of bed days and offering substantial financial benefits. The programme's multidisciplinary structure and patientcentred care have led to high patient satisfaction, particularly by allowing treatment in home settings. These results suggest that wider adoption of OPAT could enhance healthcare efficiency across the NHS, aligning with national goals to optimise resource use while maintaining high standards of care.


