It is estimated that between 176 000 and 205 000 people in the UK live with a stoma and about 13 500 to 21 000 undergo stoma surgery each year (Aibibula et al, 2022). This surgery is often a life-saving intervention, yet many people subsequently struggle with psychosocial and physical problems caused by stoma-related complications, such as leakages (Richbourg et al, 2007; Claessens et al, 2015; Jeppesen et al, 2022). Leakage of stomal effluent underneath the baseplate, especially when leakage progresses beyond the baseplate and soils clothes, significantly impacts an individual's quality of life (QoL) (Jeppesen et al, 2022).
Besides causing psychological distress for the individual, stomal effluent on the skin is a key aetiological factor for peristomal skin complications (PSCs) (Voegeli et al, 2020). PSCs are a common problem for people with a stoma (Herlufsen et al, 2006; Colwell et al, 2017; Salvadalena et al, 2020; Voegeli et al, 2020), with one study (Fellows et al, 2021) showing that 9 out of 10 people experience PSCs to varying degrees. People with PSCs have in different studies reported lower QoL compared with people not troubled with a PSC (Erwin-Toth et al, 2012; Hedegaard et al, 2020).
Skin discolouration or damaged skin are visual signs of PSCs; however, many people experience non-visual symptoms, including pain, itching and burning sensations, even in the absence of skin discolouration (Fellows et al, 2021). The high variability in the reported prevalence of PSCs may be due to a lack of a standardised method and terminology to assess the peristomal skin. Moreover, many of those diagnosed with a peristomal skin disorder by a dermatologist may not necessarily perceive that they have a skin disorder (Herlufsen et al, 2006). Recently an updated, validated tool for the assessment of peristomal skin, the Ostomy Skin Tool 2.0, was published that captures both visual signs and non-visual symptoms of PSCs to better assess severity. It can be used by both health professionals and people with a stoma (Martins et al, 2022a).
In a recent consensus (Aibibula et al, 2022), patient groups highlighted the problems experienced by people with a stoma in the UK, leading to multiple calls to action to improve stoma care in the country. For example, there is limited direct dermatological support for stoma patients in the UK, and it has been suggested that better access to specialist dermatology advice could potentially reduce the impact of PSCs (Aibibula et al, 2022). Furthermore, people with a stoma in the UK have been surveyed about research priorities within stoma care, where research on leakage and appliance problems was ranked as the top priority (Hubbard et al, 2017). Nonetheless, research-based evidence is lacking about the current level of complications experienced by people with a stoma in the UK. This article aims to offer insights into the current level of complications and unmet needs of people living with a stoma, supply healthcare providers with data to plan and deliver specialist stoma care services and improve the overall quality of care for people living with a stoma.
Methods
The Ostomy Life Study 2019 was an online, retrospective, self-reported questionnaire developed by Coloplast A/S (Martins et al, 2022b). A total of 54 614 people living with a stoma from 17 countries (the USA, Canada, Brazil, China, Australia, Japan and 11 countries in Europe) were invited to participate. A subset of the dataset concerning only respondents from the UK was used for analysis in the present study.
A comprehensive questionnaire was presented to respondents (excluding those irrigating their colostomy) that contained questions on demographics and respondents' stoma characteristics, self-reported leakage incidents, worry about leakage, ability to work, PSCs, the impact of leakage on QoL and access to stoma care nurses (SCNs). Every question had predefined response options, which are highlighted in each figure legend. Some questions had the option ‘other reason’, coupled with the opportunity to write a free-text answer. A total of 301 individuals from the UK completed the questionnaire.
The impact of leakage on everyday life for people with a stoma was assessed using the validated Ostomy Leak Impact (OLI) tool (Nafees et al, 2018). Respondents self-assessed the condition of their peristomal skin by answering questions from the Ostomy Skin Tool 2.0 (Martins et al, 2022a). Pictures of the respondents' own peristomal area were unavailable. Hence respondents could choose between seven illustrations displaying different levels of skin discolouration and skin areas with discolouration (Martins et al, 2022a).
The types of leakages were described to the respondents prior to the part of the survey that elicited information about leakage incidences and their impact. Leakage was defined as either stomal effluent observed underneath the baseplate during baseplate change or stomal effluent outside the baseplate (eg on clothes).
Exclusion criteria for using the individual questionnaire in the analysis were: if all the questions were answered within 15 minutes (the questionnaire was estimated to take 30 minutes to complete), if more than 30% of the answers were ‘do not know’, or if the participant did not complete the survey.
Statistics
Descriptive statistics were conducted in Microsoft Excel. A one-way analysis of variance (ANOVA) was performed, followed by Dunnett's multiple comparisons test to compare OLI scores between groups (GraphPad Prism v9.0.0 for Windows, GraphPad Software, San Diego, CA).
Ethical approval and consent to participate
Before answering the survey, all participants consented to taking part and allowed Coloplast A/S to use the collected, aggregated and anonymous data for internal and publication purposes.
Results
Demographics of respondents
A total of 301 people with a stoma from the UK completed the questionnaire. In this survey population, 54% (n=164) were male and 67% (n=203) were aged 60 years or older (Table 1). About 28% (n=83) of respondents worked full time or part time, 62% (n=187) were retired and the remainder reported other occupational status. Regarding stoma type, 32% (n=96) had a colostomy, 52% (n=158) had an ileostomy or jejunostomy, and 17% (n=52) had a urostomy; 2% (n=5) of respondents reported having more than one stoma. Most respondents (90%; n=269) had had their stoma for at least 5 years, while 10% (n=32) had had a stoma formed within the preceding 5 years (Table 1).
Table 1. Demography and characteristics of respondents (n=301)
| n (%) | |
|---|---|
| Age | |
| Below 39 years old | 24 (8) |
| 40–59 years old | 73 (24) |
| 60 years or older | 203 (67) |
| Do not wish to answer | 1 (0) |
| Gender | |
| Male | 164 (54) |
| Female | 137 (46) |
| Do not wish to answer | 0 (0) |
| Stoma type | |
| Colostomy | 96 (32) |
| Ileostomy or jejunostomy | 158 (52) |
| Urostomy | 52 (17) |
| More than one stoma | 5 (2) |
| Do not know | 5 (2) |
| Time since surgery | |
| 0–12 months | 3 (1) |
| 1–2 years | 3 (1) |
| 3–4 years | 26 (9) |
| 5–10 years | 135 (45) |
| >10 years | 134 (45) |
| Do not wish to answer | 0 (0) |
| Occupation | |
| Retired | 187 (62) |
| Working full time | 54 (18) |
| Working part time | 29 (10) |
| Other | 30 (10) |
| Do not wish to answer | 1 (0) |
NB. Percentages have been rounded to nearest 1%
Frequency of leakage
People with a stoma in the UK commonly experienced leakage of stomal effluent underneath the baseplate and/or onto clothes even though most respondents had had their stoma for longer than 5 years. About 86% (n=260) of respondents had experienced leakage underneath the baseplate within the preceding month, and nearly half (46%; n=138) had experienced leakage at least once within the preceding week (Figure 1a). Approximately 12% (n=36) experienced leakages of stomal effluent underneath the baseplate daily.
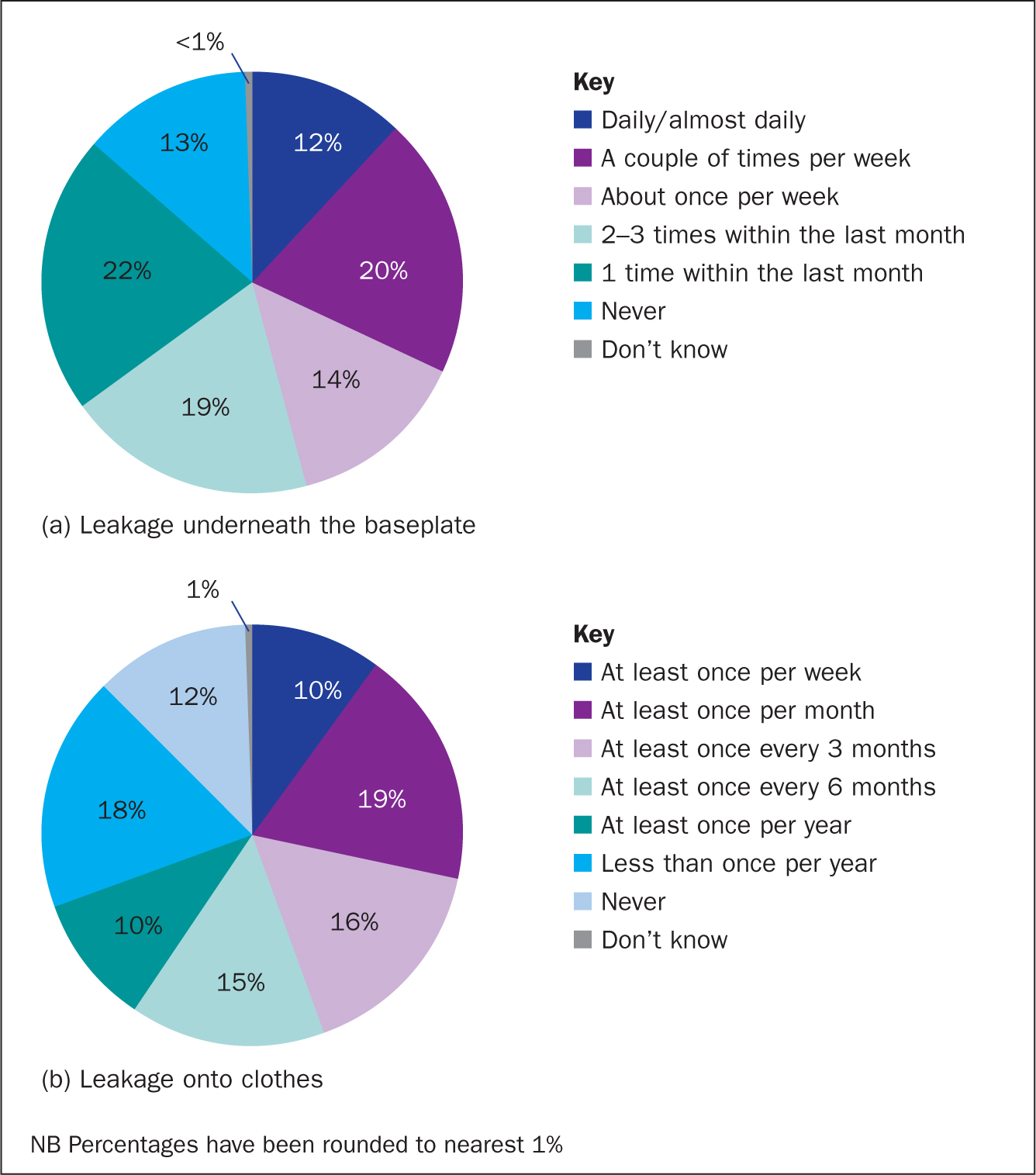
About two-thirds (69%; n=208) of respondents reported having leakage of stomal effluent onto clothes within the preceding year, with as many as 28% (n=85) experiencing this monthly (Figure 1b).
Worry about leakage
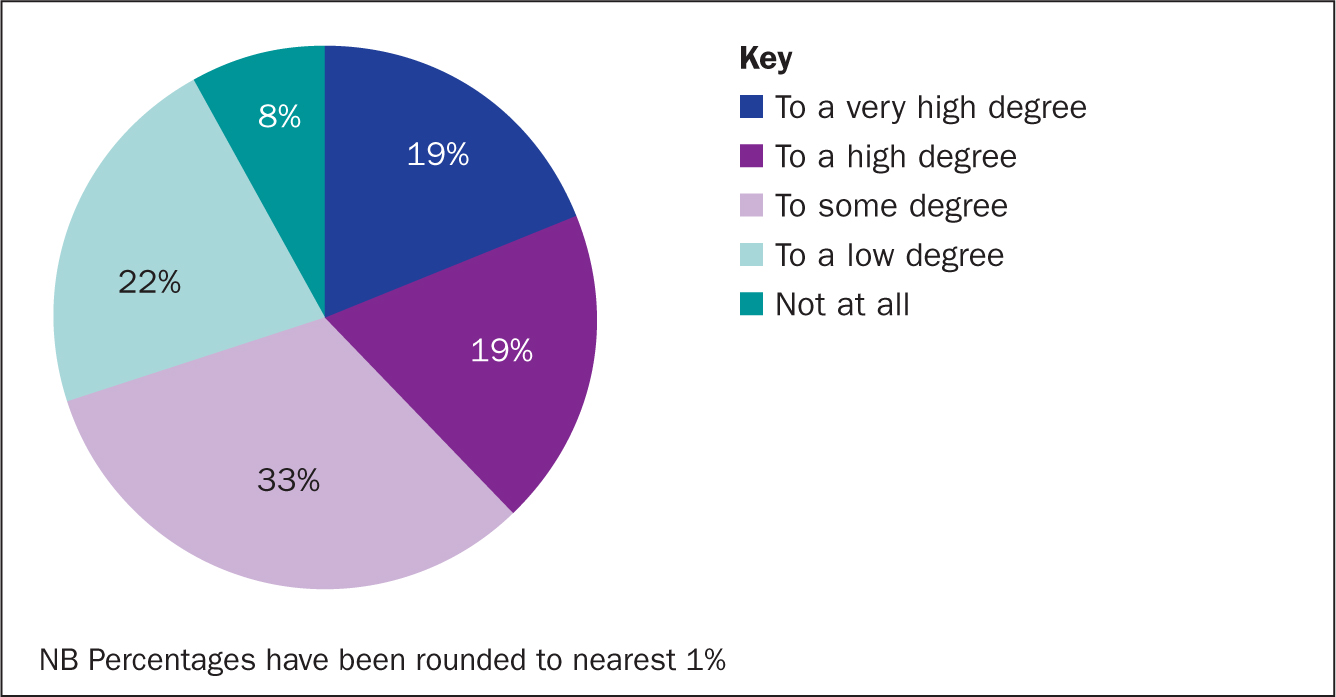
Based on a five-point Likert scale, ranging from ‘very high’ to ‘not at all’, 92% (n=277) of participants worried about leakage to varying degrees (Figure 2) and only 8% (n=24) scored their worry about leakage as ‘not at all’. The proportion who reported worrying about leakage to a ‘high’ or ‘very high’ degree was 38% (n=114) (Figure 2).
Worry about leakage impacts quality of life and work
Worrying about leakage of stomal effluent had a profound negative psychosocial impact on individuals living with a stoma (Figure 3a). The higher the worry about leakage, the greater the impact in all three domains of the OLI tool. In particular, individuals worrying about leakage to a ‘high’ or ‘very high’ degree experienced a more significant impact in all three domains compared with individuals who responded ‘not at all’, meaning that they experienced a greater degree of frustration and embarrassment, as well as social isolation, than those not worrying about leakage.
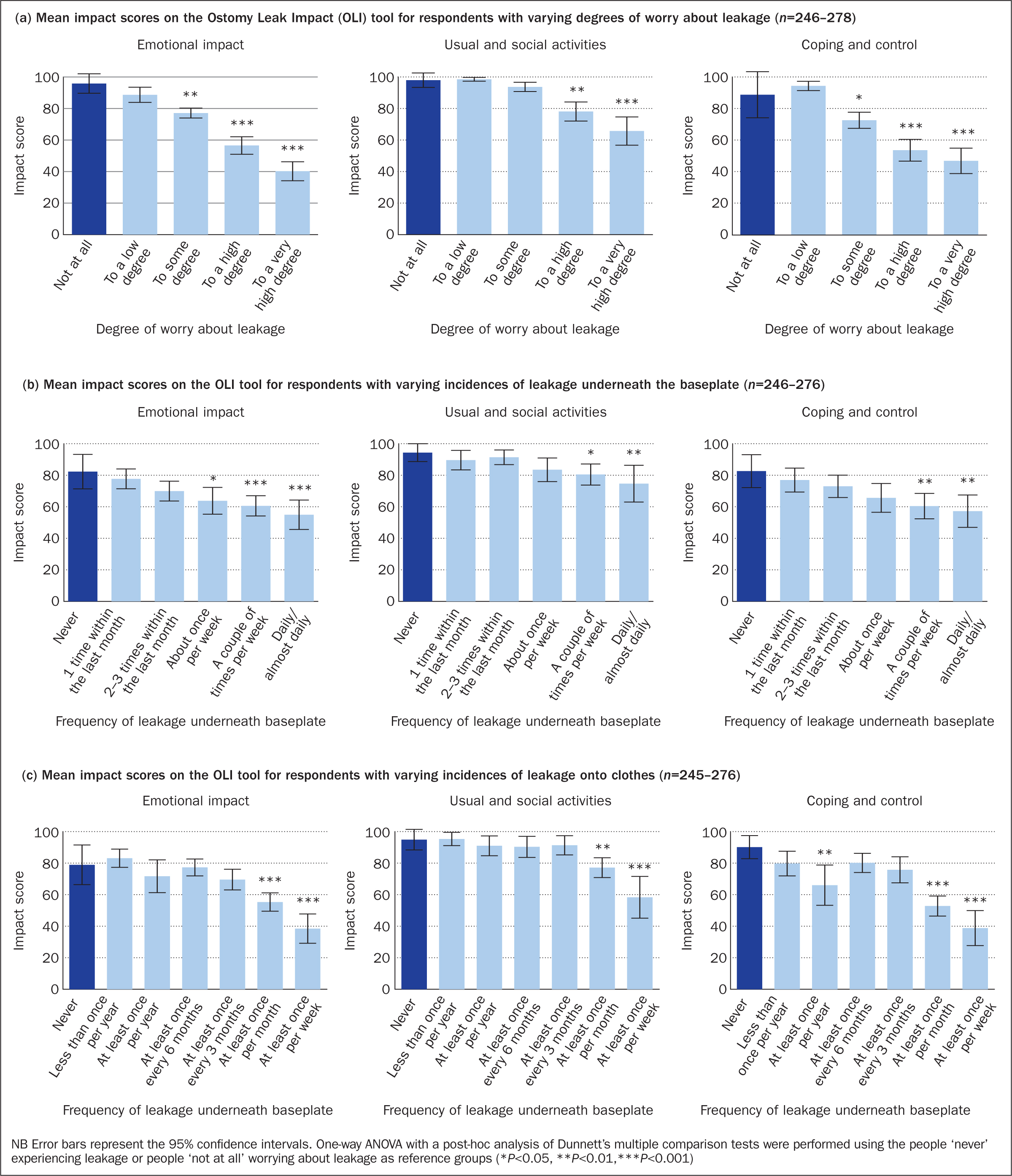
Concern about leakage is interrelated with the frequency of experiencing leakage (Jeppesen et al, 2022) and, indeed, the frequency of experiencing leakage underneath the baseplate and/or onto clothes is also correlated with a more significant impact in all three domains of the OLI tool (Figure 3, b–c).
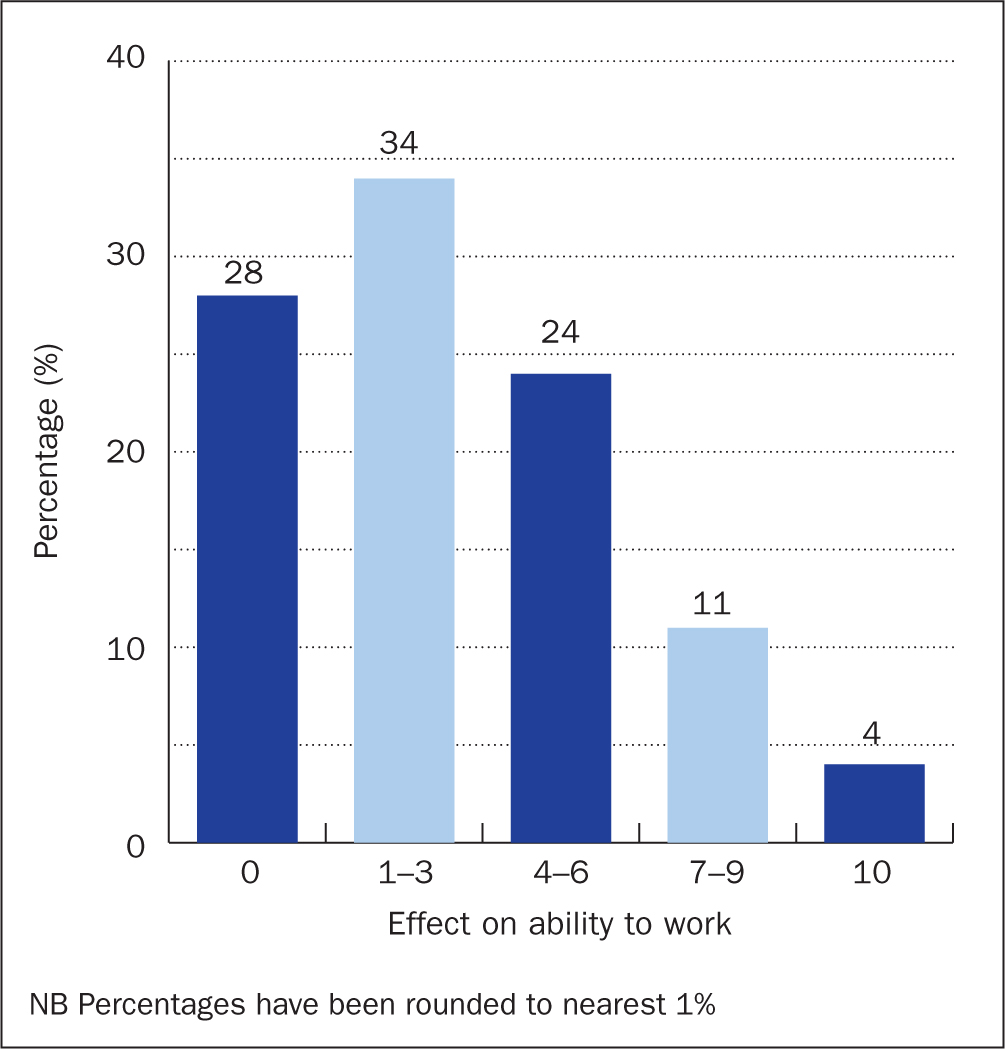
In addition to having a negative psychosocial impact, concern about leakage also affected some individuals' ability to work (Figure 4), with 4% (n=3) reporting that worry about leakage prevented them from working completely and 11% (n=9) reporting that it had a high impact (score 7–9) on their ability to work. No impact of leakage on the ability to work was reported by 28% (n=23).
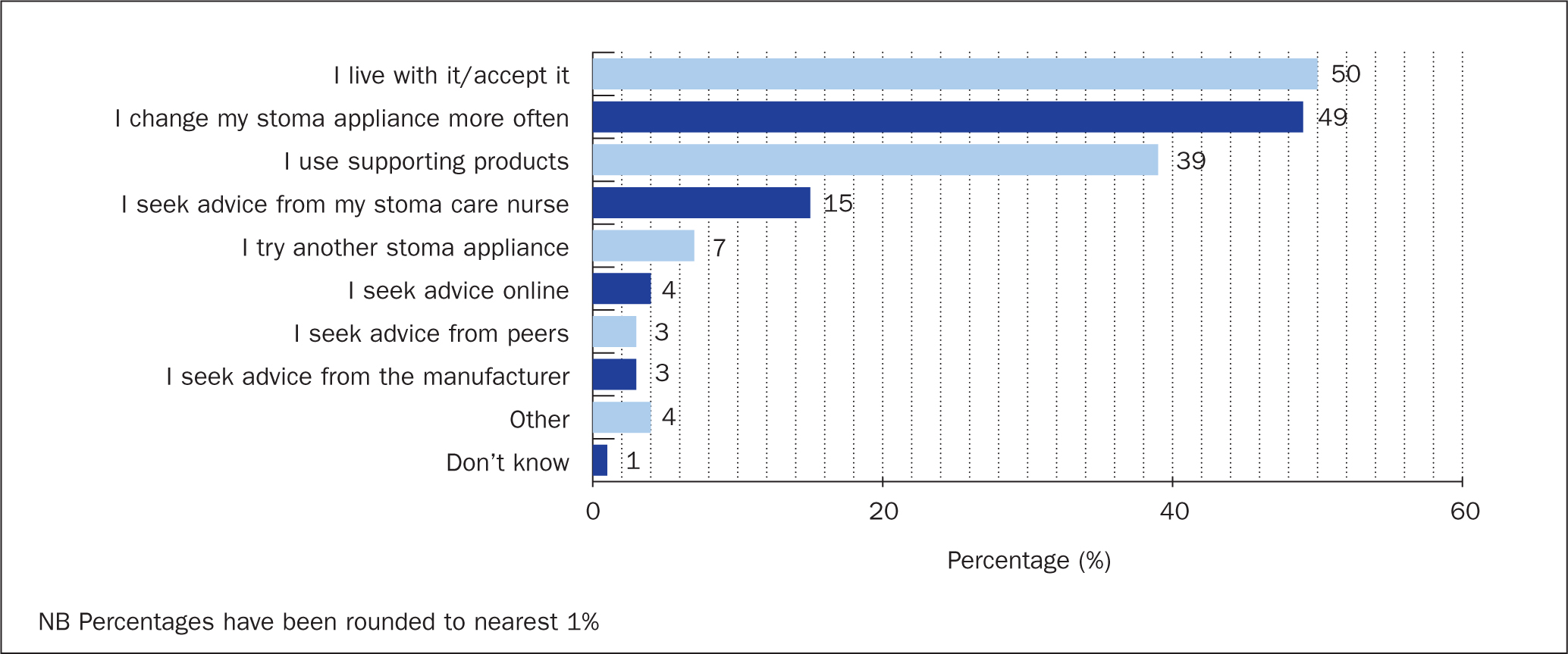
Actions taken when worrying about leakage
Half the respondents (50%; n=151) reported that they lived with worry about leakage, and only a few sought advice from an SCN (15%; n=45), online resources (4%; n=13), their peers (3%; n=8) or the product manufacturer (3%; n=8). However, due to the worry about leakage, about half (49%; n=146) reported changing their stoma appliance more often and 39% (n=118) reported using supporting products (accessories) (Figure 5).
Main reasons for experiencing leakage
Respondents were asked about the main reasons for leakage incidents. Half (49%; n=148) said it was related to the intake of specific foods (Table 2). Many also found it difficult to get a good fit of the stoma appliance to the body because of features such as skin creases or folds (28%; n=83) or experienced poor adhesion of the stoma appliance to the skin due to PSCs (23%; n=70). A few reported a lack of access to enough stoma appliances (1%; n=3), supporting products (3%; n=10), or stoma appliances with the correct body fit (ie flat, convex, concave) (5%; n=14).
Table 2. Respondents' perception of main reason(s) for experiencing leakage
| Statement | n (%) |
|---|---|
| Food related (eg when eating certain foods) | 148 (49) |
| It is difficult to get a good fit of the stoma appliance to my body (eg due to creases, fold, hernia) | 83 (28) |
| Due to skin complications (making it difficult to get a good adhesion to the skin) | 70 (23) |
| I don't always change as often as I should | 54 (18) |
| The area around my stoma has changed in shape making it difficult to get a good fit with my current appliance | 29 (10) |
| I don't always take the time to follow my change routine | 28 (9) |
| Due to poor stoma construction (eg my stoma is below or at skin level) | 27 (9) |
| I don't have access to a stoma appliance that suits my body | 14 (5) |
| The hole in the baseplate is cut wrong and/or is too small/big | 12 (4) |
| I don't have access to enough supporting products (eg tape, rings, paste) | 10 (3) |
| I don't have access to enough stoma appliances | 3 (1) |
| Other | 76 (25) |
| Don't know | 27 (9) |
NB Percentages have been rounded to nearest 1%
Peristomal skin complications
Self-assessment of the peristomal skin among the 301 respondents revealed that only 18% (n=53) had no PSCs and the remaining respondents (82%) had PSCs to varying degrees (Figure 6a). ‘Severe’ PSCs were reported by 47% (n=141) of respondents, 13% (n=39) had ‘moderate’ PSCs, 20% (n=60) ‘mild’ PSCs and 3% (n=8) had PSCs that did not require treatment.
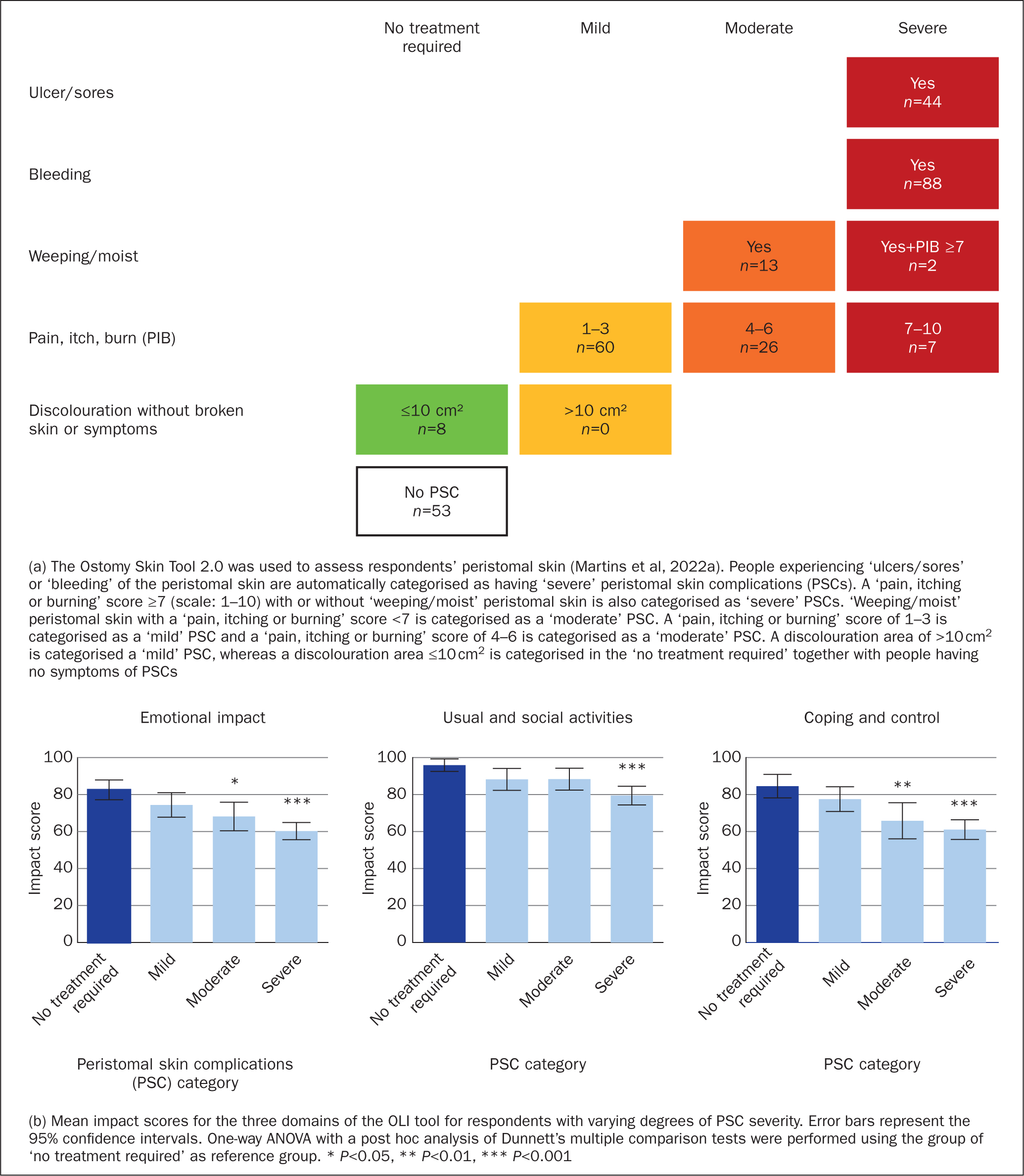
The severity of PSCs had a profound impact on individuals' QoL (Figure 6b). People with ‘severe’ PSCs experienced a more significant impact in all three domains of the OLI tool compared with people without PSCs or PSCs that did not require treatment. People with ‘moderate’ PSCs were also more impacted in the ‘emotional’ and ‘coping and control’ domains, while individuals with ‘mild’ PSCs had similar impact scores as those without PSCs or with PSCs that did not require treatment.
Access to stoma care nurses
Seventy-three percent of the respondents (n=219) reported having access to SCN consultations when needed (Figure 7a). Of those with access to an SCN, 59% (n=130) were in contact with an SCN at least once a year, while many (39%; n=86) had never had contact with an SCN, even though they had been offered the opportunity (Figure 7b).
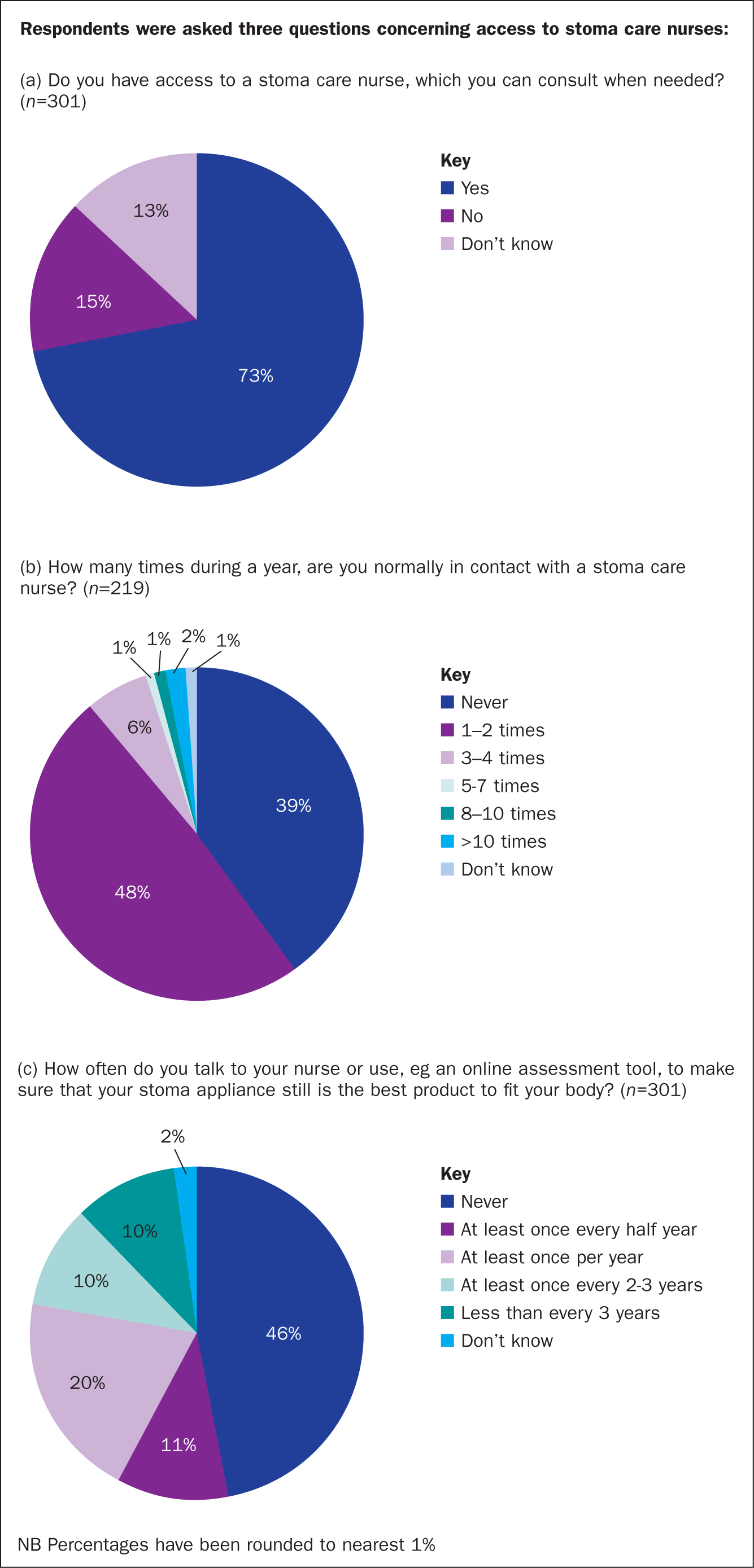
About half the respondents (46%; n=139) never talked with a nurse or consulted online tools to assess whether their existing stoma appliance was still the optimal solution for their body type. In addition, only 31% (n=93) had such an assessment on an annual basis (Figure 7c).
Discussion
This study highlights stoma-related complications experienced by many people with a stoma in the UK, regardless of when they had their stoma formed. Almost half the respondents experienced weekly episodes of leakage underneath the baseplate and 28% (n=85) reported monthly incidents of leakage onto clothes. These findings support other studies from the UK, highlighting that leakage is a problem for many people with a stoma (Hubbard et al, 2017; Aibibula et al, 2022), and that leakage is a problem that persists several years postoperatively (Pearson et al, 2020). Interestingly, 49% (n=148) thought that the main reason for experiencing leakage was related to food. Another study found that a significant proportion of people with a stoma adjusted their dietary intake and avoided specific foods to reduce the risk of leakage and odour, which may increase the risk of nutritional deficiencies (de Oliveira et al, 2018).
Although further investigation of the dietary responses was not within our study parameters, the studies suggest a need for additional patient education around diet and lifestyle factors and improved information about stoma care products, which ultimately may increase patient confidence and enable them to have the lifestyle they desire. In addition to perceived food-related causes of leakage, a substantial proportion of respondents thought they experienced leakage due to difficulties in getting a good fit of the stoma appliance to the body (28%; n=83) or due to PSCs (23%; n=70). These issues could potentially be reduced through consultations with SCNs, since incorrect product usage has been rated by SCNs as one of the most important reasons for leakage issues (Down et al, 2021). In addition, SCNs have reported that they would expect to have multiple consultations to solve leakage issues (Down et al, 2021).
Most of the respondents in this study (82%; n=248) experienced PSCs to varying degrees and people with moderate and severe PSCs reported lower QoL compared with those without PSCs, which corroborates data from previous studies (Nybaek et al, 2010; Goldstine et al, 2019; Nichols et al, 2019). The proportion of people with PSCs in the UK is similar to the level reported for the global cohort (Fellows et al, 2021; Martins et al, 2022a). However, this relies on individuals' interpretation of their PSC, which could potentially be open to subjectivity. Nonetheless, the findings are similar to the reported prevalence of PSCs in the literature, which ranges from 16% to 88% (Ratliff et al, 2005; Herlufsen et al, 2006; Richbourg et al, 2007; Colwell et al, 2017; Salvadalena et al, 2020; Voegeli et al, 2020; Fellows et al, 2021). One reason for the considerable variation in reported levels of PSCs may be due to the non-systematic assessments of peristomal skin by different health professionals, highlighting the need for SCNs to use validated assessment tools to promote consistency and standardisation (Martins et al, 2022a). In addition, individuals need to be educated to understand ‘red flags’, which indicate when a specialist clinical review is needed. The education should include both leakage and PSC so that timely review can be initiated and an opportunity for the SCN to triage and refer to relevant medical colleagues if required.
The high prevalence of stoma-related complications, such as leakage issues and PSCs, in the UK might be explained by the fact that 39% (n=86) of respondents who had access to SCNs never took up the opportunity. Moreover, half the respondents never talked with SCNs or used online assessment tools to investigate whether their existing stoma appliance was the optimal solution for their body type. The potential lack of consultations with SCNs may have negative consequences for the individual and also for the healthcare system. SCN consultations have previously been shown to help reduce the severity of PSCs (Harputlu and Özsoy, 2018) and may contribute to improving QoL for people with a stoma (Erwin-Toth et al, 2012). The lack of access to SCNs or not using the existing SCN resources may thus have a negative impact on an individual's physical and psychosocial wellbeing, caused by stoma-related complications. Prevention or minimising the risk of developing PSCs, as well as early detection of PSCs by SCNs, may provide substantial cost reductions to the healthcare system, since PSCs are costly to manage (Martins et al, 2012; Meisner et al, 2012; Taneja et al, 2017).
Moreover, support from SCNs can improve patient-reported outcomes, reduce the economic burden and wastage associated with stoma care expenditure in the UK health system, and provide additional cost-efficiency savings, eg through the reduction in readmissions to hospital (Carter, 2020).
Nine out of ten respondents from the UK worried about leakage to varying degrees, which is similar to the findings for the global cohort (Jeppesen et al, 2022). Concerningly, half the UK respondents found it acceptable to live with the concern about leakage, in contrast to only 29% in the global cohort (Jeppesen et al, 2022). The reason(s) why a higher proportion of people with a stoma in the UK have accepted living with their worry about leakage compared with the global cohort was not explored in the present study, but it is an important topic for future research. QoL of individuals who worry about leakage was significantly impacted compared with those people who did not worry about leakage, as evidenced by the degree of frustration, embarrassment and social isolation. A significant proportion (50%) of people worrying about leakage had not yet accessed their specialist SCN services, the reason(s) for which was not explored as part of this study; however, future research should investigate this to improve patient care. It has previously been reported that there is an unmet need for equitable access to SCNs across the country (Aibibula et al, 2022). Easier access to SCNs may be needed, for example via remote consultations to reduce the burden of long-distance travel, as recently demonstrated in Norway where they have been using teleconsultations (Augestad et al, 2020). It should be noted that the present study was conducted prior to the onset of the COVID-19 pandemic in March 2020 and, due to the impact of the pandemic, SCNs have needed to review their practice and access to services, demonstrating flexibility in the provision of stoma care. As a consequence of the COVID-19 pandemic, SCNs in the UK reduced face-to-face consultations and changed these to telephone or online consultations to limit transmission of the coronavirus (Brewer and Coleman, 2021). The use of remote consultations was generally well received by most respondents, and remote consultations were perceived to be a valuable supplement in stoma care (Brewer and Coleman, 2021). However, the remote consultations had some limitations and were not perceived as a solution that could replace face-to-face consultations, especially in cases with stoma complications that needed to have a visual assessment (Brewer and Coleman, 2021). It will be interesting to see whether the greater availability of remote SCN consultations will increase the proportion of people consulting with SCNs to resolve stoma-related complications.
This study calls out multiple themes to improve stoma care. First, new solutions are warranted to provide better leakage control and thus reduce the associated impacts of leakage. Second, to better understand why many people with a stoma in the UK do not consult with SCNs even though they have the opportunity.
Considering the findings of this study, it is hoped that SCNs will consider the outcomes of this study and reflect on the implications for their services. Using validated tools for PSC assessment and standardisation, educating patients and colleagues regarding PSCs and addressing people's concerns about leakage will provide consistency and structure to the patient care pathway. In addition, appropriate review and access to specialist stoma care to improve psychological and physical outcomes for individuals living with a stoma will ultimately improve their QoL.
Limitations
Since the study population presented in this article was part of the global Ostomy Life Study 2019, this UK-focused study has some of the same general limitations as previously described (Jeppesen et al, 2022). In brief, the participants of this study were recruited from Coloplast A/S databases and were therefore either using or had previously used Coloplast A/S products. They may, therefore, not be entirely representative of individuals who use stoma appliances throughout the UK. However, there is no reason to believe that the stoma-related complications should be worse for people living with a stoma who are not in the Coloplast database. Therefore, prevalence and numbers are not expected to be systematically biased.
The respondents in the survey were dominated by individuals aged 60 years or above (67%; n=203) and most (90%; n=269) had had their stoma for over 5 years. The bias towards elderly and more experienced users means that the results cannot be generalised to the general stoma population in the UK. This further warrants analysis of how younger and newly operated people with a stoma are affected by stoma-related complications.
Individual subjectivity when reporting and interpreting PSC from the respondents will be influenced by the choice of illustrations, as well as their own experiences. It is unclear whether an alternative assessment tool would have provided a different response.
Recall bias may be a problem when administering retrospective, self-reported questionnaires, especially with regard to questions for which respondents have to recall events dating back to the preceding year.
Conclusion
Leakage of stomal effluent, and worry about leakage and PSCs are common issues and complications experienced by people with a stoma in the UK. Half the respondents to the survey had simply accepted living with the worry about leakage, which did not appear to be due to a lack of access to stoma appliances or supporting products. Most of the respondents had access to specialist SCNs, however, many did not use this opportunity to resolve stoma-related complications. The reason(s) why people did not use the opportunity to consult with SCNs remain unknown, however increased access to specialist SCNs via virtual appointments and increased clinic availability may be needed. Accurate triaging and assessment by the SCN may be needed to reduce the impact of leakage and its associated complications for people with a stoma in the UK.
KEY POINTS
- 92% of people with a stoma in the UK worried about leakage to varying degrees, which persisted for those who have had a stoma for >5 years
- 86% had experienced leakage underneath the baseplate within the preceding month
- 69% had experienced leakage onto clothes within the preceding year and 28% experienced this monthly
- Half the respondents simply accepted living with the worry about leakage
- 82% of respondents experienced peristomal skin complications to varying degrees
CPD reflective questions
- Think about the reasons why so many people with a stoma continue to experience leakages, regardless of when they had their stoma operations
- Consider the implications of leakage regarding subsequent peristomal skin complications and what could be done to prevent further problems, and how worrying about stoma leakage may affect a person's mental wellbeing, social interactions, work and the day-to-day life
- Consider how the nurse's role in selecting appropriate stoma appliances and providing regular reviews helps reduce leakage incidents and peristomal skin complications, as well as improves patients' overall quality of life. How frequently should reviews be undertaken, and where: in clinic/virtual/home visit?
- Reflect on the impact and cost of stoma complications to the healthcare system

