Peritoneal malignancy encompasses primary malignancy, which is relatively rare, and the much more common metastatic malignancy from a primary cancer. Any cancer can be the source of peritoneal metastasis but most commonly the primary is an abdominal tumour such as the colon, rectum, appendix, pancreas, stomach or gynaecological organs in women. In many cases peritoneal malignancy is not suitable for surgical resection but a subset of cases, particularly patients with pseudomyxoma peritonei originating from the appendix, are amenable to a combination strategy of what is called cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) (Bouquot et al, 2018). A similar treatment strategy is beneficial for selected patients with resectable colorectal peritoneal metastases or ovarian malignancies.
CRS aims to remove all abnormal tissues by complex surgical procedures and is combined with HIPEC to address residual disease after surgery. The concept of CRS was initially described by Sugarbaker (1994) and involves a laparotomy with peritonectomy procedures and resection of involved viscera, aiming to remove all macroscopic disease. In view of the specialist treatment required for patients with peritoneal malignancy, it has been recommended that they should be treated in highly specialised centres by clinicians and teams with specialist expertise in CRS and HIPEC (National Institute for Health and Care Excellence, 2004).
The Peritoneal Malignancy Institute in Basingstoke is one of highest-volume global centres in the treatment of patients with peritoneal malignancy, having performed over 3000 CRS and HIPEC operations since 1994. Patients are referred to the institute from all over the UK and those considered suitable for CRS and HIPEC, based on clinical details and radiological images, undergo outpatient review by a surgeon and a clinical nurse specialist (CNS). A full clinical and social history is documented, and an in-depth explanation of the diagnosis and treatment plan is provided. Patients are given written information to take home to read and they have open access to the CNS service to enable expert advice and support prior to admission. A full clinical encounter summary is sent to the patient in addition to the information booklets. Most patients do not return for pre-operative assessment appointments due to the added burden of travel for themselves and their relatives, with many living several hundred miles from Basingstoke.
The average inpatient stay for CRS and HIPEC is 21 days. Patients are discharged when medically fit and independent with their activities of daily living. Due to the complexity of the surgery and the geographical distances involved, it is imperative that discharges are well co-ordinated, and that information is shared between the teams caring for each patient, as well as with the patients themselves. On discharge from Basingstoke, patients return home to their local area of residence and are supported with nurse-led telephone follow-up from the CNS team in Basingstoke and shared care with the referring team and GP practice. Nurse-led telephone follow-up calls are undertaken at 1 week, 6 weeks and 3 months following discharge, and open access to the CNS service via a dedicated telephone number and recording system is maintained during the working week, outside of these scheduled calls.
An annual patient satisfaction survey is undertaken for all patients receiving treatment at the institute. In 2022, a question was incorporated to ask patients how confident they felt regarding their ongoing care following discharge. The responses identified a need to improve facilitation of ongoing care, with a focus on the transition between the specialist centre and the local area healthcare teams highlighted as being particularly challenging for patients.
A ‘treatment folder’ was designed by the team in response to this request to ensure patients were provided with comprehensive, concise information on their treatment and recovery. The folder was given to them before discharge. It contained copies of the clinic letters from the initial outpatient consultation, the operation letter, the ward discharge summary, discharge information leaflet, written information on build-up of diet, emotional support literature, post-splenectomy information (if required), holistic needs assessment information, and also the access details for completion of holistic needs assessment.
All patients are given standardised information as a minimum (letters and information books as outlined above) and the content of the folder is then personalised with further information specific to that individual's needs. All patients are seen by the peritoneal malignancy CNS team prior to discharge and the folder contents support the conversation and advice provided. Following implementation of the treatment folder, patients were asked for feedback to determine whether it met their needs and was a helpful addition in easing the transition from inpatient care to being at home.
Aims
The aims of the study reported in this article were:
- To obtain patient feedback on the implementation of the treatment folder
- To obtain feedback on the content of the folder
- To determine the optimum time for the folder to be provided
- To assess whether the provision of information in this way improves patient confidence on discharge following CRS and HIPEC.
Methods
A pilot retrospective qualitative study was undertaken following the implementation of the treatment folder, as a service improvement initiative. In total, 30 consecutive patients who were provided with the treatment folder ahead of discharge following CRS and HIPEC at the institute were sent a link to an online questionnaire via email, following a verbal discussion during the 6-week follow-up call with the CNS. With verbal consent obtained, participants were asked to provide feedback on whether the information in the folder was appropriate, was given to them at the right time during their treatment pathway and whether it enhanced patient confidence on discharge and enabled improved communication when accessing healthcare services locally. Satisfaction scores were obtained on the type, timing and correlation of information in the folder with free-text space available to provide further responses. No personal, identifiable data were collected as part of the survey.
Results
A 90% response rate was achieved with 27 patients completing the online questionnaire. Twenty were female, 7 male and the median age was 59 years (range 35-76 years).
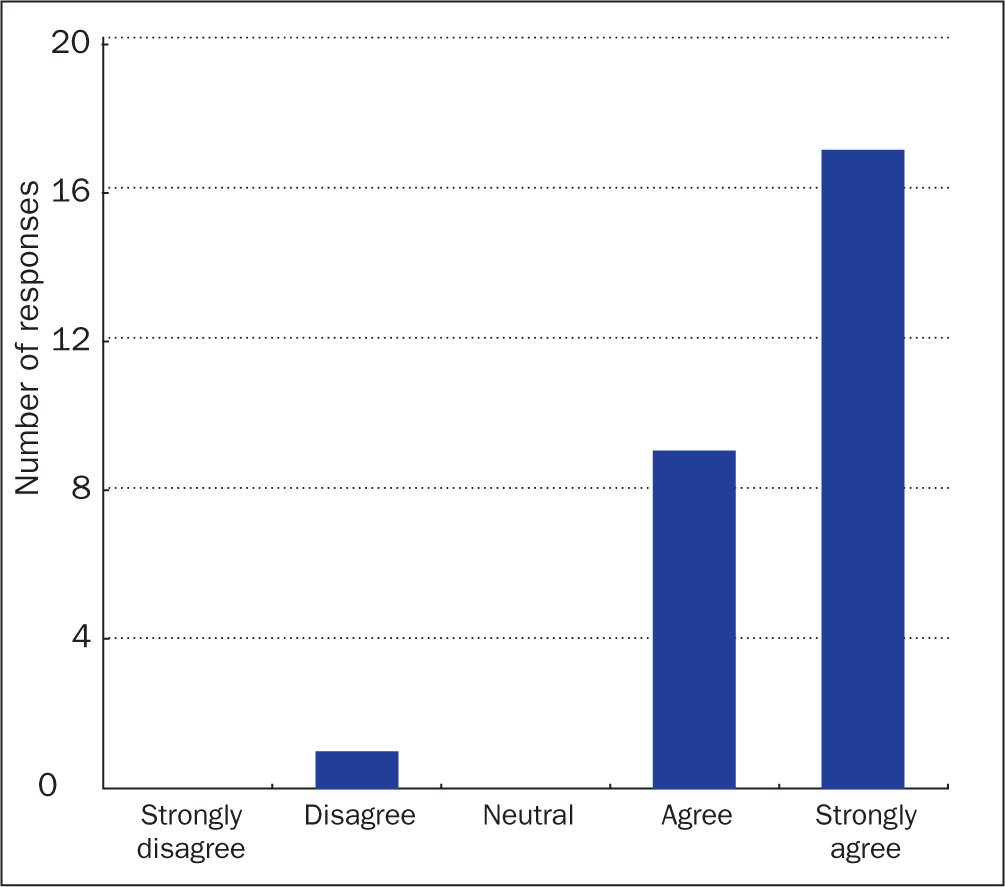
Did you find the treatment folder useful?
Of the respondents, 96% reported that they found the treatment folder useful, with 17 patients (67%) marking that they strongly agreed, 9 (29%) agreed and 1 (4%) disagreed (Figure 1).
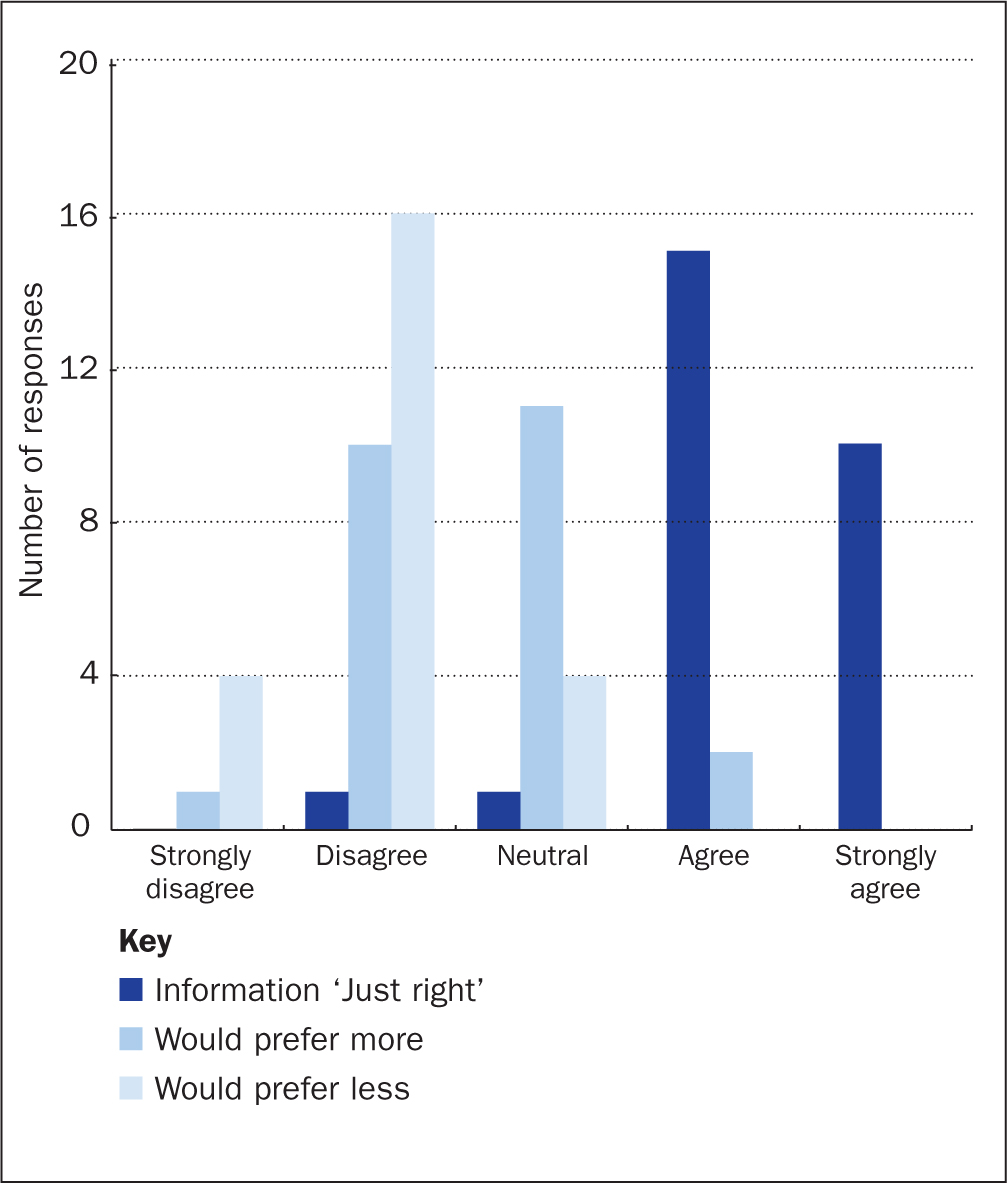
Was the amount of information provided adequate?
Participants were asked to respond to statements about the content of the folder to assess whether this was deemed to be appropriate. Twenty-five (92%) patients strongly agreed or agreed that the amount of information included in the folder was just right, with 2 (8%) patients indicating that they would have preferred more information and none indicating that less information would be preferable (Figure 2).
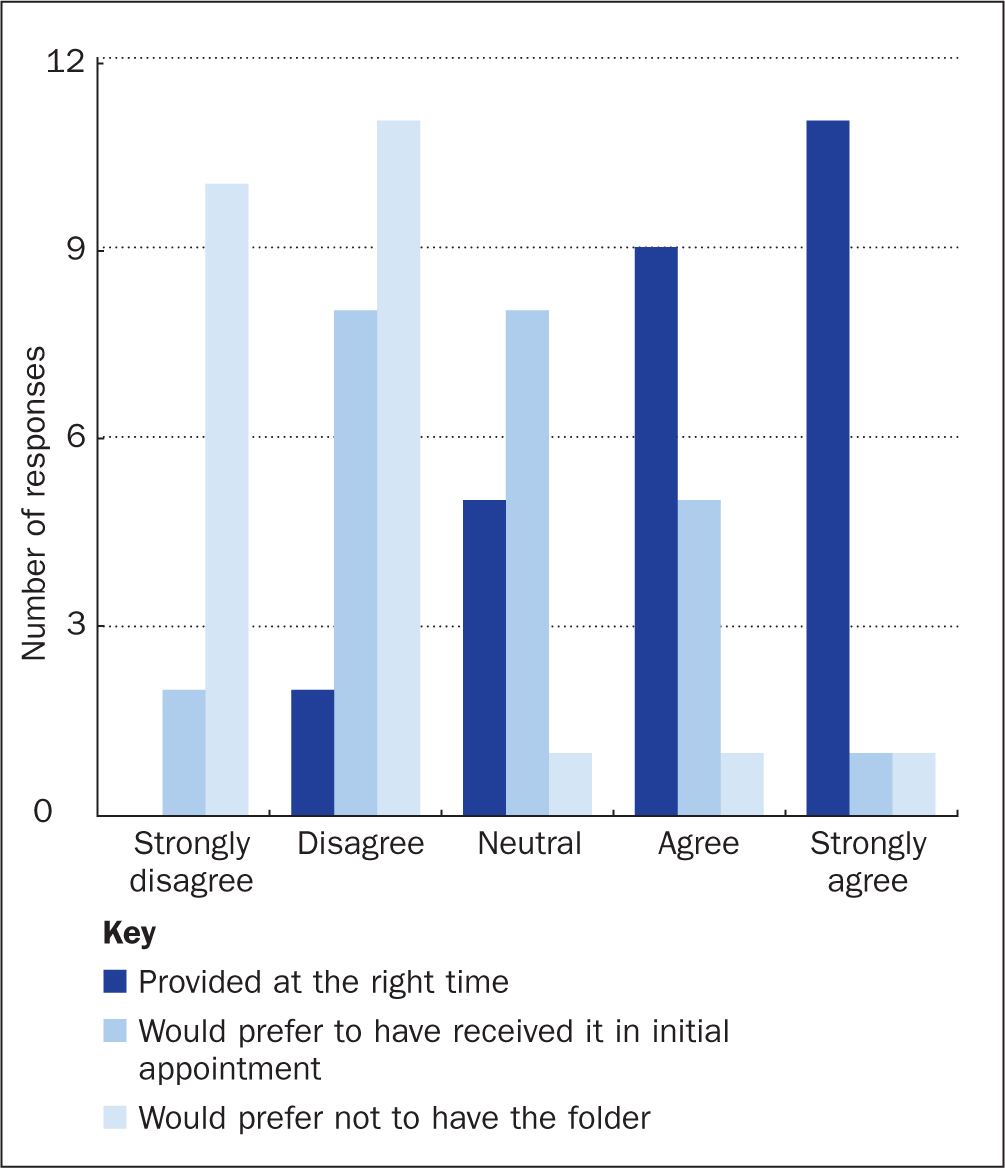
Was the folder introduced at the right time of the patient pathway?
The provision of the treatment folder was deemed to be at the right time in the patient pathway by the majority of the patients, with 20 (74%) agreeing or strongly agreeing, 5 (18%) being neutral and 2 (8%) disagreeing. Two patients (8%) would have preferred not to have received the folder at all and 6 (22%) indicated that they would have liked to have received the treatment folder in the initial outpatient appointment. However, 10 patients (37%) did not want to be given the folder at the initial outpatient appointment with 8 (30%) giving a neutral response to the question asked. Two patients indicated that they would have preferred not to have been given the folder at all (Figure 3).
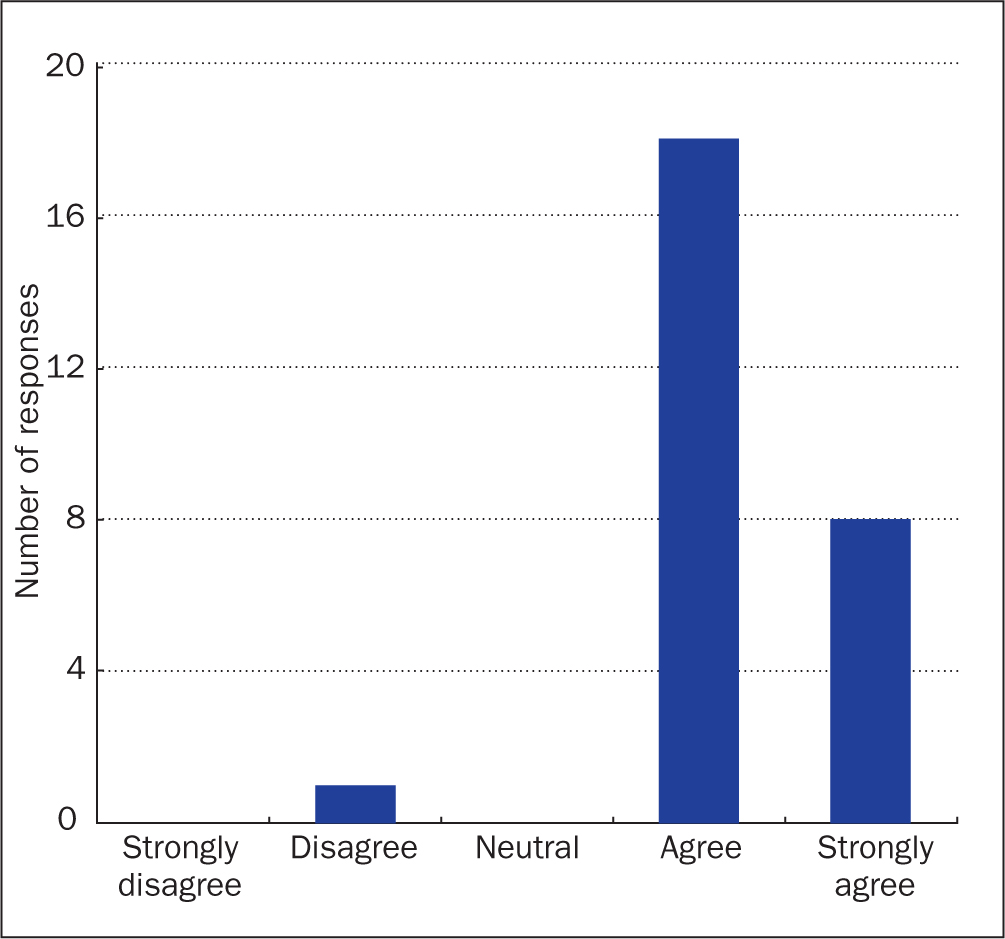
Was the content of the folder as expected?
Patients were asked to review whether the content of the information included in the treatment folder was as expected. Twenty-six (96%) responses indicated that the content met the expectations of patients (Figure 4).
Free-text comments
Participants were asked to provide free-text comments to enhance their responses to the questions asked and to provide an opportunity to give more information.
Free-text responses identified that one of the patients who indicated that they did not find the folder to be helpful had purchased a similar folder before treatment and therefore preferred to add specific information to that, rather than having a second folder given to them.
Other comments included:
‘After being discharged from Basingstoke I became unwell with pneumonia and ended up in [a hospital in a different part of the country]. I took the folder with me which proved very useful as the doctor at [the hospital] could quickly see my operation and discharge notes which helped me to get the correct treatment in [that hospital].’
‘I think it's useful to get the folder after surgery and before leaving hospital as the information was all relevant for my personal journey. Now I'm home it's great having everything in one place and knowing where that place is.’
Discussion
A cancer diagnosis and subsequent treatment are known to be a stressful experience that has a significant impact on an individual, leaving them vulnerable to long-lasting negative psychological outcomes and an impaired quality of life (Linden et al, 2012). There are many stress factors identified in the cancer care patient pathway, with potential traumatic events from the point of diagnosis, through to treatment and into the recovery and follow-up phase (Molina et al, 2014). The potential impact of a cancer diagnosis on patients cannot be underestimated and has been shown to increase the suicide risk in individuals diagnosed with cancer (Henson et al, 2019). Henson et al identified the first 6 months following diagnosis to be a critical period, but also that there was a sustained increased risk of suicide for the subsequent 3 years. This is attributed to unmet and unrecognised support needs during a stressful period. Furthermore, it demonstrates the importance of identifying these healthcare needs of cancer patients and implementing initiatives that are specifically designed to address them. The importance of acknowledging the impact of a cancer diagnosis and recognising the specific needs of patients was highlighted by the Independent Cancer Taskforce report (2015). The report recommended that the recognition and treatment of depression and anxiety related to a cancer diagnosis and treatment could improve adherence to treatment and thus improve overall outcomes.
Patients who are diagnosed with peritoneal malignancy have a complex pathway, with input from numerous professionals from multiple healthcare providers (local hospital, tertiary referral centres, GPs etc) involved in their care. The results of the patient survey clearly identified unmet healthcare needs, with the transition between inpatient care in our specialist unit to care within their local healthcare teams on discharge being a point of enhanced concern. More specific details regarding patients with rare malignancies were highlighted by De Heus et al (2021) who discussed in their systematic review how patients experience multiple and significant unmet needs throughout their disease pathway. These unmet needs are mostly reported in the information domain on the perceived adequacy of the information given and received. This is exacerbated in patients with a rare cancer, who are often cared for by teams based in different healthcare providers. This review of evidence highlights the importance of providing information to patients that is relevant to their care and is personalised to them.
The treatment of peritoneal malignancy in an experienced centre has been shown to improve outcomes of patients undergoing CRS and HIPEC (Moran et al, 2015). Patients diagnosed with this condition are therefore treated at centres that are often at a distance from their home in order to receive expert care. The expertise of a dedicated multidisciplinary team at such centres improves outcomes and reduces complications (Mittal et al, 2017). The specialist clinical teams are best placed to support patients undergoing CRS and HIPEC and have a responsibility to ease the transfer of care between local and specialist teams, and to ensure adequate support and information is provided at every step of the patient pathway.
All patients with a cancer diagnosis should have access to a follow-up pathway and support that is personalised to their needs (NHS England/NHS Improvement, 2019). The design and implementation of the treatment folder provides patients with personalised, comprehensive information at the point of discharge and aims to provide support in the period of transition, which has been highlighted as a time of increased anxiety. The results of the study demonstrate that the treatment folder is a welcomed resource with 95% of respondents reporting it to be useful.
The one patient who said they did not find the treatment folder useful added in the free-text section of the questionnaire that they had already purchased a similar folder at the point of diagnosis and therefore preferred to use the one they already had for compiling information and letters (they also had an online folder for digital information). It may have been a limitation of the way the survey was worded – if a respondent took the questions and statements literally as referring to the folder rather than the contents (ie a response being intended as ‘I had no use for the folder/container’, rather than reflecting the usefulness or not of information provided). The free-text comments further indicated that although the respondent did not personally find it useful, they liked the concept and felt that it was ‘definitely worth developing’.
The second patient who answered that they would have preferred not to have received the folder answered all the other questions in a very positive way and commented in the text that they thought it was an excellent idea and very helpful, so the team considered that this might have been a ‘misclick’ rather than a true response – a learning point for the future.
The provision of personalised information is a key aspect of meeting the needs of the individual and is recommended in the care of patients with a cancer diagnosis. Macmillan (2023) provides guidance on the practical implementation of personalised support to help people living with cancer to take an active and empowered role in their care. The charity advises that personalised care can be achieved through a series of supported conversations with the patient and by ensuring they are provided with adequate and appropriate information. The implementation of treatment summaries, as outlined by the National Cancer Survivorship Initiative (2013), is recommended to provide patients with specific information on their cancer diagnosis, treatment, follow-up care and indications of when to access healthcare advice. This information should be provided at the end of treatment, when evidence shows that many patients have unmet needs (Armes et al, 2009).
The timing of the treatment folder being given to patients was included in the study and 70% of respondents felt that the folder was provided at the right time in the care pathway. Further information gleaned from the free-text comments demonstrated that the folder helped support the information that is discussed verbally between the CNS and patient during the conversations that take place prior to discharge. It is this conversation that enables the folder to be truly personalised to the patient, as the discussions identify specific needs of the individual and should be considered a vital component of patient care. However, personalised care cannot be fully determined from a single conversation and it is imperative that patients are allocated a key worker early on in their treatment pathway to enable a relationship to be established between the patient and the CNS. The importance of this relationship should not be underestimated to enable open discussions to take place on potentially sensitive subjects.
Much has been written regarding the role of the CNS in relation to the care of the cancer patient, but Staunton (2020) looked closely at the role of the CNS specifically for patients with pseudomyxoma peritonei and identified the complexity of the requirements of patients with this rare disease. These needs are varied and cover a broad range of subjects but, in addition to the provision of expert advice, clinical consultancy and education, it focuses on the CNS's role in the personalisation of patient-centred care. That such a broad spectrum of expertise is required further supports the implementation of personalised care for patients undergoing CRS and HIPEC in a specialist centre.
For care to be personalised effectively the content of the information provided needs to be relevant to the individual receiving it. From a service perspective, there is generic information that should be provided to all patients, such as copies of clinic letters, operation letters and guidance on recovery from surgery in the first 6 weeks following discharge, but all other information included in the treatment folder should be personalised to the patient and their specific needs. When asked about whether the content of the folder was as expected, 98% of respondents indicated that it was and 92% felt that the volume of information included was ‘just right’. These results indicate that the design of the folder and its contents meet the needs of the patients in the provision of information relating to their disease and treatment.
Conclusion
Patients who are referred to the institute discussed here and treated with CRS and HIPEC have been diagnosed with a rare malignancy, and they have specific needs related to their diagnosis and treatment. The results of the annual patient survey clearly identified the importance of supportive, personalised care for patients undergoing treatment for peritoneal malignancy. A particularly vulnerable point in the care pathway is at discharge/transition of the patient's care from the specialist centre back to the local healthcare teams. The implementation of the treatment information folder at this point in the pathway has been well received and has been demonstrated to be a useful addition to the care previously in place.
Provision of information, guidance and support, in a manner that is clear, comprehensive and concise, can alleviate the anxiety of patients and enhance confidence on discharge. Ensuring written information is provided to support vital conversations between patient and CNS helps the patient to make sense of their treatment journey and identifying any unmet information needs. Personalised information is a key part of patient-centred care. Further development of the treatment folder would be beneficial to ensure that it continues to meet the needs of the patient, as would consideration of whether the treatment folder should be provided earlier in the pathway and examination of whether further additions would be useful to patients.
KEY POINTS
- Complex cancer care should be personalised to all patients undergoing treatment
- Unmet needs of complex cancer patients have long-term impact on their wellbeing
- To increase confidence on discharge, treatment folders (end-of-treatment summary and additional information) were personalised and provided to patients
- Almost all participants deemed the treatment folder to be helpful
- Further development of the treatment folder is needed to ensure patient care is optimised.
CPD reflective questions
- Reflecting on your own practice, how can you personalise patient care?
- How does the personalisation of care link to the Nursing and Midwifery Council's Code?
- Consider how healthcare teams find a balance between providing standardised information and tailoring information to patients' needs? What issues need to be addressed?


