Most people will be aware that, unfortunately, COVID-19 has led to more than 4 million deaths across the world. However, few are aware that more than 7 million premature deaths are caused by air pollution every single year (World Health Organization (WHO), 2021). Our grandparents may remember the deadly pea-souper smogs of the 1950s. And anyone who grew up in south or south east Asia will be familiar with the euphemistically named ‘haze’ events, where smoke from agricultural or forest burning blots out the sun and stings eyes and throats for days on end. However, in the UK, air pollution is largely invisible, but that does not mean that it does not affect our health.
Levels of air pollution can vary from day to day and throughout the year, depending on the weather and activities. Episodes of high air pollution can occur during winter months when weather conditions can mean that pollutants are trapped close to their sources, preventing them from being dispersed. In the summer, hot and sunny days can cause high levels of ozone. These episodes can cause an increase in hospital admissions for cardiovascular and respiratory effects.
Exposure to high levels of air pollution can affect us immediately, but even the seemingly low levels that we are exposed to every day can, over the longer term, damage our lungs, brains and cardiovascular systems. From adverse birth outcomes such as low birth weight to diabetes, cognitive decline and dementia, health effects can occur throughout our lives, reducing quality of life and life expectancy. Figure 1 details how air pollution affects people across the life course.
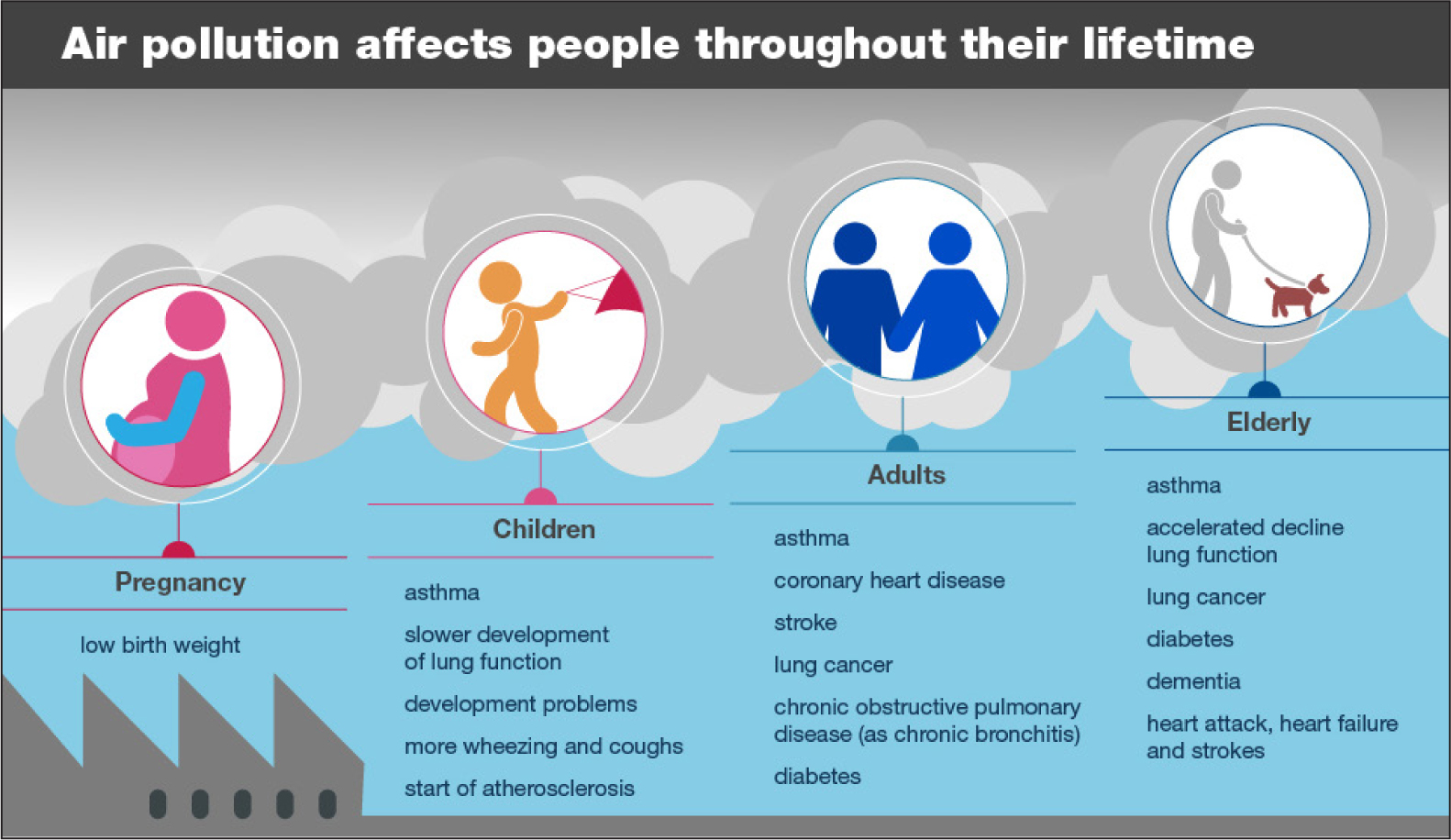 Figure 1. How air pollution affects people through life
Figure 1. How air pollution affects people through life
Some people are at higher risk from the effects of air pollution, including those with pre-existing cardiovascular or respiratory disease, as well as children, pregnant women and older people. People living or working in areas with high levels of air pollution, such as areas close to busy roads and in low-income communities, are also more likely to be affected by air pollution (Public Health England (PHE), 2019).
Air pollution is a complex mix of particles and gases that can occur naturally, such as from wind-blown soil and wildfires, or derive from human activities, emitted from transport, industry, agriculture, and domestic heating. Most of our evidence on the health effects is from exposure to particulate matter, a mixture of solid and liquid particles. Other pollutants include nitrogen dioxide, ozone, ammonia, sulphur dioxide, carbon monoxide and volatile organic compounds.
Given that we spend so much time indoors, we must not forget that the quality of indoor air is also important. Sources of indoor air pollutants include gas cookers, stoves (such as wood burners), fireplaces, building and construction materials. Furnishings and household consumer products can also include air pollutants, such as paints, cleaning products and air fresheners. Tobacco smoke is another household pollutant, with second-hand smoke a problem for non-smokers. Housing conditions are also an important factor: poor ventilation, lack of maintenance, damp and poorly maintained fuel-burning appliances can all reduce the quality of the indoor air.
Enhancing knowledge
To support all health and care professionals to enhance their knowledge and, more importantly, to take greater action on key public health issues, PHE has published free online e-learning resources as part of a programme entitled ‘All Our Health’ (PHE, 2019). Already being accessed by thousands of health and care professionals, the air pollution e-learning resource aims to support professionals by:
- Enhancing knowledge of air pollution and increasing confidence on discussing it
- Increasing understanding of health inequalities related to air pollution and what actions can be taken to address this in your setting
- Helping you to think about the data, resources and services available in your area that can help address or manage air pollution.
This year, for the first time in the UK, a coroner recorded that air pollution contributed to the death of Ella Kissi Debrah, a 9-year-old who had severe asthma. The coroner's report highlighted that there was:
‘Low public awareness of the sources of information about national and local pollution levels and that greater awareness would help individuals reduce their personal exposure to air pollution.’
Courts and Tribunals Judiciary, 2021
Information about daily levels of air pollution can be found on the Department for Environment, Food and Rural Affairs' UK Air website, which features a Daily Air Quality Index (DAQI) (https://uk-air.defra.gov.uk/air-pollution/daqi). This provides recommended actions and health advice for both the general population and for at-risk individuals. The index is numbered 1 to 10 and divided into 4 bands, low (1) to very high (10). You can find it on apps including the Met Office weather app. The Clean Air Hub also provides information for the public and health and care professionals about the health effects of air pollution and actions they can take (https://www.cleanairhub.org.uk/).
The coroner's report also noted that the adverse effects of air pollution on health are not being sufficiently communicated to patients and their carers by medical and nursing professionals. Health and care professionals are invaluable as a trusted source in helping to provide advice to the public about how air pollution can affect their health, and how to help reduce their exposure. The National Institute of Health and Care Excellence (NICE) recommends that children, young people and adults with chronic respiratory or cardiovascular conditions are given advice at routine health appointments on what to do when outdoor air quality is poor. NICE has also produced guidance on both outdoor air quality and indoor air quality at home (NICE 2017, 2019, 2020).
Building back better, fairer and greener
As we start to focus on the recovery phase of the COVID-19 pandemic, it will be essential for the nursing and midwifery workforces to appraise the lessons learnt and consider what changes need to be made to ensure that we genuinely build back better and fairer. This will require the professions to use the 2020s as a decade that sees transformation across the nursing and midwifery workforces, placing equal focus on both preventing diseases as we do on treating them. Given the significant impact that air pollution plays in causing preventable ill health and premature death, nurses must prioritise this area of practice and take every opportunity to address unacceptable health inequalities.
It is not just about giving advice to the public but recognising that we can all do our bit to help spread the word about improving air quality and the actions which can be taken.
The NHS has set ambitious targets to reduce emissions, and with more than 1.3 million people employed by the NHS in England, much can be done to limit the impact on the environment and make a difference to public health (Greener NHS website, 2021).
Nurses can act as a force for change in supporting healthy communities and challenging policy and practice for the greater good. As the largest and most trusted professional workforce, nurses have the potential to make change happen.
CASE STUDY
Donald Jones (not his real name) attended his local medical practice for his annual asthma review with his practice nurse, Caroline. During the consultation, the practice nurse found out that Donald was having to use his reliever inhaler more often. They went through his usual triggers for this, but could not identify anything unusual.
Caroline had completed the All Our Health e-learning resource on air pollution and had read the NICE guidance on outdoor air pollution and indoor air pollution, so she knew that air pollution might be causing his asthma attacks. She had developed a general understanding of the sources of both indoor and outdoor air pollution, how it can affect health and what advice she can give to her patients.
Caroline gave the usual advice around the management of asthma, but she also discussed air pollution as part of Donald's personalised asthma action plan. She advised Donald that outdoor air pollution or pollutants in the home can sometimes be a trigger for asthma attacks. She also explained that some pollution particles are very small or are gases and can reach down into the lungs and irritate the airways.
Caroline also knew that air pollution has been high in their area recently because she regularly checks the Daily Air Quality Index. She asked whether Donald lived or worked near busy roads. Donald explained that he regularly walked to work along a busy road. Caroline explained that it was good to keep exercising but taking an alternative route away from the heavy traffic might help. She suggested that Donald looked at the Daily Air Quality Index, when the index showed ‘high’ levels of air pollution he should reduce strenuous physical exertion, particularly outdoors, and particularly if he was experiencing symptoms.
Caroline asked about Donald's home and whether there was any damp or mould. Activities such as drying wet clothes indoors without adequate ventilation can cause a build-up of damp and mould. She also mentioned how chemicals from cleaning sprays and air fresheners can trigger asthma attacks in some people and advised not to use them or to use a non-spray alternative.
Together they updated Donald's personal asthma action plan to include air pollution as a trigger and actions to help reduce exposure. Caroline recommended that Donald also look at webpages on air pollution and asthma from Asthma UK (https://tinyurl.com/f9j2u3n8) and the British Lung Foundation (https://tinyurl.com/3cxfmtsb).
Donald went away from his asthma review knowing that there were positive things that he could do that might better help manage his asthma in the future.


