An intestinal stoma is a surgically created opening in the body that allow waste matter to bypass the digestive system and may be formed in patients with a range of underlying conditions, such as cancer and inflammatory bowel disease (IBD) (Burch, 2005; Hill, 2020). In the UK, it is estimated that between 176000 and 205000 people live with a stoma (Aibibula et al, 2022; Burch, 2022). Around 13500 people undergo stoma surgery each year (Kettle, 2019): 56% of stomas are permanent and 44% are classified as temporary or reversible (Eucomed Medical Technology, 2012). There are three main types of functional ostomies: colostomy (the most common, accounting for 43–54% of stomas), ileostomy (about 38%) and urostomy (10-18%) (Burch, 2014).
Stoma formation can be lifesaving (Burch, 2005), but it can pose considerable challenges (Claessens et al, 2015; Jeppesen et al, 2022; Martins et al, 2022a). The creation of the stoma can cause significant complications, although the number of people reporting problems in the literature varies between 20% and 70% (Krishnamurty et al, 2017). As well as surgical complications, long-term issues represent a significant burden on the patient and may be under-reported (Scheidbach et al, 2009; Murken and Bleier, 2019; Pearson et al, 2020).
Coloplast has developed a new digital leakage notification system, Heylo™, to address the unmet need associated with leakage and leakage worry for people living with an ileostomy or colostomy with liquid/mushy faecal output. Coloplast and the authors identified that there is currently no tool routinely used in clinical practice to assess this need and consequently developed a provisional assessment tool, which can be used with Heylo, and potentially other innovations and interventions, to help address leakage and leakage worry.
Literature review of leakage and complications
Stoma leakage
Leakage is a common problem for people living with a stoma. One study found that only 2.9 out of 10 baseplates were free of stoma effluent (Down et al, 2021), with many people experiencing leakage (Pearson et al, 2020). In the Ostomy Life Study, a large survey of more than 4000 people living with a stoma, about three-quarters (77%) of respondents reported experiencing output under the baseplate and one-quarter (26%) leakage onto clothes in the preceding month (Martins et al, 2022a). A published study with data from 3509 stoma surgeries evaluated surgical and patient-centred stomal complications after stoma formation with emphasis on under-reported symptoms and complaints. Night-time leakage, soiling, and emptying were high post–stoma formation, particularly in the ileostomy group, and continued to be reported as high after 2 years (Pearson et al, 2020).
There are two distinguishable types of leakage (Nafees et al, 2018):
- Leakage underneath the baseplate (LUB): output that stays underneath the baseplate in contact with the skin, but is not visible when wearing the stoma product
- Leakage outside the baseplate (LOB): output that seeps beyond the baseplate resulting in soiling of clothing or bedding (commonly referred to as leakage onto clothes)
Non-visible leakage (ie LUB) may go undetected and thus stay in contact with the skin for prolonged periods; visible output that extends beyond the baseplate (ie LOB) can have significant emotional and physical consequences (Nafees et al, 2018; Voegeli et al, 2020). The incidence of LUB and LOB is dependent on many factors including stoma type (Martins et al, 2022a). In a survey of 328 stoma care nurses (SCNs), the main reasons cited for leakage were stoma related (82%), the patient's peristomal body profile (72%), incorrect product usage (65%) or the patient not following recommendations (22%) (Down et al, 2021). Other factors include having an ileostomy, having a liquid faecal output, a stoma that was level with or below the skin level, and irregularities or superficial creases, stoma location, stoma mobility (peristalsis) or folds around the stoma (Almutairi et al, 2018; Martins et al, 2022a).
Worry about leakage and impact of leakage on quality of life
Leakage seems to be most prevalent just after stoma formation and within the first year following surgery (Jeppesen et al, 2022); for some people, it can remain a persistent problem (Pearson et al, 2020; Jeppesen et al, 2022; Martins et al, 2022a; Osborne et al, 2022). It can lead to problems such as soiling, skin complications and sleep disturbance due to having to check or empty the bag (Pearson et al, 2020). For many people with a stoma, worry about leakage can be a constant mental burden Claessens et al, 2015; Jeppesen et al, 2022).
Leakage has been shown to impact the physical, psychological and social wellbeing of people living with a stoma (Jeppesen et al, 2022) and, in some cases, post-surgery anxiety can lead to a person isolating themselves from social situations (Claessens et al, 2015; Jeppesen et al, 2022). The possibility of unpleasant odour and noise means that individuals with a stoma may face additional unique social anxieties following surgery. A systematic literature review of 14 descriptive cross-sectional studies demonstrated that living with a colostomy negatively influences overall quality of life (QoL) (Vonk-Klaassen et al, 2016). The stoma-related problems described included sexual problems, depressive feelings, gas/flatus, constipation, dissatisfaction with appearance, change in clothing, travel difficulties, feeling tired, and worry about noises and odour (Mitchell et al, 2007; Popek et al, 2010; Paszyńska et al, 2023).
In a matched cross-sectional study of long-term rectal cancer survivors, both men and women living with a stoma had significantly worse social wellbeing compared to those who did not require an ostomy (Krouse et al, 2009). The psychological impact of leakage was investigated in three large Ostomy Life Studies, where worrying about leakage was reported from a low to a very high degree by 90–92% of respondents (Claessens et al, 2015; Hedegaard et al, 2020; Jeppesen et al, 2022). ‘High’ and ‘very high’ levels of leakage worry were reported by 23% and 26% of respondents within 1 year of stoma surgery respectively, and in 22% and 27% of those with a liquid output (Jeppesen et al, 2022).
The most recent Ostomy Life Study 2019 showed that worrying about leakage had a direct impact on an individual's behaviour, with 20% of respondents choosing to stay at home due to leakage; 63% felt they were in control, with 74% indicating that they were able to cope; 39% reported that they often or always kept checking their ostomy solution for potential leakage; 15% avoided physical contact (respondents selected the answer ‘often’ or ‘all of the time’ to the question about worry regarding leakage) (Jeppesen et al, 2022). Furthermore, the study showed that, among those who were in employment, 65% reported that their ability to be effective at work was affected by leakage to a greater or lesser degree, compared with those who worried less; 15% of those who worried about leakage reported that their ability to be effective at work was highly affected (Jeppesen et al, 2022). Worry and fear about leakage can significantly affect a patient's QoL.
Leakage and worry about leakage do not only affect psychosocial wellbeing, but also influence people's use of stoma care products. The Ostomy Life Study 2019 (Jeppesen et al, 2022) found that 54% of people with a stoma used more ostomy products (bags and baseplates) than those who worried less and 52% used supporting products (such as pastes, tapes and belts) to manage leakage and leakage worry. Those who worried about leakage to a high or very high degree reported using more rings/seals, tapes, belts and/or powders than the remaining population of people with a stoma, and worry of leakage made 23% of patients contact their SCN for advice (Jeppesen et al, 2022).
Leakage and peristomal skin complications
Leakage is significantly correlated with issues such as peristomal skin complications (PSCs) (Nybæk et al, 2009; Porrett et al, 2011). However, there is wide variation in PSC prevalence, with reports ranging from 18% to 88% in individuals living with a stoma (Herlufsen et al, 2006; Richbourg et al, 2007; Gray et al, 2013; Salvadalena, 2013; Colwell et al, 2017; Fellows et al, 2021). PSCs can compromise the ability of the baseplate to stick to the skin, further increasing the risk of (recurrent) leakage incidents (Nybaek et al, 2009). They are also associated with erythema, sore/irritated skin, pain, itching and burning sensations, which all have a significant negative impact on people living with a stoma. Repeated incidents of leakage can lead to a breakdown of the skin around the stoma (Gray et al, 2013; Voegeli et al, 2020; Fellows et al, 2021), which affects QoL (Goldstine et al, 2019; Nichols et al, 2019; Hedegaard et al, 2020).
Health economic impact of leakage and leakage worry
As well as the often considerable physical and psychological impact on the patient, stoma care and its complications place a significant burden on the NHS and healthcare resources. An estimated £364 million per year is spent on stoma products in the UK, with an average cost per patient per year in the region of £2008, although some patients may have more complex requirements (Kettle, 2019). In addition to the cost of the products, specialist SCNs are an essential part of patient care in both acute and community settings (Bird et al, 2023). Leakage and its consequences are common reasons for patients to seek additional support (Down et al, 2021), with 35% of in-person nurse consultations concerning leakage and its complications, and a further 17% related to emotional issues (Vestergaard et al, 2023). In the Ostomy Life 2019 study, 96% of SCNs (Down et al, 2021) reported that two or more patient consultations were needed to resolve a leakage issue, and in 28% of cases four or more consultations were required.
A study to quantify the impact of leakage on healthcare utilisation found that 21.4% of those who had experienced leakage in the preceding 3 months had been in contact with a health professional; 39.6% had increased the frequency with which they changed their ostomy product; 25.0% had increased their use of existing supporting products; and 21.1% had added additional supporting products to their routine (NB The study was conducted with participants from the UK, Germany, France, the USA and Denmark) (de Fries Jensen et al, 2023). PSCs also result in increased healthcare costs (Persson et al, 2005; Pittman et al, 2008; Neil et al, 2016; Rolls et al, 2023). In one study from Denmark, they accounted for 39% (n=181/464) of all consultations with ostomy nurses (Jemec and Nybæk, 2008). Moreover, consumption of ostomy products and supporting products also increased when people experienced PSCs (Neil et al, 2016; Voegeli et al, 2020).
Literature review summary
From the data presented, it is clear that leakage and its consequences impact patients' overall QoL and wellbeing. They place a large burden on SCNs, as well as affect the use of products, thereby incurring significant costs for the NHS. The data suggest potentially significant effects in terms of skin complications, emotional issues, isolation, anxiety/depression, disrupted sleep, and work and social life (Bassy and Libutzki, 2019; Jeppesen et al, 2022). Worry about leakage is clearly a significant problem for many people living with a stoma (Jeppesen et al, 2022; Brady et al, 2023a; de Fries Jensen et al, 2023). So how can health professionals identify those at greatest risk in order to help to improve their QoL?
Identifying patients who worry about leakage
Tools to assess stoma-related complications
Ideally, a standardised and validated tool would be used to identify patients who struggle physically or mentally with leakage and its consequences. Tools and assessments used in routine clinical practice should be validated, relevant and reliable, as well as simple and easy to use in terms of length (ie the number of questions) and design (patient or health professional led). Assessments used in clinical practice should provide an overview of an individual patient's stoma care and guidance on decision-making, with the opportunity to explore and understand a patient's specific challenges and needs.
There are several available tools and instruments to assess the individual needs of people living with a stoma; however, each has its strengths and weaknesses. Some have been developed specifically for use in people with stomas, such as the Ostomy Leakage Impact (OLI) tool (Nafees et al, 2018) and the Ostomy Skin Tool 2.0 (Martins et al, 2022b; Jemec et al, 2023), whereas others are generic and may not capture the precise needs of individuals living with a stoma and the challenges they experience. Examples of generic tools include the 5-item World Health Organization Well-Being Index (WHO-5) (Topp et al, 2015) and the Short Form (36) Health Survey (SF-36) (Brazier et al, 1992). Some tools capture only certain elements of living with a stoma, such as the Body Profile Assessment (BPA), which evaluates the peristomal area (Vendelbo et al, 2023), whereas others are too long for use in routine clinical practice, namely the 43-item City of Hope Quality of Life Ostomy Questionnaire (Grant et al, 2004). In terms of tools developed specially to understand the impact of leakage on people using a stoma appliance, the OLI is a validated patient-reported tool comprising 22 questions across three domains: emotional impact (including sleep), usual and social activities, and coping and control (Nafees et al, 2018).
The OLI tool is a validated, patient-reported instrument that captures the impact of leakage. However, although it is a useful tool that health professional can apply to assess a patient's quality of life, the authors recognised that it was too long to be routinely implemented. Therefore, the authors wished to develop a user-friendly tool for clinical practice to assess the impact of leakage, which would also help identify people who would benefit from the use of a digital leakage notification system.
Development of the leakage impact assessment form
The first stage of development established which of the factors identified in the literature are the most important in clinical practice, such as coping strategies, social support, tendency to worry, leakage anxiety, or not returning to work or normal life after surgery. The second stage in the development process was setting up and running a series of three consensus groups and qualitative workshops with 26 specialist SCNs to evaluate and refine a list of questions to include in the form.
The two rounds of development created an initial version of the Leakage Impact Assessment tool, which was then reviewed by the authors. There was then a final round of meetings with the original groups of SCNs to gain consensus, to ensure that the questioning, scoring and framing of the questions were appropriate and clinically relevant. The authors provided a final round of review and input to the development of the form, the phrasing of the statements and reviewing the overall structure.
Using the leakage impact assessment form
The provisional tool (Figure 1) begins with a statement to establish the degree of worry the patient has about leakage, followed by eight statements that have been identified as the most important in relation to non-surgical complications and ongoing stoma management in the context of leakage impact; these eight statements are also representative of the three domains from the OLI. In addition, the final section of the tool includes questions on type of output, access to a smartphone and episodes of leakage over the preceding 2 weeks: these issues are relevant for evaluating the appropriateness of an intervention such as the digital leakage notification system (Heylo), or any other interventions to address leakage and leakage worry that may become available to patients in future.
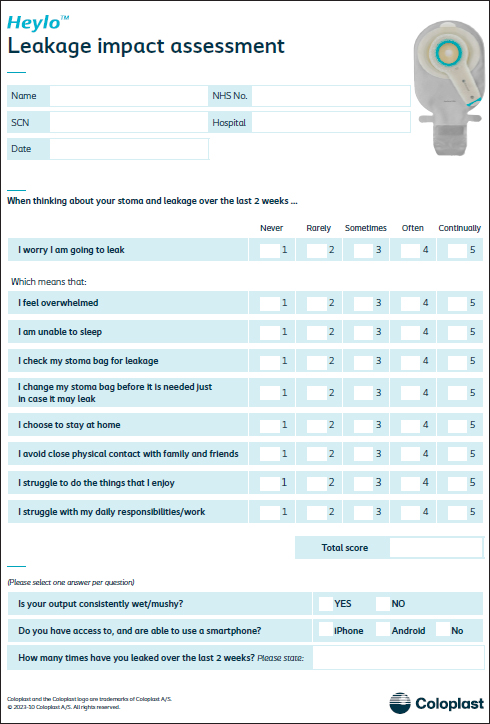
The leakage impact assessment form can be completed by patients prior to their consultation or as part of the nursing assessment. There is uncertainty around the optimal timing of assessment post surgery, because the impact of leakage may not be immediate; however, a pattern of low/moderate/high impact may still be observable to guide assessment.
Although formal validation of the scoring still needs to be undertaken, the total score represents the overall level of leakage worry, while the individual scores characterise the impact on a patient's everyday life. Interpretation should include the overall pattern of scores, with specific scores pointing to level of need, for example:
- High scores indicate that the patient is strongly impacted by worry of leakage, demonstrated by scoring 4 or 5 on the majority of questions
- Mid-value scores suggest that the person is experiencing a moderate impact on their QoL due to worry about leakage, especially if they score 3 on most of the statements, but with some statements scoring 2 or 4
- Low scores indicate that the impact of worry is low, as demonstrated by the majority of statements scoring 1 and 2.
The total score is intended for ease of reference during a review and to monitor changes in scores at subsequent reviews. It is not intended as a threshold for decision-making because neither the appropriate categories nor the issues that inform them have yet been established. Interpretation of the scoring is intended as a guide to be considered as part of a wider assessment of the patient, with moderate to high scores indicating those who are most likely to have the biggest benefit from using Heylo. The assessment tool is currently termed ‘provisional’ since it needs to undergo formal validation and more experience needs to be accumulated through its application in the clinical setting, with subsequent iterations developed as needed.
Tackling unmet needs
Although some products have been developed to help individuals manage their stoma better, complications are still prevalent, which means that patients continue to experience significant worry and distress, leading to decreased QoL, increased healthcare resource utilisation and excessive product use (Jeppesen et al, 2022; de Fries Jensen et al, 2023, Rolls et al, 2023). People living with a stoma cannot always feel a leakage occurring underneath their baseplate and a leakage event is unpredictable to many patients. Only when the faecal output reaches the outside of the baseplate and soils clothes do patients become aware of it (as identified via anecdotal evidence from personal communications with the authors) – and it is clear that such leakage events may represent trauma for people living with a stoma (Jeppesen et al, 2022).
Advances in products and patient care have helped to improve the fit and attachment of the baseplate to the body, but there is still a profound unmet clinical need to detect leakage as early as possible to ensure a timely change of the baseplate, reduce exposure of peristomal skin to faecal output, and reduce the risk of LOB (on to clothes). Earlier detection of leakage could help reduce its impact and enable people with a stoma to become confident in their stoma management, reducing worry about leakage and improving psychological wellbeing.
In recognition of this unmet need, a digital leakage notification system has been developed to detect and notify people living with a stoma of the occurrence of LUB via an app on their smartphone. The Heylo leakage notification system is a first-of-its-kind digital solution for patients with a stoma and represents a new category in ostomy care. The system is designed to be easy to use and works with both iOS and Android smartphones, together with most ostomy solutions on the market.
The Heylo leakage notification system comprises:
- The app: tracks leakages and sends notifications to the user's smartphone (the user can also check for leakage at any time)
- The sensor layer: continuously monitors for leakage to detect output before it reaches the edge of the baseplate
- The transmitter: a reusable component that physically connects the sensor layer to the user's smartphone via bluetooth
- The charging dock: to wirelessly charge the transmitter.
Leakage is one of the biggest problems for people living with a stoma (Claessens et al, 2015; Aibibula et al, 2022), therefore Heylo should help them manage the physical and mental burden this brings. Giving patients the ability to be in control of leakage enables them to perform ostomy product changes according to the actual status of the baseplate, rather than being guided by their fear of leakage and having to act preventively (Brady et al, 2023a). It is hoped that use of Heylo will allow patients to take part in everyday life with more dignity and confidence, and may also reduce product usage by increasing length of wear time.
The Heylo leakage notification system has undergone an extensive clinical developmental programme, which has demonstrated its reliability and accuracy for detecting leakage in addition to reducing leakage worry (Brady et al, 2023a; 2023b). Heylo has been evaluated by both people living with a stoma and SCNs, who recognised the value of the product in reducing worry about leakage.
In a prospective, single-arm pilot study with 25 people experienced in living with a stoma with leakage issues, the mean number of LOB episodes decreased significantly from 2.84 in the 3 weeks before the trial to 0.51 leakage episodes with Heylo over the 3-week test period (P<0.001); feedback from patients also showed that there was a significant reduction in worry about leakage (P<0.001) (Brady et al, 2023a). In a multicentre, open label, single-arm study involving 92 patients with a recent (≤9 months) stoma formation, the mean number of episodes of LOB decreased from an average of 1.57 (95% CI [1.19; 2.08]) during the preceding 14 days to an average of 0.93 (95% CI [0.56; 1.54]) episodes during the 14-day test period, corresponding to a 41% reduction in episodes of leakage outside the baseplate (P=0.046) (Brady et al, 2023b). The study also showed a significant improvement in QoL documented through a significant increase in all three domains of the OLI (emotional impact P<0.001, usual and social activities P<0.001, coping and control P<0.001).
The benefits of Heylo on leakage reduction and improvements to QoL were later confirmed in a larger randomised, controlled, cross-over clinical trial (Ambe et al, 2023). Reducing the incidence of leakage on to clothes should significantly reduce the burden experienced by people living with a stoma and potentially reduce the healthcare resources spent on consultations with health professionals and on ostomy products (de Fries Jensen et al, 2023).
Heylo aims to help both new and experienced patients who struggle physically or mentally with leakage and its consequences. It is broadly suitable for adults and adolescents who have an ileostomy or a colostomy that produces liquid or mushy faecal output; however, in clinical practice, it should be offered on a patient-by-patient basis, depending on individual need and level of worry about leakage. These factors are reflected in the provisional leakage impact assessment tool.
The authors suggest that moderate to high scores on the leakage impact assessment tool are indicative of patients who would have the greatest benefit from the security that Heylo can bring. However, the information obtained using the leakage impact assessment tool should always be considered in combination with clinical assessment by the nurse.
Conclusion and next steps
Reviewing the published evidence demonstrates that leakage is a well-documented problem for people living with a stoma, which has a significant impact on their everyday lives. Fear and worry about leakage can severely limit a person's mental health, QoL and affects their daily activities (Jeppesen et al, 2022). It is also associated with PSCs and significant burden and cost to the NHS (Nybæk et al, 2009; Porrett et al, 2011; de Fries Jensen et al, 2023; Rolls et al, 2023). Identifying leakage early, before it extends beyond the baseplate, could help avoid worry associated with leakage and decrease costs due to reduced product usage, improved self-care and fewer consultations.
Along with identifying and selecting the most appropriate stoma products for each individual patient, the Heylo leakage notification system has been shown to detect leakage early reliably and accurately, which enables users to take action to avoid it progressing outside the baseplate (Brady et al, 2023a; 2023b); this has the potential to deliver significant improvements in patient care, as well as secondary benefits to the healthcare system.
By conducting several consensus meetings with expert SCNs, Coloplast Ltd and the authors developed the leakage impact assessment tool for use in clinical practice to support assessment and identification of patients who have been affected by worry about leakage, in terms of emotional impact (sleep, daily routine and social activities), and coping and control over life with their stoma. By establishing and adopting a proactive, preventive approach, SCNs can identify struggling patients and thus help them to manage their stoma, reduce the worry around leakage, and consequently improve their lives.
The next steps are to test the leakage impact assessment tool in clinical practice and to establish whether it is appropriate for identifying patients with leakage worry. In addition, the authors would like to investigate the scoring (total score versus pattern of responses) to further understand the tool's use in clinical practice. Finally, when Heylo becomes available in the UK at a future date, Coloplast Ltd and the authors propose to test the appropriateness of the tool for identifying patients suitable for Heylo and how interpretation of the scoring can inform clinical decision-making, as well as to monitor the impact of Heylo on leakage worry.
KEY POINTS
- People with a stoma face many challenges, including leakage of stomal effluent from under the baseplate and onto their clothes
- Leakage and worrying about it occurring can significantly impact patients' everyday lives and their quality of life
- A novel digital leakage notification system is able to detect and notify users of leakage occurrence under the baseplate
- A tool has been developed to identify patients who might benefit from use of the digital leakage notification system
CPD reflective questions
Reflect on the impact of stoma leakage on the person with a newly formed stoma:
- Why are the cost of stoma products relevant to health professionals?
- How would you identify and assess for worry associated with leakage in your patient group?
- Give three examples of how a validated tool related to worry associated with leakage can enhance patient care
- Consider whether tool assessments can be beneficial in improving patient care


