A stoma is a surgically created opening on the abdomen that involves bringing a spout of bowel to the surface to provide an outlet for urine or faeces from the body. Stoma formation can be a lifesaving intervention, performed primarily in the treatment of cancer, inflammatory bowel disease, trauma or other bowel or bladder diseases (Schott et al, 2022). The stoma can be temporary or permanent, and the surgery can be planned (elective) or unplanned (acute/emergency), depending on the cause for its creation (Pine et al, 2020; Schott et al, 2022).
Formation of a stoma is a significant event for patients and introduces multiple challenges to a patient's lifestyle and self-care, which requires both physical and psychological adjustments (Brown and Randle, 2005; Martins et al, 2022a). Early complications following stoma surgery are prevalent, such as stoma retraction, oedema, necrosis, stenosis and peristomal skin complications (PSCs) (Pearson et al, 2020; Maglio et al, 2021); these may prolong hospital stay, increase the risk of readmissions and increase the number of visits to outpatient clinics, resulting in larger costs related to stoma care (Zelga et al, 2021). Even several years post-surgery about 2 out of 3 people with a stoma continue to struggle with one or more self-care problem (Bulkley et al, 2018), such as leakage of stomal effluent outside the pouching system (bag and baseplate), PSCs and the amount of time needed each day for stoma care (Bulkley et al, 2018; Pearson et al, 2020). These can have a significant psychological impact, which will affect each individual differently (Goldstine et al, 2019; Nichols et al, 2019; Jeppesen et al, 2022; Rolls et al, 2022).
The type of stoma surgery performed, inadequate patient education and a lack of pre-operative stoma site marking are some of the contributing factors for the development of complications following stoma formation (Hsu et al, 2020; Zelga et al, 2021; Ambe et al, 2022; Schott et al, 2022). Stoma care nurses (SCNs) play an important role in helping patients to adapt to a new life following stoma surgery, for example early counselling and teaching of stoma-management can enhance the psychological adjustment to living with a stoma (O'Connor, 2005).
This study explored and quantified the successes, choices, and challenges faced by SCNs and patients having stoma surgery in the pre-operative phase, during hospital admission and after hospital discharge. The investigation includes perspectives from both patients and SCNs.
Methods
The Ostomy Life Study 2022 consisted of two online, retrospective, self-reported questionnaires developed by Coloplast A/S. One questionnaire was designed for people with a stoma and the other for nurses working within stoma care services. The questionnaires were sent out to the participants via email.
Patients
A total of 99 023 people with a stoma from 12 countries (Australia, Austria, Canada, Finland, France, Germany, Italy, Japan, the Netherlands, Switzerland, the UK and the USA) were invited to participate in the study in January and in May 2022. Participants were randomly selected from local Coloplast A/S databases.
The patient survey questionnaire elicited demographic information, such as participants' age, sex, years living with a stoma, type of stoma, as well as users' self-reported details about their stoma surgery, hospital stay, mental health and product choice. Every question had a set of predefined response options and some questions included the option ‘other reason’, coupled with the opportunity to provide a free-text answer.
The study mainly concerned the pre- and postoperative phases of stoma surgery. For simplicity, in presenting the results of the questionnaires, the article primarily refers to people living with a stoma as patients.
Nurses
Nurses from local Coloplast Ostomy Forum (COF) boards in 15 countries (Austria, Belgium, Canada, Czech Republic, Denmark, France, Germany, Italy, Japan, the Netherlands, Norway, Poland, Sweden, the UK and the USA) were invited to participate in the study between May and June 2022.
The nurse survey contained questions regarding work experience, time spent preparing patients for stoma surgery and for life living with a stoma, and product choice. Every question had a set of predefined response options and some questions included the option ‘other reason’, coupled with the opportunity to provide a free-text answer.
Statistics
Data were collected and processed using Microsoft Excel. The data have been presented with descriptive statistics.
Results
Participant demographics
Patient demographics
A total of 6500 people with a stoma from 12 countries completed the patient-specific survey (Australia, 6%; Austria, 1%; Canada, 7%; Finland, 3%; France, 11%; Germany, 14%; Italy, 6%; Japan, 10%; the Netherlands, 15%; Switzerland, 2%'; the UK, 13%; and the USA, 10%). Of these, 45% were female and most (86%) were aged 50 years or older. In total, 64% of participants were veterans (that is, those who had had their stoma for 5 years or more), 29% were experienced users (had had their stoma for 1–4 years) and 7% were new users (had had stoma surgery within the preceding year). In terms of stoma type, 47% had a colostomy, 36% had an ileostomy and 18% had a urostomy.
Nurse demographics
A total of 250 nurses from 15 countries completed the nurse-specific survey (Austria, 4%; Belgium, 13%; Canada, 5%; Czech Republic, 9%; Denmark, 4%; France, 6%; Germany, 6%; Italy, 11%; Japan, 6%; the Netherlands, 2%; Norway, 2%; Poland, 19%; Sweden, 4%; the UK, 4%; and the USA, 4%).
The responses from the nurses showed that 88% identified themselves as certified SCNs (all nurses in this study are referred to as SCNs, since they all work within stoma care). In terms of experience, 73% of the nurses had 10 years or more experience of working within stoma care, 16% had 6-10 years' experience, 10% had 3-5 years' experience, and 2% had 0-2 years' experience in this field. Most nurses worked in inpatient settings (68%) and/or outpatient clinics (66%), 16% worked as community nurses and 16% did not specify their work setting.
Pre-operative period of stoma surgery
Planned versus unplanned surgery and pre-operative consultations with health professionals
In this survey population, 68% of patients had had planned stoma surgeries and 31% had had unplanned surgeries. Most patients recalled having pre-operative consultations (broadly defined as any kind of talk/interaction) with a health professional (87%), but 13% did not. The pre-operative consultations were primarily with a surgeon (76%) and/or an SCN (40%), and most often they took place prior to the day of surgery (91%) (Table 1). Of the patients who underwent unplanned surgery, 36% did not recall having any pre-operative consultation with a health professional.
Table 1. Patients' time with health professionals before stoma surgery
| Question: Before having stoma surgery, did you have a pre-operative talk with one or more health professionals preparing you for surgery? If yes, please choose all that apply | Total | Planned | Unplanned |
|---|---|---|---|
| n=6499 | n=4451 | n=1987 | |
| Yes, with a surgeon | 76% | 87% | 52% |
| Yes, with a stoma care nurse | 40% | 49% | 20% |
| Yes, with a doctor | 14% | 17% | 8% |
| Yes, with a ward (general) nurse | 9% | 9% | 7% |
| Yes, other | 4% | 4% | 3% |
| No | 13% | 2% | 36% |
| Don't remember | 2% | 1% | 4% |
| When did the pre-operative talk(s) take place* | n=5136 | n=4003 | n=1104 |
| The same day of surgery | 9% | 3% | 30% |
| Prior to day of surgery | 91% | 97% | 70% |
Pre-operative consultations between SCNs and patients
SCNs were asked about the time they had available to hold pre-operative consultations with patients having either planned or unplanned surgery. Eighty-one per cent of the SCNs reported that they typically had one or more pre-operative consultation with patients undergoing planned surgery. Contrarily, 68% of the nurses responded that they did not have any pre-operative consultations with patients who were having an unplanned surgery (Table 2).
Table 2. Stoma nurse questionnaire: consultations with patients having planned versus unplanned stoma surgeries (n=250)
| Question: How many scheduled consultations do you typically have with each stoma patient having planned/unplanned surgery? | Question: How much time do you typical have per consultation with each stoma patient having planned/unplanned surgery? | ||||
|---|---|---|---|---|---|
| Number of consultations per patient | Planned | Unplanned | Time per consultation | Planned | Unplanned |
| Pre-operatively | Pre-operatively | ||||
| 0 consultations | 19% | 68% | 0–15 minutes | 19% | 70% |
| 1 consultation | 66% | 30% | 16–30 minutes | 23% | 15% |
| 2–3 consultations | 13% | 2% | 31–45 minutes | 19% | 7% |
| 4+ consultations | 2% | 0% | 46+ minutes | 39% | 8% |
| Postoperatively | Postoperatively | ||||
| 0 consultations | 6% | 6% | 0–15 minutes | 8% | 7% |
| 1 consultation | 15% | 15% | 16–30 minutes | 35% | 32% |
| 2–3 consultations | 42% | 44% | 31–45 minutes | 22% | 26% |
| 4+ consultations | 37% | 35% | 46+ minutes | 35% | 35% |
| Preparing for discharge | Preparing for discharge | ||||
| 0 consultations | 11% | 9% | 0–15 minutes | 7% | 10% |
| 1 consultation | 43% | 43% | 16–30 minutes | 30% | 33% |
| 2–3 consultations | 32% | 37% | 31–45 minutes | 26% | 23% |
| 4+ consultations | 14% | 11% | 46+ minutes | 37% | 35% |
| Follow-up first year | Follow-up first year | ||||
| 0 consultations | 10% | 10% | 0–15 minutes | 6% | 9% |
| 1 consultation | 11% | 11% | 16–30 minutes | 30% | 24% |
| 2–3 consultations | 31% | 31% | 31–45 minutes | 33% | 33% |
| 4+ consultations | 49% | 48% | 46+ minutes | 31% | 34% |
Seventy per cent of the SCNs typically have less than 15 minutes per pre-operative consultation with patients having an unplanned surgery (Table 2). In the case of patients having a planned surgery, 39% of SCNs reported that they typically have more than 45 minutes per pre-operative consultation (Table 2).
Weighted averages indicate that pre-operatively SCNs have about 10 minutes per patient having unplanned surgery and 45 minutes per patient undergoing planned surgery.
About half the SCNs (56%) responded that they have sufficient time pre-operatively to prepare patients for a life with a stoma, while the perception of 30% of SCNs was that they did not have sufficient time (Table 3).
Table 3. Nurse responses on whether they have sufficient time to prepare patients for life with a stoma (n=250)
| Question: In general, do you agree or disagree, that you have sufficient time to prepare your stoma patients (physically and/or mentally) for life with a stoma? | |||
|---|---|---|---|
| Pre-operatively | Preparing for discharge | ||
| Fully agree | 23% | Fully agree | 17% |
| Agree | 33% | Agree | 45% |
| Neither agree nor disagree | 14% | Neither agree nor disagree | 15% |
| Disagree | 22% | Disagree | 18% |
| Fully disagree | 8% | Fully disagree | 5% |
| Postoperatively | Follow-up first year | ||
| Fully agree | 15% | Fully agree | 21% |
| Agree | 51% | Agree | 50% |
| Neither agree nor disagree | 11% | Neither agree nor disagree | 10% |
| Disagree | 17% | Disagree | 12% |
| Fully disagree | 7% | Fully disagree | 7% |
Topics most important to discuss with patients pre-operatively
When asked about the most important topics to discuss with patients pre-operatively, the majority of SCNs chose topics related to helping patients understand what a stoma is and helping them to prepare psychologically, ie where the stoma is to be located (stoma marking) (70%), what a stoma looks like (54%), and how to prepare mentally for life with a stoma (48%) (Table 4).
Table 4. Nurses' perception of topics to discuss with patients before surgery
| Question: Which topics do you feel are most important to discuss with your patients before they have stoma surgery? (Up to five topics can be selected) | n=250 |
|---|---|
| Where to locate the stoma (stoma marking) | 70% |
| What a stoma looks like | 54% |
| How to prepare psychologically for life with a stoma | 48% |
| Showing examples of what stoma products look like | 42% |
| How to deal with practicalities when living with a stoma | 40% |
| Why they need stoma surgery | 40% |
| How stoma management will fit with personal circumstances | 32% |
| How to use a stoma product | 29% |
| Explaining how the intestinal system works | 24% |
| Hydration and/or nutrition | 16% |
| How to keep the peristomal skin healthy | 14% |
| How to avoid and cope with leakage issues | 9% |
| Discuss/recommend what stoma product to use | 6% |
| Other | 9% |
| I do not see patients pre-surgery | 10% |
Postoperative period until hospital discharge
Length of hospital stay
For people who had their stoma surgery between 0-1 and 1-4 years previously, 46% reported having a hospital stay of 11 days or longer following their stoma surgery, with just 6-7% reporting a hospital stay of just 1-3 days. The proportion of patients spending 11 days or more in hospital after surgery were higher among those who had undergone surgery 5 years ago or longer (57%). Regardless of time since surgery, one quarter (24-26%) of all patients had spent 7-10 days in hospital following their surgery. A higher proportion (68%) of patients who had undergone unplanned surgeries reported spending 11 days or more in hospital post-surgery compared with patients who had planned surgeries (46%).
Patients were subsequently asked how well they had felt prepared for living with a stoma based on the information and education they had been provided with during their hospital stay. About half (49%) reported that they felt very well or well prepared for life with a stoma. However, 19% felt poorly or very poorly prepared for life with a stoma, and 28% felt neither well nor poorly prepared; 4% answered that they had not been given any information at all during their hospital stay.
Segmenting patients into planned versus unplanned surgery revealed that a higher proportion of those who had undergone planned surgery felt very well or well prepared for life with a stoma (54%) compared with people who had had unplanned surgery (38%). In addition, 34% of the patients who had unplanned surgery did not feel prepared for life with a stoma based on the information they had received while in hospital, as opposed to only 17% of patients who had planned surgery.
Moreover, a higher proportion of patients who had a pre-operative consultation with an SCN felt that they had been very well or well prepared for life with a stoma (59%), compared with patients who had not had such pre-operative consultations (43%). The degrees of preparedness for life with a stoma based on the information and education provided during patients' hospital stay were similar when segmenting patients into new users, experienced users and veterans.
Postoperative consultations
The majority of SCNs (79%) estimated that they typically have two or more consultations scheduled with patients postoperatively, independently of whether the surgery is planned or unplanned. Furthermore, 90% of SCNs typically have one or more consultations with patients to prepare for discharge (Table 2). Weighted averages indicate that the time spent by SCNs with patients postoperatively until discharge is about 4 hours.
Approximately two out of three SCNs consider they have sufficient time postoperatively until discharge to prepare patients for life with a stoma. One quarter of nurses responded that they do not feel they have sufficient time to do so (Table 3).
The SCNs were asked to select the topics they find most relevant to discuss with patients after stoma surgery. The most important topics were primarily focused on practical aspects, specifically how to use a stoma product (82%), how to keep the skin healthy in the peristomal area (66%), and how to avoid and cope with leakage issues (62%) (Table 5). Furthermore, in preparing patients to live a ‘normal’ life with a stoma, SCNs provided advice on diet (69%), how to engage in physical activities (60%), and how to deal with the practicalities of having to bring products with you (58%) (Table 5).
Table 5. Nurses' responses on topics to discuss with patients after surgery
| Question: Which topics do you feel are most important to discuss with your patients after they have stoma surgery? (Up to five topics can be selected) | n=250 |
|---|---|
| How to use a stoma product | 82% |
| How to keep the skin healthy in the peristomal area | 66% |
| How to avoid and cope with leakage issues | 62% |
| Hydration and/or nutrition | 56% |
| How to deal with practicalities when living with a stoma | 44% |
| How stoma management will fit with personal circumstances | 36% |
| Discuss/recommend what stoma product to use | 32% |
| How the peristomal area can change over time | 30% |
| How to prepare psychologically for life with a stoma | 28% |
| Showing examples of what stoma products look like | 17% |
| Explaining how the intestinal system works | 9% |
| Why they need stoma surgery | 4% |
| Other | 6% |
| I do not see patients post-surgery | 2% |
| Question: Which topics are most relevant to discuss with your patients when it comes to their ability to live a ‘normal’ life with a stoma? (Up to five topics can be selected) | n=250 |
| What to eat/drink (diet advice) | 69% |
| How to engage in physical activities | 60% |
| How to deal with practicalities of having to bring products with you | 58% |
| How to engage in social activities | 50% |
| How to order products | 48% |
| How the peristomal area can change over time | 46% |
| How to have an intimate relationship | 42% |
| Considerations when travelling/on vacation | 38% |
| What clothes to wear for different occasions | 28% |
| What level of details to share with family/friends | 26% |
| Other | 7% |
In all, 56% of SCNs estimated that they spent an equal amount of time teaching patients about the practical and emotional aspects surrounding stoma management.
Choice of first stoma care product
Stoma formation necessitates use of stoma care products for the collection of urine or faeces. Both the surveys for patients and SCNs included questions concerning choice of first stoma products. Almost half the patients (47%) responded that they had made the decision about choice of discharge product solution, together with a health professional (eg SCN). A slightly lower proportion (36%) of patients stated that a health professional had made the decision about their discharge product, and 15% of patients reported making the decision themselves.
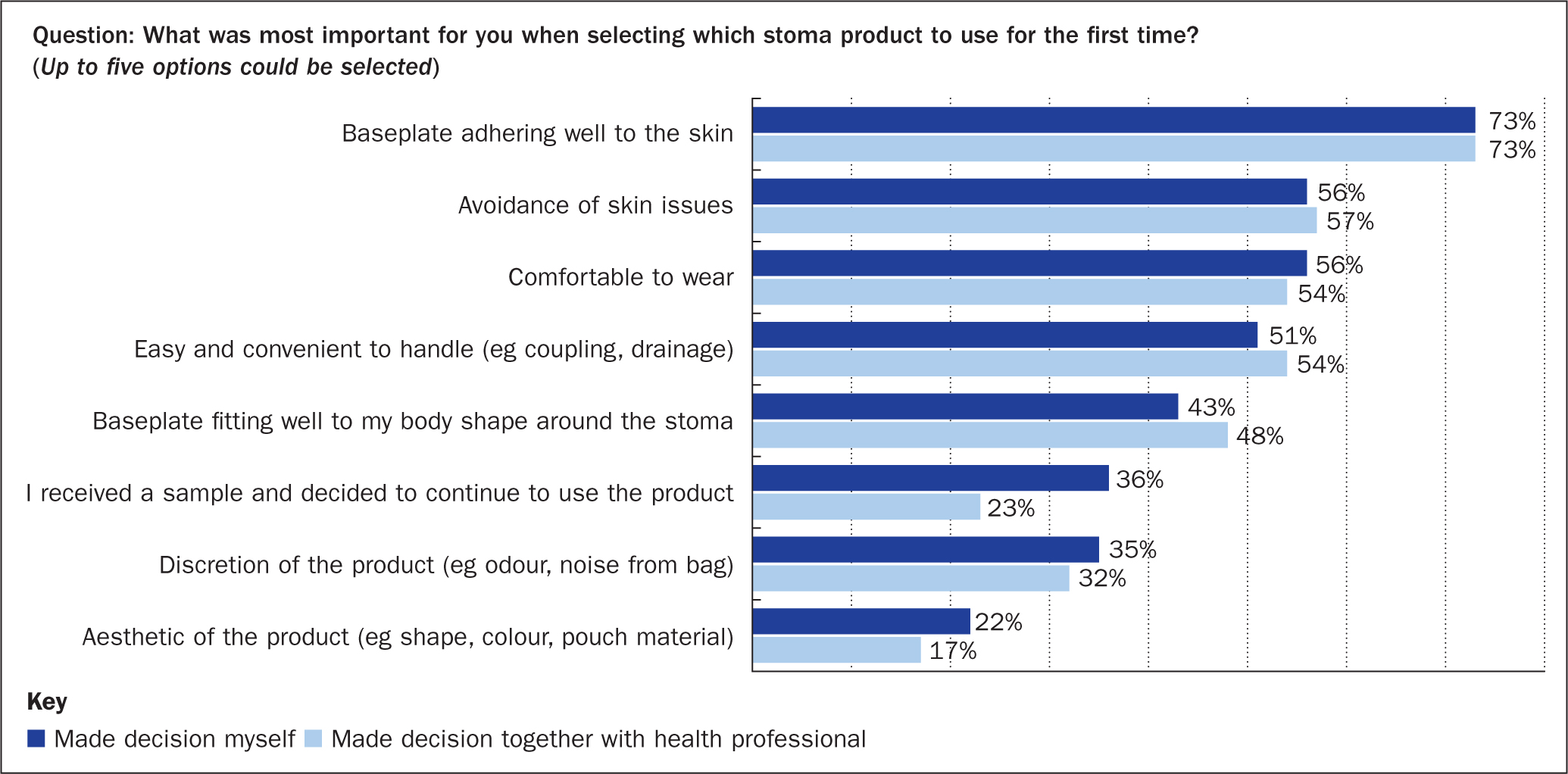
Patients (n=4016) who had been involved in making the decision about which discharge product to choose were asked to select the most important factors for making their choice. Independently of whether the decision had been made solely by the patient, or together with a health professional, the most important factors in choosing products were: baseplate adheres well to skin, avoiding skin issues, device is comfortable to wear, and it is easy and convenient to handle (Figure 1). Patients who decided on the choice of discharge products themselves valued product samples and it was evident that product aesthetics were more important than if the decision had been made together with a health professional (Figure 1).
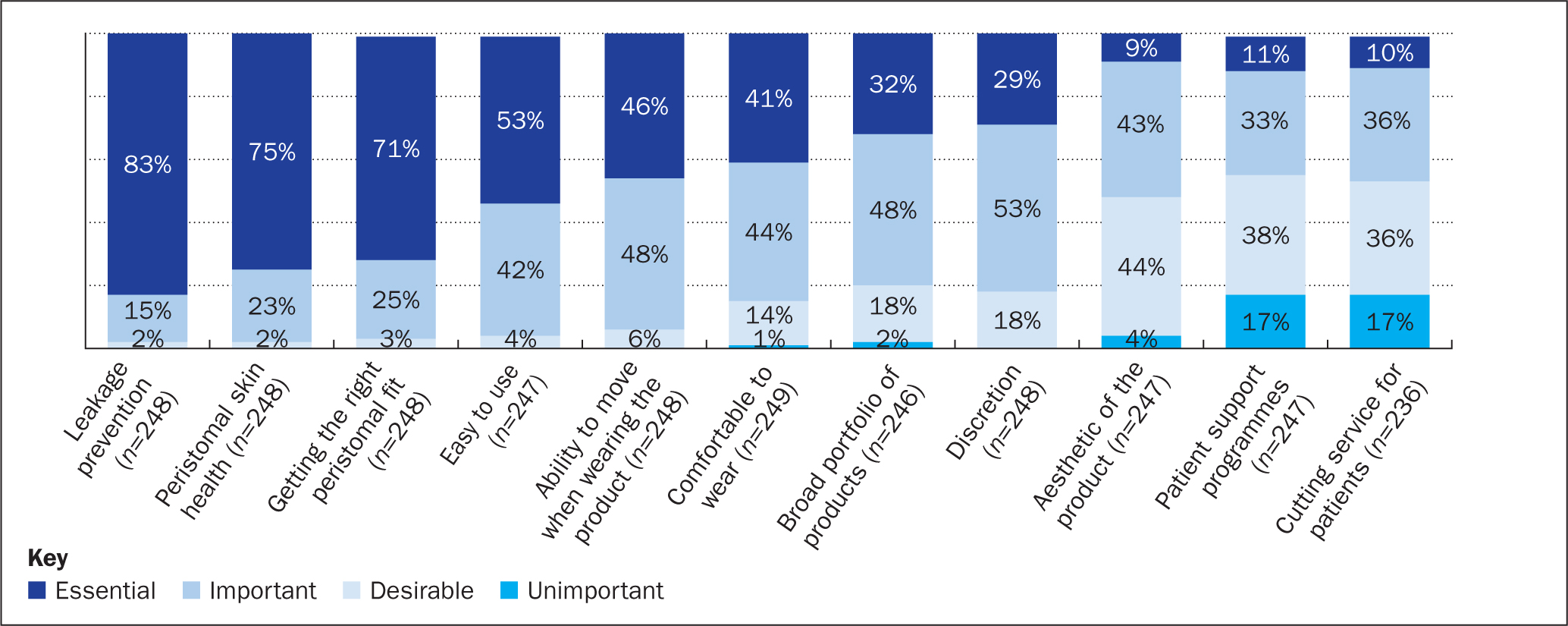
Most SCNs reported that leakage prevention, peristomal skin health and getting the right peristomal fit were essential aspects to consider as part of their clinical assessment of patients when selecting which products to use (Figure 2). Of less importance to SCNs are aesthetics of a product, the availability of patient support programmes and the availability of a cutting service for patients (Figure 2).
First year post-discharge
Life satisfaction and complications reported by patients
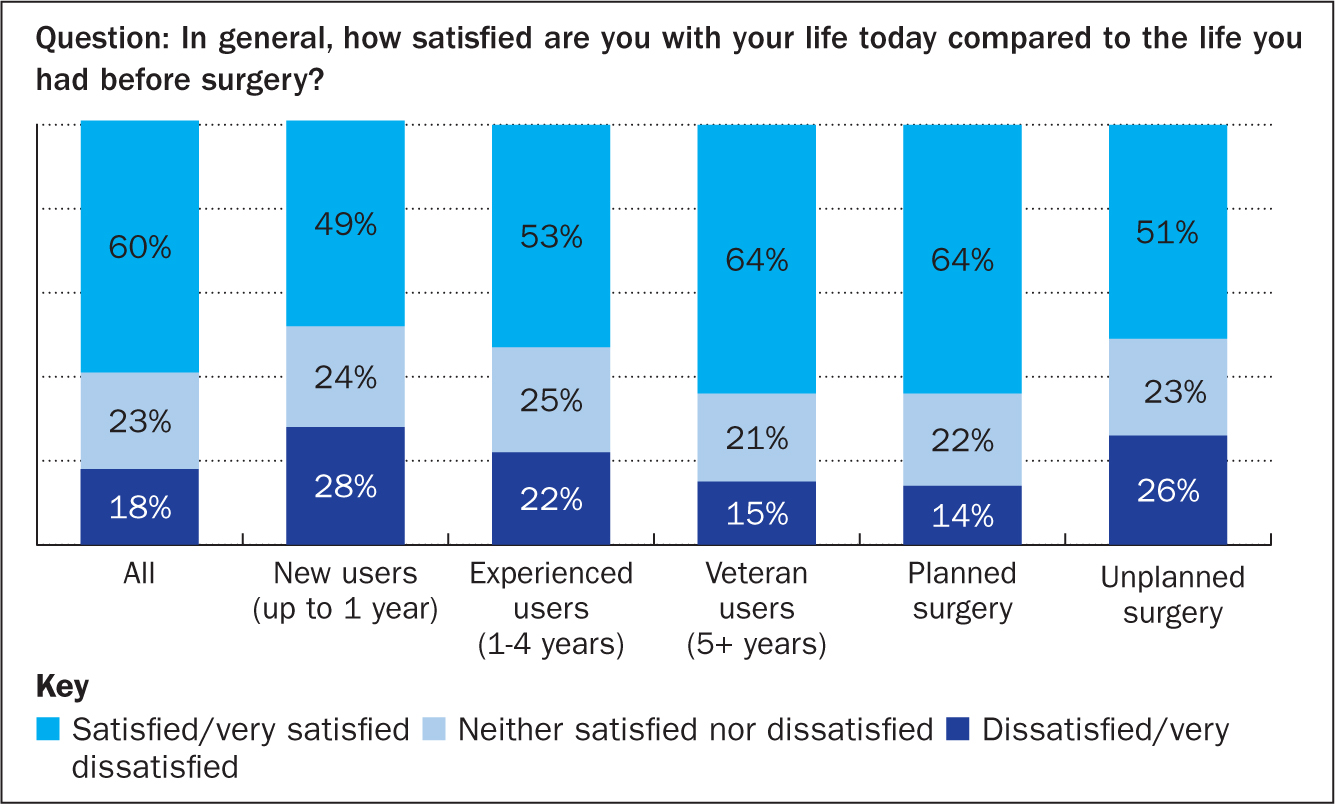
Of the total cohort, 60% reported being satisfied or very satisfied with their lives today compared with their situation before surgery, and 18% were dissatisfied or very dissatisfied with their life today. The proportion of patients who were dissatisfied or very dissatisfied was highest among patient who had recently had surgery (28%) and among those who had undergone unplanned surgery (26%) (Figure 3).
Patients were asked to choose from 17 pre-defined daily struggles. Fifty-one per cent reported struggling with embarrassing situations, 35% with keeping the peristomal skin healthy and 28% with having to deal with all the practicalities related to having a stoma (Table 6). Only 17% responded that they did not have any struggles in their daily life of living with a stoma.
Table 6. Topics patients commonly struggle with
| Question: Which of these topics (if any) do you struggle with most in your daily life with a stoma? (Up to five topics can be selected) | n=6500 |
|---|---|
| Having embarrassing situations | 51% |
| Keeping the skin healthy in the area around the stoma | 35% |
| Having to deal with all the practicalities around having a stoma | 28% |
| Not being able to exercise the way/or as much as I want to | 20% |
| Having an intimate relationship | 20% |
| Not being in control of my body | 20% |
| Have no daily struggles | 17% |
| Having to change the product | 17% |
| Having a body that I do not like | 16% |
| Feeling different from other people | 15% |
| Not being able to eat/drink the things I enjoy | 14% |
| Being diagnosed with an illness | 9% |
| Other | 8% |
| Not having someone to talk to about my life with a stoma | 6% |
| Not being able to work | 6% |
| Not being able to play my role for my loved ones | 6% |
| Not recognising my stoma as being a part of me | 6% |
| Feeling isolated | 4% |
| Not being able to maintain a healthy lifestyle | 4% |
| Don't know | 1% |
Time with patients in the first year post-discharge
Half the SCNs typically reported having 4 or more consultations with each patient in the first year post-discharge, and about 40% reported that they have 1-3 consultations with each patient (Table 2). Weighted averages indicate that SCNs have about 3 hours together with a patient in the first year post-discharge. Seventy-one per cent of the SCNs reported that they have sufficient time to prepare patients mentally and physically to a life of living with a stoma in the first year following surgery, with 19% responding that they do not have sufficient time to do so.
SCNs use different channels to interact with their patients, ie face-to-face consultations (97%), telephone calls (88%), emails/e-consultations (42%), SMS/messaging apps (31%) and video calls (11%). Face-to-face interactions are the most common way of engaging with patients (61% of time), with the remaining time distributed between telephone calls (16%), emails (7%), SMS (8%) and video calls (7%).
Discussion
The Ostomy Life Study 2022 was conducted using retrospective, self-reported questionnaires completed by both patients and SCNs to understand how patients undergoing stoma surgery and SCNs interact to prepare patients for surgery and to life with a stoma post-surgery.
There are established clinical practice guidelines for stoma care which recommend both pre-operative and postoperative training and education of patients (Hendren et al, 2015; Chabal et al, 2021). This survey has highlighted that most patients (87%) report having pre-operative consultations with a health professional, but also that the availability of pre-operative consultations with a health professional differed and depended on whether the patients had a planned or unplanned surgery. More than one-third (36%) of patients with unplanned surgery did not recall having any pre-operative consultation with a health professional, with only 2% of patients who underwent planned surgery reporting that they had not had such consultations.
Recommendations on pre-operative care focus primarily on stoma site marking and educational topics related to anatomy/physiology, surgical procedure, demonstration of stoma products, lifestyle adjustments and psychological preparation (Goldberg et al, 2010) – and this aligns well with the topics focused on pre-operatively by the SCNs in this study. Concerningly, 30% of SCNs in the present study reported that they did not have sufficient time pre-operatively to prepare patients for life with a stoma, despite the fact that the importance of stoma site marking and pre-operative education are well-documented as minimising the risk of stomal complications and improving patient rehabilitation (Hsu et al, 2020; Zelga et al, 2021; Ambe et al, 2022). This may partially reflect that SCNs who responded to the questionnaire were unable to differentiate between time available for patients having planned versus unplanned surgeries, or that many patients primarily had pre-operative consultations with surgeons. Furthermore, some patients are placed on strict patient pathways (eg those diagnosed with cancer), which may restrict time for patients to have with SCNs to allow for psychological adjustment.
Following stoma surgery, patients recover in hospital and must begin adjustment to a new life of living with a stoma. In the present survey, about half the patients spent ≥11 days, one quarter of patients spent 7-10 days and one quarter spent 1-6 days in hospital before being discharged. Short hospital stays post-surgery may limit the opportunity to interact with SCNs and reduce the time available to learn to handle and manage pouching systems (Kwiatt and Kawata, 2013). Pre-operative counselling with SCNs for patients with planned surgery can, however, encourage faster proficiency in stoma care management and may promote earlier discharge (Chaudhri et al, 2005; Forsmo et al, 2016). The length of hospital stay for patients who responded in this study is similar to numbers from a retrospective cohort study reported from the USA, where the median total length of hospital stay in relation to stoma surgery was 9 days and median length of stay in hospital post-surgery was 7 days (Schott et al, 2022).
During postoperative consultations with patients, SCNs in this study focused on practical aspects of stoma care, such as stoma product training, common complications (PSCs and leakage), hydration and practicalities of living with a stoma, as well as emotional aspects of living with a stoma and ways to engage in social and physical activities, as per the recommendations outlined in best practice guidelines for stoma care (Goldberg et al, 2010). Even though SCNs overall followed guidelines for postoperative patient education, almost one quarter of them did not feel they had sufficient time to prepare patients properly for life with a stoma before hospital discharge. Enhanced recovery after surgery is considered best practice (Marsden, 2020); this, together with the constant pressure to reduce length of hospital stay and release beds, can place further time constraints on SCNs and may impact their ability to prepare patients for life with a stoma.
When asking patients about their perception of preparedness for life with a stoma, based on information and education provided during their hospital stay, about half (49%) of the respondents felt prepared for life with a stoma. However, 17% of those who underwent planned surgery and 34% of patients who had unplanned surgery did not feel prepared for living with a stoma based on the education they had received during their hospital stay. Pre-operative consultations with SCNs improved patients' perception of preparedness for life following their surgery.
The authors' findings support those of a previous survey, in which a sizeable proportion of new patients discharged felt poorly equipped to undertake their stoma care, for example more than half the patients were unable to change a new pouch independently (Wasserman and McGee, 2017). Previous, anecdotal reports have indicated that some patients who underwent emergency surgery experienced feelings of abandonment and had an increased risk of psychological distress due to lack of pre-operative information and limited time postoperatively to deliver the necessary information (Borwell, 2009; Bowles et al, 2022a). Other studies highlighted that overall patients with unplanned surgery have higher complication rates than those who have planned surgery (Cottam et al, 2007; Braumann et al, 2019). This is due primarily to increased risk of experiencing stoma retraction (Braumann et al, 2019; Pearson et al, 2020) and skin irritation (Braumann et al, 2019). Patients undergoing unplanned stoma surgery also show lower levels of acceptance and social engagement compared with those having planned surgery when using the Ostomy Adjustment Inventory-23 (Dellafiore et al, 2022), which again probably reflects their lack of preparation and information before surgery. Further studies are needed to identify the impact of planned versus unplanned surgery on patients' psychological adjustment to life with a stoma and self-care ability following hospital discharge, and whether tailored post-surgery stoma care programmes are needed for those who undergo unplanned surgery.
In provision of patient education, SCNs may adopt instruments that have recently become available to assess and prevent complications associated with stoma formation. Such instruments may also be valuable in training health professionals who do not necessarily have specialist knowledge of stoma care, but who may encounter stoma patients, to raise awareness of the signs and symptoms that may need expert evaluation to minimise the risk of a given complication to increase in severity level, and to promote standardisation in communication between patients and health professionals. This could support and empower colleagues, and enhance collaboration to help address complications arising from stoma surgery, particularly to mitigate staff shortages and help improve patients' adaption and recovery, both on wards and within stoma care teams.
Instruments such as the Peristomal Body Profile Assessment Tool (Colwell et al, 2019; James-Reid et al, 2019), the Ostomy Skin Tool 2.0 (Martins et al, 2022b) and Ostomy Leakage Impact tool (Nafees et al, 2018) can be relevant to stoma care to ensure the right fit of the pouching system for individual patients, enable effective assessment of PSCs and help monitor of mental wellbeing. Such a preventive approach, which is also reflected in the Risk Factor Model on PSCs (Hansen et al, 2022), may ultimately lead to a reduction in stoma-related complications (Tonks et al, 2022; Vendelbo et al, 2023) and hence relieve pressure on nurses and wards.
Stoma formation necessitates the use of stoma care products for the safe collection of faeces or urine. Choice of pouching system (flat, convex or concave baseplate) and appropriate use of accessories are key in minimising the risk of experiencing leakages (Vendelbo et al, 2023), which is a major concern for most people living with a stoma (Jeppesen et al, 2022). In the present study, 83% of patients reported that a health professional was either involved in or responsible for the choice of discharge stoma product, identifying aspects to address when choosing a first stoma product, such as prevention of leakage, peristomal skin health and getting the right peristomal fit. Preference for pouching system features may also change over time, with the initial focus following stoma surgery geared towards a reliable pouching system that will ensure safe discharge. Changes in a patient's physical and psychological recovery over time may require adjustments of pouching system to resolve potential complications arising from choice of discharge stoma product. Use of The Peristomal Body Profile Assessment Tool has been shown to help health professionals choose the best stoma product, significantly reducing the number of leakages of stomal effluent experienced by patients and improving their quality of life (Tonks et al, 2022; Vendelbo et al, 2023).
Concerningly, this survey revealed that half the respondents struggled with embarrassing situations and one third struggled with PSCs daily. This is an indication that many people with a stoma may not use optimal product solutions for their peristomal body profiles or do not have the necessary skills to adequately manage stoma self-care; thus, many could probably benefit from additional care post-hospital discharge to address these issues. The authors' study corroborates a previous study showing that two out of three people with a stoma struggled with one or more self-care problems several years post-surgery (Bulkley et al, 2018). Episodes of leakage with stomal effluent progressing outside the baseplate and soiling clothes is often embarrassing for the individual and have a negative impact on people's quality of life (Jeppesen et al, 2022). This highlights the important role of SCNs, in terms of their ongoing contact and consultation with patients for continued review, as well as their input in selecting or re-selecting a pouching system that will provide the most secure seal. The study findings also highlight the importance of SCNs' continued focus on the psychosocial aspects of living with a stoma to help improve life satisfaction among patients.
This survey has highlighted that SCNs are key in preparing patients for stoma surgery and for living with a stoma, both mentally and practically. It has also shown that patients with unplanned surgery could benefit from additional attention postoperatively to ensure they receive adequate education and training to better equip them for life with a stoma. As emphasised in this survey, a constraint in providing sufficient education and training to all stoma patients before discharge is that more than one third of SCNs perceived that they had insufficient time to prepare patients adequately for life with a stoma. This resonates with the issue raised previously – that there is a lack of specialist SCNs to ensure there is sufficient time for patient consultations both in hospital and in the community (Bowles et al, 2022b). Furthermore, these specialist nurses provide vital education and expertise, benefiting the wider multidisciplinary team, with a corresponding positive impact on patients, colleagues and the healthcare system.
Limitations
In interpreting the results of this study it is important to consider potential limitations. The patients in the survey were predominantly individuals who had had surgery 5 years ago or longer (64%). Since patient data were self-reported and not collected by health professionals as part of a clinical study, the responses may have been affected by recall bias, especially on topics concerning stoma surgery and the stoma care service provided in relation to this. Furthermore, the surveys were distributed to participants in many countries: this, while providing an international representation of the stoma and SCN populations, also means that national, regional and local differences in stoma care services could influence the responses. It was not within the scope of this investigation to explore country-specific differences.
Conclusion
The study revealed that SCNs are key in preparing patients for stoma surgery and in adjustment to a new life with a stoma. About two thirds of SCNs in the present study felt that they had sufficient time to prepare patients for stoma surgery and life with a stoma. SCNs primarily undertake the education and training of patients when they are mentally ready to embrace the information.
The study revealed considerable variations in stoma care services experienced by patients having planned versus unplanned surgery, indicating that additional attention should be provided to patients undergoing unplanned stoma surgery to better prepare them for life with a stoma.
KEY POINTS
- Stoma care nurses are key in helping patients to adjust to a new life with a stoma, both psychologically and practically
- 30% of stoma care nurses do not perceive that they have sufficient time pre-operatively to prepare patients for a life with a stoma
- About half the patients felt prepared for life with a stoma based on the information and education provided during their hospital stay. Those with unplanned stoma surgeries felt less prepared than those who had planned surgeries
- Variations in stoma care services were experienced by patients having planned versus unplanned stoma surgeries.
CPD reflective questions
- The survey highlights variations in patient experience of stoma care services for planned versus unplanned stoma surgeries. Does this also reflect the situation with the stoma care service provided at your facility?
- Have you considered a specific pathway for patients with unplanned surgery to ensure that they are prepared for life with a stoma? If not, then reflect on initiatives that can improve patients' perception of being prepared for life with a stoma
- Do you use currently available tools in helping patients to adjust to a new life with a stoma and manage complications, and are the tools sufficient?


