It is estimated that 700 000 people in Europe and more than 1 million in the USA live with a stoma (Claessens et al, 2015). Stoma effluent leakage is a common problem and a great concern for people living with a stoma (Porrett et al, 2011; Claessens et al, 2015). In a survey conducted a decade ago, only 13% reported to never experience incidences of leakage (Porrett et al, 2011). In the recent Ostomy Life Study 2019, 76% of the respondents, independent of stoma type, reported experiencing leakage of stomal effluent underneath the baseplate at least once a month, while 65% experienced leakage of effluent outside the baseplate and on to clothes at least once within the previous year (Anne Steen Hansen, personal communication).
Leakage of stomal effluent is often socially uncomfortable for the individual and negatively affects quality of life (Davis et al, 2011; Claessens et al, 2015). Importantly, leakage of stomal effluent is also a significant risk factor in the development of peristomal skin complications (PSCs) (Voegeli et al, 2020), especially irritant contact dermatitis (ICD) (Doctor and Colibaseanu, 2017; Salvadalena et al, 2020). In the diagnosis of PSCs, up to 77% of the cases have been associated with contact between stomal effluent and the skin (Herlufsen et al, 2006).
The aetiology of ICD is multifactorial, but still remains incompletely understood (Gray et al, 2013; Koudounas et al, 2020). However, two key factors contributing to the progression of ICD are moisture (moisture-associated skin damage) and enzymes from stomal effluent (Doctor and Colibaseanu, 2017). Effluent from faecal stomas (colostomy, ileostomy and jejunostomy) contains immunoreactive, lipolytic and proteolytic enzymes that can compromise the skin barrier (Bohe et al, 1983; Andersen et al, 1994). People with an ileostomy have a greater risk of severe PSCs than people with a colostomy (Salvadalena et al, 2020; Voegeli et al, 2020), since effluent from an ileostomy often has a higher content of moisture and digestive enzymes compared with effluent from a colostomy (Gray et al, 2013). Urine contains no enzymes and has an average pH of around 6, but over time urine can, due to the moisture, lead to irritation and maceration of skin (Walsh, 1992; Berti-Hearn and Elliott, 2019). Compromised skin can ultimately lead to less efficient adhesion of the pouching system to the skin, so the risk of leakage increases and further skin irritation is promoted in a vicious circle (Rolstad and Erwin-Toth, 2004).
In a survey from 2002, 89% of patients with PSCs thought it was due to an allergic reaction to their pouching system (Smith et al, 2002), although allergic contact dermatitis is actually an uncommon cause of PSCs (0–9%) (Nybaek and Jemec, 2010; Martins et al, 2011; Salvadalena et al, 2020). This indicates a lack of knowledge about the risk factors leading to PSCs (Voegeli et al, 2020). In other research, only 38–58% of people with a stoma who were diagnosed with a PSC agreed that they had a skin disorder (Herlufsen et al, 2006; Martins et al, 2011). In prevention of leakage and the associated PSCs it is important that people living with a stoma can recognise symptoms of PSCs and understand the common causes (John et al, 2019). Furthermore, it is important to understand when a change of baseplate is needed and situations in which consultations with health professionals are necessary (John et al, 2019).
Although the term ‘leakage’ is widely used, there has been no standard definition of ‘leakage’ (Nafees et al, 2018). By using qualitative interviews with health professionals and people living with a stoma Nafees et al attempted to define leakage for the development of the ‘ostomy leak impact tool’, a tool for objective assessment of the burden of leakage for people living with a stoma (Nafees et al, 2018). Here two broad definitions of leakage were given: ‘leakage under the baseplate’ and ‘leakage outside the baseplate’ (Nafees et al, 2018). However, there has been little exploration regarding what extent of stomal effluent people with a stoma perceive as leakage and whether there are any discrepancies in the perception of leakage between health professionals and people living with a stoma.
The objective of this article, a subanalysis of the Ostomy Life Study 2019, was to investigate how people living with a stoma and stoma care nurses perceive leakage and to better understand the causes of leakage.
Methods
The Ostomy Life Study 2019 consisted of a pair of retrospective, self-reported surveys, conducted among people living with a stoma and stoma care nurses (Fellows et al, 2021).
Survey for people with a stoma
A total of 54 614 people living with a stoma from 17 countries (the USA, Canada, Brazil, China, Australia, Japan, Belgium, Denmark, France, Germany, Italy, the Netherlands, Norway, Poland, Sweden, Switzerland and the UK) were invited to participate in the Ostomy Life Study 2019. The participants were randomly selected from local Coloplast A/S databases with stratified sampling to reflect each country’s market size. Participants received the survey online.
Before answering the survey, all participants consented to their participation and allowed Coloplast A/S to use the collected data in an aggregated and anonymous representation for internal and publication purposes
The survey sent to people living with a stoma contained questions regarding demographics, description of the stoma and the use of appliances and supporting products (accessories). For people not irrigating their stoma, additional questions were asked regarding leakage, PSCs and interactions with health professionals. Every question had predefined response options, but some questions had the option ‘other reason’, coupled with the opportunity to write an individual answer.
Criteria for excluding individuals from the analysis were: if all questions were answered within 15 minutes (it was estimated that the survey would take around 30 minutes to complete), if more than 30% of the answers were ‘don’t know’ or if the participant did not finish the survey.
Survey for nurses
Stoma care nurse participants (n=328) received their survey online, or in a paper version at the European Council of Enterostomal Therapist (ECET) Congress held in Rome, June 2019, or at the Coloplast Ostomy Forum, December 2019. The purpose of collecting data from these sources was to reach nurses with different backgrounds and experience levels. Before answering the survey, all nurses consented to their participation and allowed Coloplast A/S to use the collected data in aggregated and anonymous representations for internal and publication purposes.
Leakage scale
In the survey, the participants were shown pictures of baseplates with different patterns of effluent to investigate the degree of effluent being perceived as leakage (Figure 1). People with faecal stomas (colostomy, ileostomy or jejunostomy) were shown pictures with faeces, whereas people with a urostomy were shown pictures with urine. Stoma care nurses were only shown pictures with faeces.
Data analysis
Microsoft Excel was used for collection of data and GraphPad Prism v9 was used for preparation of figures (GraphPad Software, San Diego, California USA). Only descriptive statistics were used for the analysis.
Results
Demography and baseline characteristics of the participants
A total of 5187 subjects completed the survey for people living with a stoma. People irrigating their stoma were excluded from the extended questionnaire concerning experiences of leakage and PSCs, leaving a total of 4209 subjects responding to this questionnaire. Among this number, 56% were male and 43% female, and 62% were aged over 60 years (Table 1). In terms of stoma type, 41% had an ileostomy or jejunostomy, 39% a colostomy and 21% a urostomy; 3% of the respondents had more than one stoma. Approximately 16% of the respondents recently had their stoma surgery (less than 12 months), while 55% had had their stoma for more than 5 years.
Table 1. Demography and characteristics of respondents living with a stoma
| n | % | |
|---|---|---|
| Total respondents | 4209 | 100% |
| Age | ||
| Below 39 years old | 289 | 7% |
| 40–59 years old | 1318 | 31% |
| 60 years or older | 2595 | 62% |
| Do not wish to answer | 7 | 0% |
| Gender | ||
| Male | 2371 | 56% |
| Female | 1826 | 43% |
| Do not wish to answer | 12 | 0% |
| Stoma type | ||
| Colostomy | 1661 | 39% |
| Ileostomy or jejunostomy | 1734 | 41% |
| Urostomy | 903 | 21% |
| More than one stoma | 133 | 3% |
| Do not know | 48 | 1% |
| Time since surgery | ||
| 0–12 months ago | 657 | 16% |
| 1–4 years ago | 1225 | 29% |
| 5 years or more ago | 2319 | 55% |
| Do not wish to answer | 8 | 0% |
In addition to the people living with a stoma, 328 stoma care nurses participated in the survey and received questions about leakage and PSCs. Among the nurses, most were certified stoma care nurses (84%) with more than 10 years of experience (70%), many worked in a surgical department (73%) and most cared for both inpatients and outpatients (68%) (Table 2). Geographically, the stoma care nurses were working in Western Europe (61%), Eastern Europe (14%), Middle East (12%), North America (8%) and the remainder from other regions.
Table 2. Characteristics of stoma care nurses responding to survey
| % | |
|---|---|
| Certified stoma care nurse (n=311)* | |
| Yes | 84% |
| No | 16% |
| Experience level (n=326) | |
| 0–2 years | 6% |
| 3–5 years | 8% |
| 6–10 years | 17% |
| More than 10 years | 70% |
| Region (n=305) | |
| Western Europe | 61% |
| Eastern Europe | 14% |
| Middle East | 12% |
| North America | 8% |
| Asia | < 4% |
| Other | < 2% |
| Workplace (n=328) | |
| Surgical department | 73% |
| Medical department | 19% |
| Other | 26% |
| Type of patients (n=306) | |
| Outpatients | 10% |
| Inpatients | 22% |
| Both | 68% |
Perception of leakage by people living with a stoma
The respondents indicated whether different patterns of effluent (Figure 1) were perceived as leakage or not. Most of the respondents considered it as leakage when effluent reached outside the edges of the baseplate (89-90% for people living with a colostomy, ileostomy or jejunostomy (Figure 2a) and 88-90% for people living with a urostomy) (Figure 2b). When faeces or urine covered most of the baseplate, but did not extend outside of the baseplate, this was also perceived as leakage by most of the respondents with a colostomy, an ileostomy or a jejunostomy (83%) (Figure 2a), but only by 57% of respondents with a urostomy (Figure 2b). Interestingly, most of the respondents did not consider faeces or urine close to the stoma as leakage (81% for people living a colostomy, ileostomy or jejunostomy and 91% for people living with a urostomy) (Figure 2aand2b).

Frequency of leakage estimated from pictures of baseplates
The respondents living with a stoma were subsequently asked to estimate the frequency of their personal leakage pattern, by answering how often, out of 10 baseplates, theirs resembled one of the displayed effluent leakage patterns (Figure 1).
For respondents with a faecal stoma, on average only 2.9 out of 10 baseplates were estimated to be free of faeces (Figure 3a), whereas baseplates containing faeces close to the stoma were the most common (4 out of 10 baseplates). Faeces covering most of the baseplate was estimated for 1.7 out of 10 baseplates, while faeces running in channels reaching the outside edges of the baseplate and faeces suddenly running outside the edges of the baseplate were less common (0.9 out of 10 baseplates and 0.5 out of 10 baseplates, respectively).
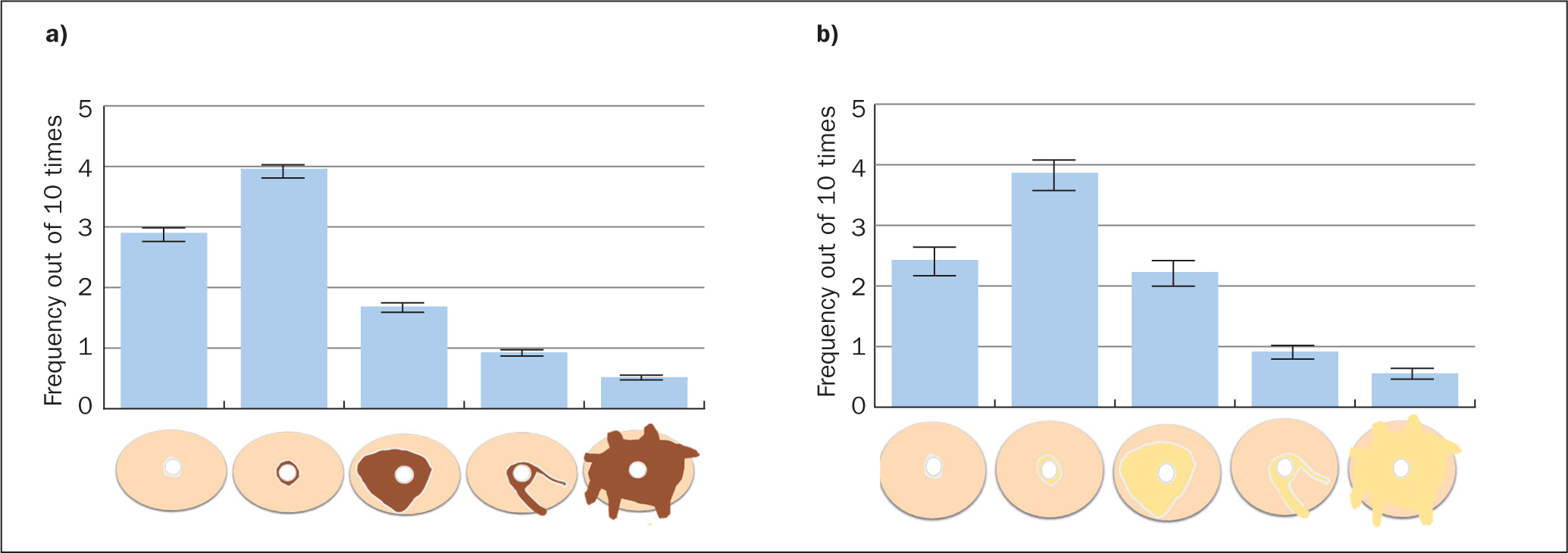
Baseplate leakage frequencies reported by people with a urostomy were similar to the pattern reported by people with a faecal stoma. Only 2.4 out of 10 baseplates were estimated to be free of urine, whereas 3.9 out of 10 baseplates were estimated to contain urine close to the stoma. Urine covering most of the baseplate was estimated for 2.2 out of 10 baseplates, while urine reaching outside the baseplate again was less common (Figure 3b).
Perception of leakage by stoma care nurses
Among the stoma care nurses, 70% did not perceive effluent close to the stoma as leakage, whereas most nurses (93-98%) perceived all other effluent patterns as leakage, regardless of whether the effluent reached the outside edges of the baseplate or not (Figure 2c).
Nurses’ perceptions of reasons for leakage
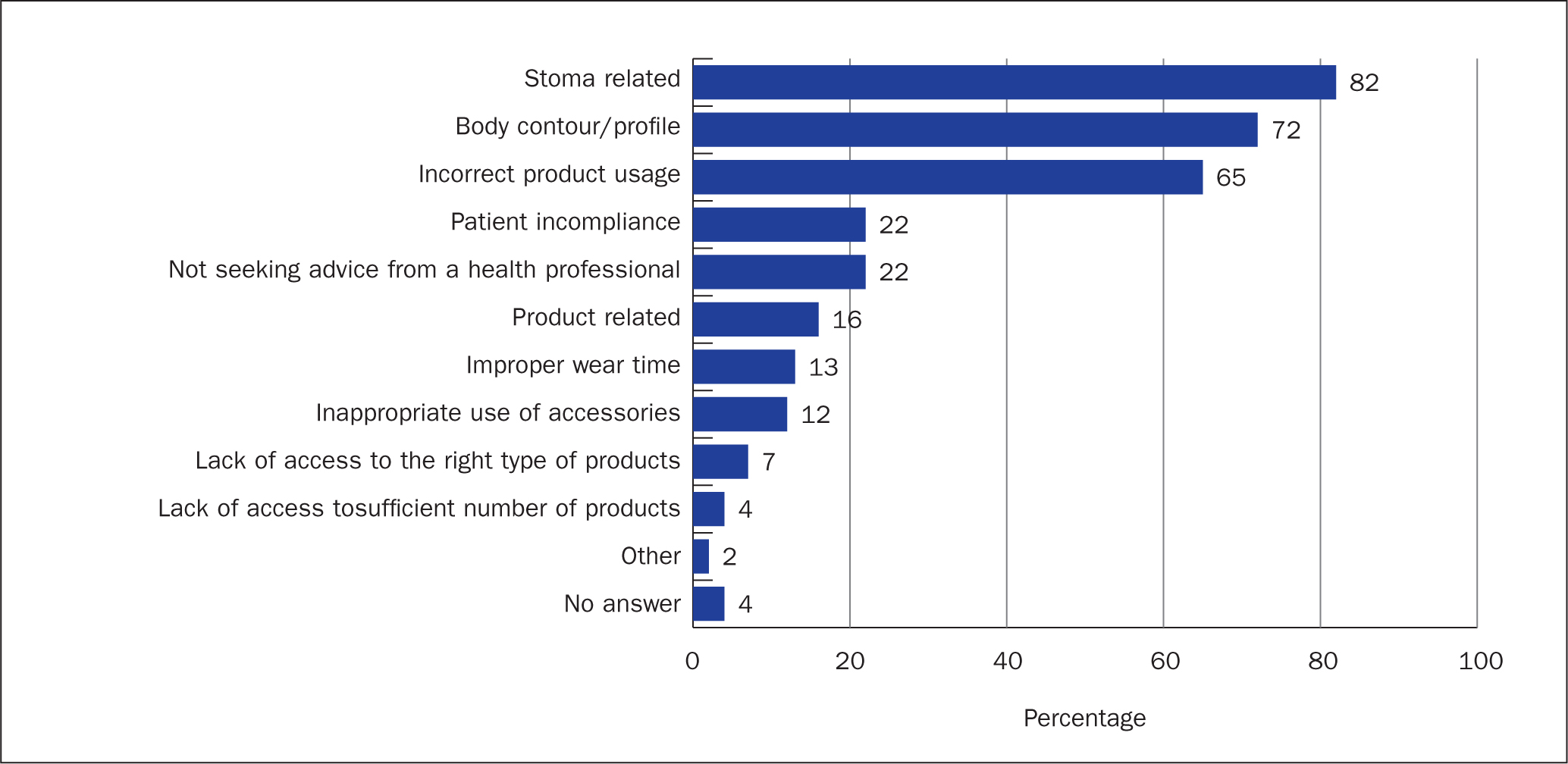
The three main reasons why patients experienced leakage issues were rated by most of the nurses as stoma related (eg retracted stoma, poorly performed surgery, type of stoma, poorly located stoma) (82%), related to the patient’s body profile (72%), and incorrect product usage (65%) (Figure 4). The options ‘patient incompliance’ and ‘not seeking advice from a health professional’ were also considered within the three main reasons for leakage by many of the nurses (22% in both cases). The lack of access to the right type of products or lack of sufficient number of products were only considered to be among the three main reasons for leakage issues by 4-7% of the nurses (Figure 4).
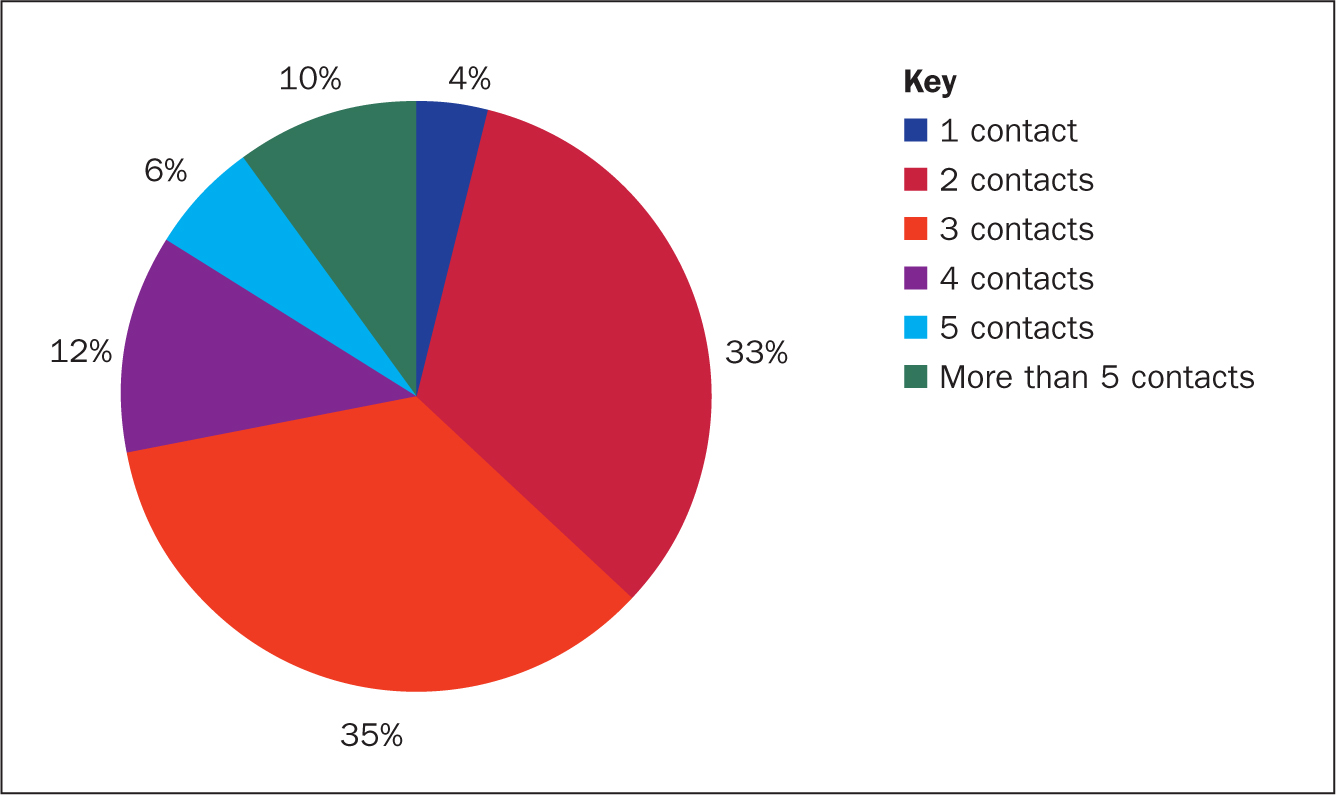
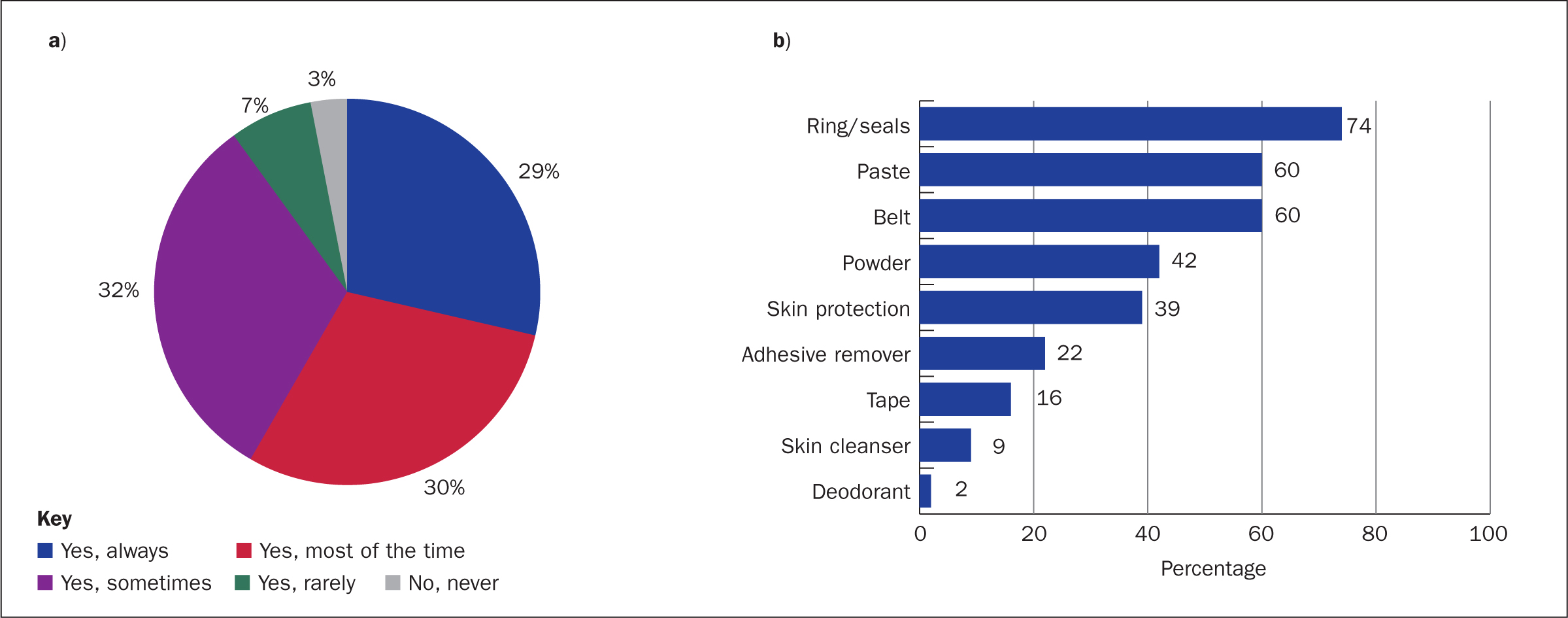
In 96% of cases the stoma care nurses reported that two or more patient consultations would be needed to close the case of a person’s leakage issue (Figure 5). In order to alleviate the issues of leakage the stoma care nurses ‘always’ or ‘most of the time’ (59%) advised patients to use supporting products (Figure 6a), with seals, paste and belts being the most recommended products (Figure 6b).
Discussion
Episodes of stomal effluent leakage and the related worry of leakage are common problems for people living with a stoma (Claessens et al, 2015). The term ‘leakage’ is widely used, but it is not clearly understood how people living with a stoma perceive the term. Nafees et al (2018) and colleagues suggested making a distinction between ‘leakage under the baseplate’ and ‘leakage outside baseplate (and onto clothes)’. The term ‘seepage’ is sometimes used to describe effluent under the baseplate, however, it does not seem widely accepted that seepage only refers to effluent under the baseplate, since ‘seepage’ is used interchangeably with the term ‘leakage’ in the literature (Claessens et al, 2015).
The present study further elaborated on how people living with a stoma and stoma care nurses perceive leakage, by having them rate figures with different patterns of effluent as leakage or not. The majority (88-90%) of people living with a stoma perceived faeces or urine outside the baseplate as leakage, as similarly did the stoma care nurses (97-98%) (Figure 2). When faeces covered most of the baseplate, but did not escape outside the baseplate, 83% of the people living with a stoma perceived this as leakage, while among stoma care nurses this was perceived so by 93%. Interestingly, only 57% of the people with a stoma considered urine covering most of the baseplate as leakage, which might be due to difficulties in distinguishing leakage of urine under the baseplate with swelling of the baseplate.
Only 9-19% of the people with a stoma and 30% of the stoma care nurses considered stomal effluent close to the stoma as leakage (Figure 2), either suggesting a low level of concern regarding having effluent on the skin close to the stoma or that there needs to be better awareness of the different types of leakage and in which situations the leakage requires action. Adhesive wafers are generally developed to absorb moisture from the skin (eg, sweat and leakage), and thereby remove excess moisture from the skin. Minor amounts of effluent may therefore not necessarily be problematic for the skin. However, if effluent is located on the skin (underneath the baseplate) close to the stoma, and is not only within the adhesive, skin exposure may still be problematic for PSC development. Why users do not necessarily find it problematic to have effluent on the skin close to the stoma is not known. It may be because the effluent is not at immediate risk of coming on to clothes, because users find it unavoidable, or because they do not know the impact it may have in PSC development.
It is therefore important to educate people living with a stoma and stoma care nurses that leakage of effluent on to the skin, even if it is observed only on a smaller part of the baseplate close to the stoma, may have secondary consequences, such as development of ICD (Burch et al, 2021).
Development of PSCs in general has a negative impact on the quality of life for people living with a stoma (Erwin-Toth et al, 2012; Nichols 2018; Nichols et al, 2019; Nybaek et al, 2010; Pittman et al, 2008). Besides having negative emotional impact for the individual, those with PSCs are more likely to be readmitted to hospital, have increased length of stay in hospital after readmission and have an increased use of supporting products, leading to higher total healthcare costs (Martins et al, 2012; Meisner et al, 2012; Taneja et al, 2017; Taneja et al, 2019; Voegeli et al, 2020). Additionally, more than one third of the visits to stoma care nurses are related to PSCs (Jemec and Nybaek, 2008).
Even though ostomy care products have gradually evolved in the past 70 years (Erwin-Toth and Krasner, 2020), leakage and PSCs are still common problems experienced by people living with a stoma (Claessens et al, 2015; Fellows et al, 2021). To alleviate the risk of improper fit of the ostomy solution to the patient, guidelines have recently been published for selection of appropriate ostomy solutions based on individual’s peristomal body profile (Colwell et al, 2019). At the level of the individual, appropriate use of ostomy products is important to minimise the risk of developing PSCs and consultations with a stoma care nurse may help to identify the causes (Porrett et al, 2011).
People living with a stoma recently ranked pouch leak and appliance problems as the most important research priority among nine topics (Hubbard et al, 2017). New solutions are needed that can help people with a stoma identify leakage and/or alleviate the impact from leakage onto the skin, by ensuring that users recognise leakage when it occurs and thereby ensure a timely change of the pouching system and hence removal of effluent from the skin.
Limitations
The survey was sent out to many countries, which gives a good representation of the global population in ostomy care. However, this also means that national differences in stoma care could influence the results. The present study did not investigate national differences further. However, country-specific differences in stoma care standards and the impact of these on perceptions could be of interest for future analysis.
When conducting survey research it is always important to consider the type of people who freely participate. Therefore it could be theorised that this research is not representative of all people living with a stoma, but rather those with the time and energy to take part.
The research was conducted online only for people with a stoma, which means that those who are not comfortable with using online media were not represented in the survey.
Conclusion
The study revealed that effluent reaching outside the baseplate is generally perceived as leakage, whereas effluent present next to the stoma is generally not perceived as leakage, by both people living with a stoma and stoma care nurses. The consequences of stoma effluent leakage may be both psychological and physical. The psychological aspects, such as embarrassment following leakage on to clothes, may be more apparent to patients, whereas the link to PSCs may be less obvious to patients. More education about what ‘leakage’ is and the consequences that it can have for peristomal skin health is needed for people living with a stoma and stoma care nurses.
KEY POINTS
- Most people living with a stoma and stoma care nurses did not perceive effluent close to the stoma as leakage
- Effluent on the baseplate close to the stoma was frequently reported
- Body profile, stoma appearance and incorrect product usage were often considered by stoma care nurses as the reasons for leakage
- In the majority of cases, multiple interactions between stoma care nurses and patients were needed to resolve leakage issues
- Stoma care nurses often advised patients having problems with leakage to use supporting products
CPD reflective questions
- Which aspects of stoma effluent leakage onto the baseplate do you teach users living with a stoma to understand?
- How do you perceive stoma effluent leakage onto skin close to the stoma? Is it problematic and if, yes, how do you train users to understand this?
- Why do you think that more people with urostomy compared with faecal stomas do not perceive urine underneath the baseplate as leakage?
- What can you do in daily practice to help identify those users who may have leakage and skin issues and who are not aware of their interrelation?


