In 1978, St Mark's Hospital published the outcomes of pioneering restorative surgery for patients with ulcerative colitis (UC) requiring proctectomy who did not desire permanent ileostomy (Parks and Nicholls, 1978). Restorative proctocolectomy (RPC) involves the removal of the colon and rectum, and subsequently the formation of a reservoir (pouch) fashioned from the last part of the small intestine (Figure 1). The pouch is then joined on to the anus and a temporary loop ileostomy usually fashioned above the pouch. If an ileostomy is required, this is reversed in a separate operation.
RPC may be carried out in one, two or three stages. It has evolved in high-volume centres, with experienced teams, as a modified two-stage operation, that is, without loop ileostomy. RPC is also suitable for selected people with colitis-associated neoplasia, familial adenomatous polyposis, colorectal cancer requiring proctectomy and indeterminate colitis (Nicholls and Williams, 2002).
Bowel function is not the same in people with a pouch as in those with a healthy rectum and colon. It is common for patients to experience a high pouch frequency in the first few weeks following stoma reversal, approximately 10–15 times in 24 hours, with some seepage and possibly a degree of urgency or incontinence. A low-fibre diet and anti-diarrhoeal medications may help to reduce frequency while the ileoanal pouch adapts. Pouch frequency usually reduces to 6–8 times in 24 hours, with some people needing to evacuate their pouch once at night, (Michelassi et al, 2003) but this may vary depending on pouch configuration or reason for RPC. Cherem-Alves et al (2021) suggest that most people do not experience major restrictions to their lifestyle after RPC and often report an acceptable quality of life (QoL).
In the authors' clinical experience, most pouch patients report varied levels of support after stoma reversal and commonly feel they lack confidence or knowledge in differentiating between normal and abnormal pouch function with a new pouch. This is particularly the case in areas where patients are operated on in low-volume centres and may not have access to experienced pouch nurses, medical teams or GPs. In many cases, patients resort to self-care, while others source information and learn coping strategies from other people with pouches or through interaction with local and national support groups.
In the literature, there appears to be a lack of structured follow-up, protocols or guidance on surveillance for pouch patients (Winslow, 2006; Samaan et al, 2019) and, where it does exist, it is often variable, not easily available or accessible (Perrin, 2005; Perry-Woodford and McLaughlin, 2008). Few studies detail the advanced roles of pouch nurses in immediate or long-term pouch surveillance.
Data collection
Between January 2014 and January 2020, selected (low-risk) pouch patients were reviewed in a nurse-led clinic following stoma reversal. Patients were followed up at regular intervals postoperatively—at 6 weeks, 3 months, 6 months and 12 months—before being discharged. Ethical approval was considered but not deemed necessary for this service review. The low-risk inclusion criteria stipulated patients had a background of UC, had not experienced major perioperative complications, were deemed safe for nurse-led follow-up by their consultant surgeon and had verbally agreed to nurse-led follow-up.
A protocol was designed by the pouch nurses and agreed by the consultant body. The protocol incorporated: the use of a two-page questionnaire to gather QoL and pouch function data; and a postoperative clinical review to check the wound at the closure site, offer physical, emotional and lifestyle advice and, if deemed necessary, assess the integrity of the pouch anal anastomosis by digital examination.
QoL was assessed through face-to-face or telephone application of two questionnaires, the Cleveland Global Quality of Life (CGQL) and the Pouch Functional Score (PFS). The CGQL is a short questionnaire rating quality of life, health and energy levels between 1 and 10, and has been validated in patients with ulcerative colitis undergoing RPC (Kiran et al, 2003). The PFS scores data on pouch function related to ‘symptoms’ and ‘impact on personal life’. Symptoms are described by stool frequency in a 24-hour period, presence of nocturnal stool frequency, urgency, minor/major incontinence as well as the use of anti-diarrhoeal medications and antibiotics (Lovegrove et al, 2010). Impact on personal life data is collated by ‘yes’ or ‘no’ answers and free text replies to questions related to restrictions surrounding work, dietary, social or sexual activities. These are all accepted tools in the literature commonly used to collect QoL data following RPC (Chandrasinghe et al, 2020).
Between June and August 2020, all patients who had completed 12 months of follow-up were contacted to request personal email details and verbal consent for participation in a patient satisfaction survey, as part of the validation process. An online questionnaire was created via an external platform and responses anonymised.
The data collected from the survey concerned patients' satisfaction regarding issues such as the time between each follow-up appointment, the time required to complete the questionnaires during the appointment, the quality of advice provided during the consultation, preferences for type of consultation and data collection (face-to-face, telephone and email) and the need for further follow-up.
The aim of these interventions was to validate surveillance for pouch patients following stoma reversal, update current nurse-led follow-up, to improve service delivery using an agreed patient pathway, reduce unwarranted variation in follow-up and discharge criteria and, if possible, reduce the outpatient burden on consultant-led clinics.
Findings
The findings have been presented in two sections: the first reports the CGQL and PFS data gathered from the nurse-led clinics; the second covers the outcome of the patient satisfaction survey.
Nurse-led clinic findings
A total of 96 pouch patients completed 12 months of nurse-led follow-up. However, only 56 (58%) completed all four follow-up appointments and were, therefore, included in the analysis. Of these, 42 (75%) were men and 14 (25%) women, with an average age of 39 years when the pouch was created.
The CGQL scores demonstrated a trajectory of improvement in patients' perception of QoL, quality of health and energy levels over time, with each domain improving steadily over time. Energy levels appeared to be the lowest domain immediately following stoma reversal (Figure 2).
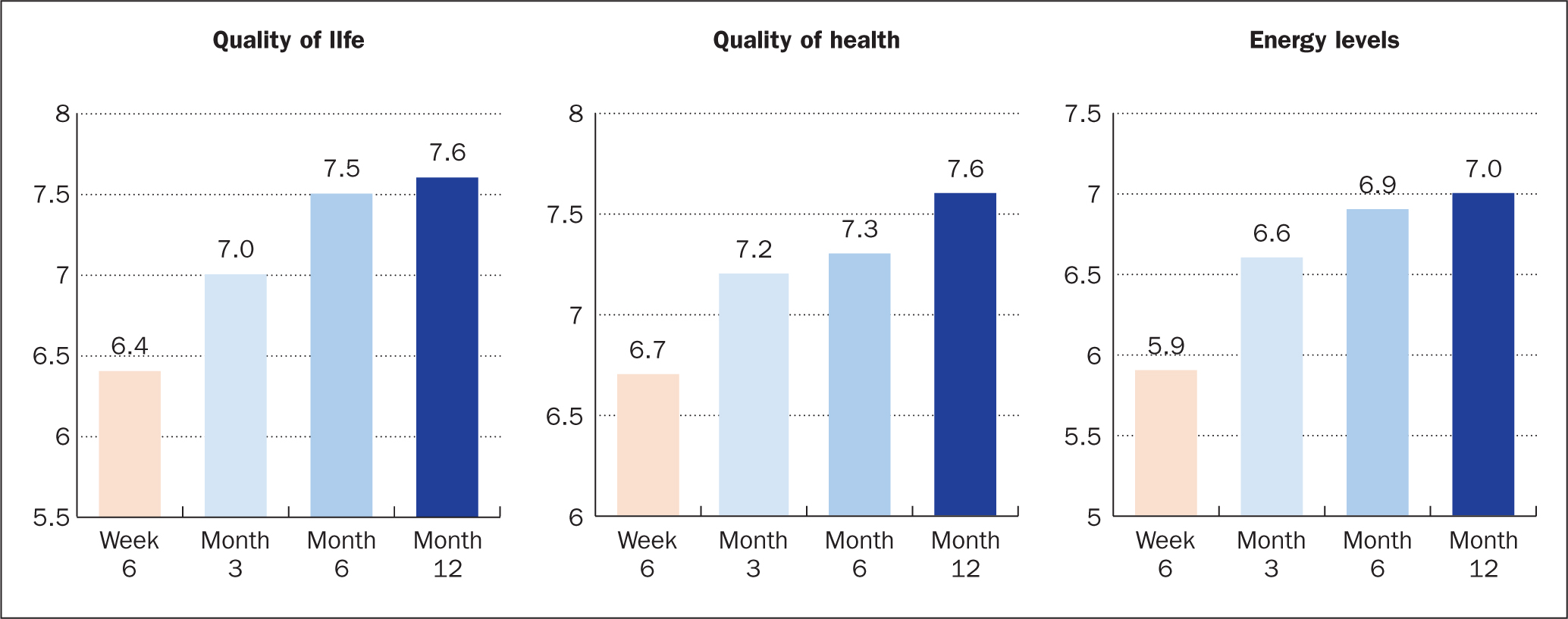
The PFS also demonstrated an overall improvement over time for both symptoms and impact on personal life.
Symptoms
Pouch frequency in a 24-hour period was highest during the first 3 months but reduced consistently over time. At 6 weeks, 25 patients (45%) evacuated the pouch nine times or more within 24 hours, reducing to 13 (23%) at 12 months. At 6 months, 28 patients (50%) evacuated the pouch 6–8 times within 24 hours, which is within the range of expected frequency documented in the literature (Carmon et al, 2003; Kulkarni and Shen, 2019).
Nocturnal evacuation decreased over time, with 34 patients (61%) getting up to empty the pouch two or more times at night at 6 weeks and 20 (36%) still doing so at 12 months. Urgency was highlighted as a problem by almost half of the patients initially but this consistently reduced as time progressed.
At 12 months, major incontinence was not present for most patients (41; 73%). In the two patients (3%) who stated ‘always’ in their initial response, neither had experienced a significant improvement at 12 months. Minor incontinence was selected as ‘never’ by half of all patients; however, for patients who experienced minor incontinence in either the day or at night, incidences of minor incontinence slightly increased over time before gradually reducing at 12 months.
At 6 weeks, most patients (34; 61%) used anti-diarrhoeal medication (loperamide) to manage pouch frequency; this increased to 43 patients (77%) at 12 months.
The use of antibiotics was not consistent and fluctuated over time. However, at each follow-up interval, at least 45 (80%) of the patients were not using antibiotics. In patients who did use antibiotics, these were prescribed mainly for suspected pouchitis, followed by non-pouch-related problems.
Impact on personal life
Social and work restrictions appeared to be a problem for approximately half of the patients but gradually reduced as time progressed. Both social and work restrictions had increased slightly between 6 and 12 months but were not as limiting as documented at 6 weeks.
Dietary restrictions were a main problem for the majority of patients (40; 71%) at 6 weeks postoperatively but were much less restrictive at 12 months.
Sexual restrictions were not apparent for the majority of patients (41; 73%) at 6 weeks but findings showed there were more sexual restrictions at 12 months than at 6 months. One patient said she was trying to get pregnant and reported a successful pregnancy at 12 months following stoma reversal.
Patient satisfaction survey
All 56 patients who completed 12 months' nurse-led follow-up were invited to offer feedback for the service development audit, with 51 patients (91%) agreeing to take part in the survey. However, only 35 patients (69%) completed the survey, of whom 33 (94%) still had their pouch in situ and two (6%) had reverted to an ileostomy following excision of their pouch.
The majority of participants (29; 83%) felt that the time between each follow-up appointment was satisfactory, while six (17%) were somewhat satisfied. A total of 33 (94%) were happy with the time needed to complete the CGQL and PFS questionnaires during their appointment, with two patients (6%) stating that it took longer than they expected. Nearly half of the participants (15; 43%) stated that they were happy with the way follow-up consultations were conducted, but seven (20%) said they wanted to have only face-to-face consultations, one (3%) requested a telephone consultation, while 12 (34%) would have preferred a combination of interactions.
Overall, 34 patients (97%) were satisfied with the clinical advice provided by the pouch nurses but one patient (3%) found the advice was not so useful. Additionally, 27 patients (77%) felt they were offered satisfactory solutions to their problems during their follow-up consultations, three patients (9%) did not feel happy with the solutions offered to their problems and five patients (14%) stated ‘other’ reasons, including not having problems, not feeling well informed before surgery regarding complications or follow-up, as well as acknowledging that there were not always solutions to their problems.
Furthermore, 28 patients (90%) felt that they did not require an appointment with their surgical team after seeing the pouch nurses. However, seven (10%) said they would have preferred to see a member of the surgical team, giving reasons such as liking to see their consultant or because of the perceived complex nature of their pouch; in these cases, verbatim quotes by patients demonstrated that such a consultation was then facilitated by the pouch nurses. At the end of the 12-month, nurse-led follow-up, 21 patients (60%) felt confident enough to be discharged and did not feel they needed further follow-up but 14 (40%) felt they would have preferred follow-up consultations to continue.
Limitations
The main limitation of this review was not having the substantial infrastructure (such as clinical rooms and digital technology), time and a robust, specialist nursing workforce to consistently review pouch patients at the stipulated intervals. The initial aim was to review all pouch patients who met the inclusion criteria within 3 years, evaluate the CGQL and PFS data, then perform a patient satisfaction survey.
However, it took 6 years to complete adequate data collection and, by the time the patient satisfaction survey was designed and disseminated, some patients had experienced pouch failure and reverted to an ileostomy. It was also possible that recall may have been difficult for some patients as so much time had elapsed after stoma reversal.
Although the authors recognise that this is not a large patient study, they consider it was a significant cohort with a good response rate given the relatively low numbers of new pouches created nationally.
Another limitation was shifting the culture and attitudes of some patients and health professionals in reshaping nursing roles to meet contemporary healthcare demands. Workforce transformation is essential if traditional roles of consultant-led surveillance for pouch patients are to be undertaken by a nursing workforce and this needs full investment by health providers and engagement from service users.
Clinics led by pouch nurses are run by highly skilled and trained specialist nurses and, during periods of unplanned absence, some clinics were postponed. To mitigate the risk of delayed reviews, consultations were offered via telephone clinics and the questionnaires completed electronically. These interventions greatly improved efficiencies, allowing more patients to complete all four consultations. However, the limitation remains that not all clinical reviews are viable using these methods and not all patients wanted to be followed up remotely.
Analysis and discussion
These findings suggest that, at 12 months following stoma reversal, the majority of patients were experiencing an acceptable QoL, with all aspects of pouch function improving over time. This correlates with the general literature on QoL and pouch function after RPC, though this transition does not appear to be directly correlated with who provided the aftercare (nurse or consultant), the duration of follow-up or if follow-up was even offered (Berndtsson et al, 2007; Tulchinsky et al, 2010; Lorenzo et al, 2016).
Validated CGQL and PFS were used to collect our data yet some patients requested clarification on certain questions before they could complete the questionnaire. Patients were given the opportunity to discuss or expand on their answers during the clinical consultation after data collection. A few patients requested to change their answers after such discussions during the consultation, as they felt they had not interpreted some questions correctly.
The majority of queries were around the definition and interpretation of urgency, nocturnal evacuations and major incontinence. Scarpa et al (2007) say that different questionnaires used for QoL following RPC have different interpretations and this was also noted in one study where patients with a higher education level showed better results in QoL, as well as in functional and social domains (Ross and Van Willigen, 1997). We now aim to ensure all patients are routinely informed preoperatively about how the follow-up will be conducted and explain certain terms before giving patients the questionnaire to improve patient understanding and confidence in their responses.
Wuthrich et al (2009) highlighted that good QoL scores should not be a surrogate for good functional results. QoL after RPC is documented in some studies as normal or indistinguishable from the healthy population (Richards et al, 2001; Heikens et al, 2012) while other studies report QoL comparable to patients with mild UC because of similarities in bowel frequency, complication development, continuous use of medication, ongoing medical investigation and levels of psychological distress (Martin et al, 1998; Scarpa et al, 2004;).
At 12 months after stoma reversal, the authors found similar issues as approximately half of patients report some level of minor incontinence, one-third report more than two nocturnal evacuations and three-quarters of patients still rely on anti-diarrhoeal medication.
Pouch function is, therefore, highly individual and subjective as most patients embark on this extended surgical journey with the primary intention of avoiding a permanent ileostomy. Anecdotal evidence suggests that many patients believe having poor pouch function is preferable to living with an ileostomy. The patient satisfaction survey in this study highlights that, even though some patients acknowledge that there are not always solutions to their problems, they still rate QoL at an acceptable or high value.
Health professionals need to consider individual patients' views on what they deem acceptable. Understanding patients' specific concerns during the first 12 months after stoma reversal can improve their long-term outlook and help manage related psychological distress. Pouch nurses have usually developed good working relationships with their patients over many years before stoma reversal and are in an ideal position to assist patients adapt their lifestyle to maximise pouch function, offer reassurance or diagnose and manage early complications that can otherwise reduce overall QoL.
In most longitudinal studies, high patient satisfaction after RPC appears to be based on positively associated CGQL and PFS data because peri- and postoperative complications have been avoided (Fazio et al, 1995; McLaughlin et al, 2008; Lovegrove et al, 2010; Fialho et al, 2019), with the inclusion criteria being patients who have had stoma reversal over 12 months and are, therefore, more likely to have developed complications or have the ability to distinguish normal and abnormal function. The inclusion criteria in the present study selected patients from 6 weeks after stoma reversal, as there was a paucity of information available on this patient group in the literature. The authors have, therefore, been able to document only the early experience of pouch patients who would have otherwise been routinely discharged from consultant care at their institution.
The authors have also been able to influence how anti-diarrhoeal and antibiotic medication is prescribed after stoma reversal. Historically, pouch patients at their institution were not routinely started on loperamide postoperatively or at hospital discharge but the authors now encourage patients to self-care by titrating loperamide use to their individual pouch function. At 6 weeks, 22 (39%) patients were not taking any loperamide, of whom 12 (55%) evacuated their pouch more than eight times in 24 hours. In comparison, of the 34 (61%) patients who had started taking loperamide within 6 weeks, only 13 (38%) had a pouch frequency of more than eight times in 24 hours. However, it was noted that patients who had a high frequency despite using loperamide were not taking it regularly or were not able to specify the dose, which highlights the need for closer nursing observation and intervention. Very few patients used antibiotics within the 12-month period for pouch-related concerns, which the authors attribute to better nursing advice and early investigation during that time.
Positive patient satisfaction data established that pouch patients are not disadvantaged by nurse-led surveillance. A few patients said they were ‘not happy’ when questioned about the solutions offered during nurse-led consultations. If this was mentioned during a consultation, the pouch nurses escalated the patient's concerns to the consultants for a second opinion, which was supported by verbatim quotes. As the patients' satisfaction survey was anonymous, we could not cross-reference these comments with actual patient notes to detail what areas needed to be improved. However, verbatim reports related to ‘not feeling well-informed prior to surgery regarding complications or follow-up’ and this was subsequently actioned.
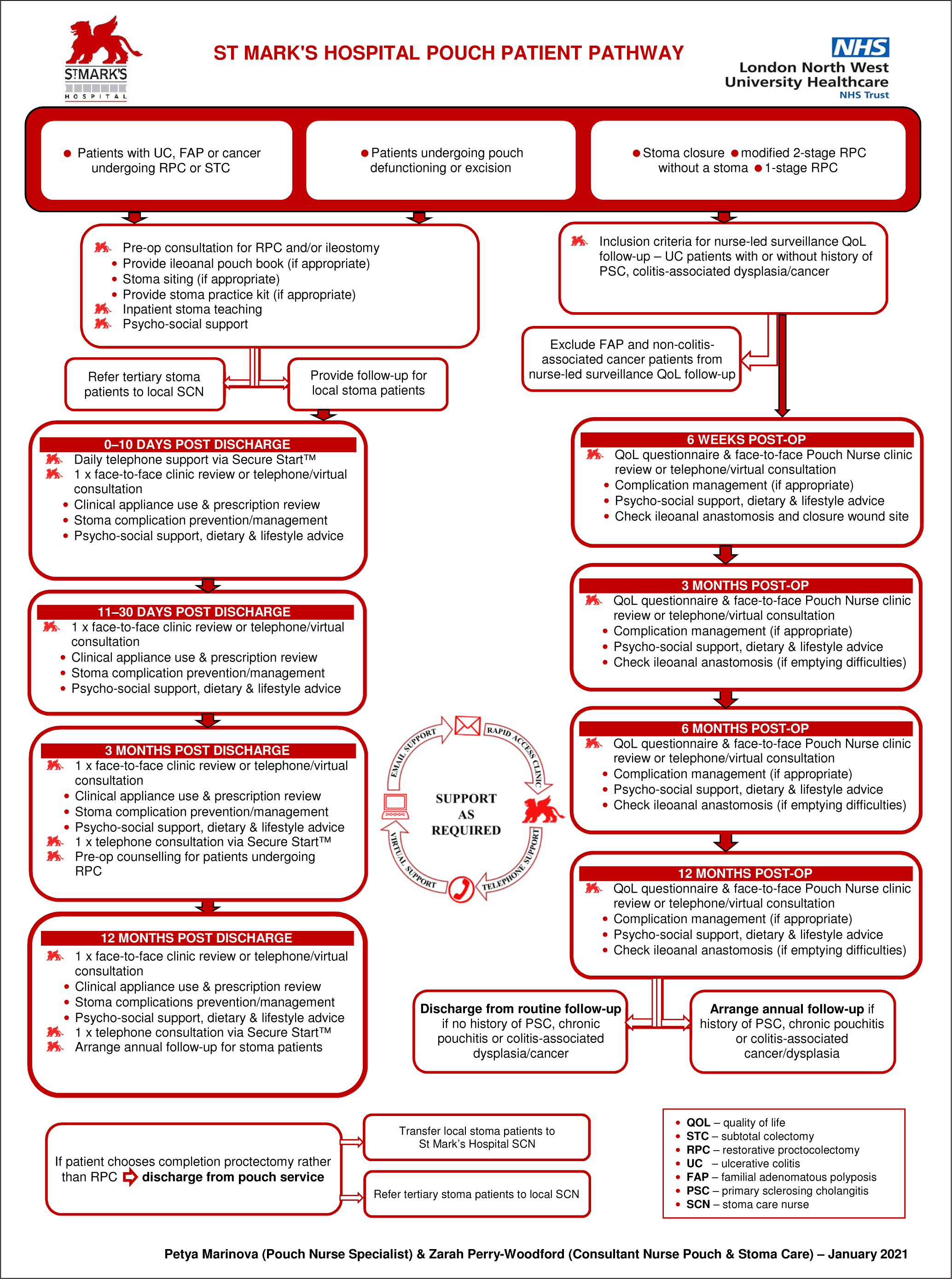
The authors have since incorporated the protocol from this study into their long-term patient surveillance pathway (Figure 3) and disseminated the updated pathway to the consultant body and patients in the preoperative phase.
Although it is well documented that nurse-led care is advantageous across many specialties (Berglund et al, 2015; Jutterström et al, 2016), further research is warranted to compare the outcomes of patients in this study to those who have received only consultant-led care or been lost to routine follow-up, as the authors' patient group had experienced only structured, protocol-based, nurse-led care.
Conclusion
Nurse-led surveillance for pouch patients following stoma reversal can be validated as clinically effective, reduce unwarranted variation in follow-up and is positively associated with acceptable CGQL and PFS data.
Feedback from the patients in this study has shown that a structured follow-up pathway provides vital touchpoints for clinical review, early complication detection and management, and also serves as a record of the milestones they have achieved in a difficult journey to recovery.
However, there remains a requirement for investment and engagement in nurse-led services in order to provide pouch patients with sustainable services while reducing the burden on consultant-led care.
KEY POINTS
- Development, implementation and validation of an agreed patient pathway ensures consistent, evidence-based care is provided to pouch patients immediately following stoma reversal
- Nurse-led care is advantageous to patient recovery, early detection and management of postoperative complications and can reduce the burden on consultant-led outpatient services
- Patient feedback and audit is paramount to validate and shape services compatible with the contemporary changes in healthcare
- Investment and engagement in the nursing workforce is necessary to ensure succession planning for highly skilled pouch nurses and ongoing service development
CPD reflective questions
- Should the NHS invest in nurse-led services for pouch patients if patients report acceptable quality-of-life outcomes, regardless of variations in the care they receive?
- What are the obstacles to establishing an effective surveillance pathway for pouch patients if not affiliated with a high volume or tertiary referral centre?
- Are existing validated questionnaires that are designed to assess patients' quality of life, pouch function or satisfaction levels still appropriate for use in a healthcare system that is radically changing after the impact of a pandemic?


