With the NHS spending about £80 million per year on continence products (NHS England, 2018), it is appropriate to say that continence care in acute settings is part of the everyday protocol. Yet, according to the National Institute for Health and Care Research (Featherstone, 2022), performing this care is often seen in a negative light – even though it is at the heart of person-centred care.
In an acute setting, poor continence care can have a negative outcome for the patient, which includes moisture-associated skin damage, reduced quality of life, risk of infection, risk of pressure damage and even an increased mortality (Percival et al, 2021). When approached inappropriately, continence care can impact the individual affected, the ward team and the hospital itself. Because of this, it has never been more vital to identify the factors that may be preventing the delivery of high-quality continence care and whether some of the solutions could lie in technology.
This article aims to take a balanced view of continence care and to report on the outcomes of a recent trial of continence care technology at the Ysbyty Cwm Cynon (Canon Valley Hospital), NHS Wales, undertaken in conjunction with Cwm Taf Morgannwg University Health Board, to determine if this should be part of the next stage in the evolution of value-based health care in the sector.
Understanding acute hospital pressures
Seen as a low priority in acute care settings (Percival et al, 2021), continence care can easily be misunderstood as being inevitable for patients. However, it is important to remember that incontinence is not something that has to be accepted as unavoidable: we must first understand why it is happening and consider the likely next steps to address the issue. This will include a robust assessment by an appropriate professional and specialist referrals, if required. This should be the first-line solution, with continence containment products seen only as the second-line solution. If these products are considered as a first response, they can become the focus of attention for the wrong reasons and perhaps used inappropriately. This is likely to be less beneficial for patient, and risks the patient developing skin damage (Featherstone et al, 2022).
Understanding the pressures in an acute care setting helps to find answers to better continence care. For example, a lack of knowledge and training can be the reason for poor continence care (Woollerton, 2023) and, once addressed, result in savings for the trust and inspire a positive attitude among colleagues.
One of the pressures experienced across the NHS are staff shortages, with a 10.5% increase in nurse vacancies reported in September 2022 compared with the previous year (Waitzman, 2022). Percival et al (2021) identified staffing pressures and a lack of oversight, as well as routine incontinence product use over an individualised approach, as barriers to the provision of high-quality continence care, highlighting the need for good communication and care planning. This is where a technological solution could assist in relieving some of the pressures brought about through staff shortages.
Acknowledging barriers
Before taking part in the six-week technology trial, nurses on the hospital's long-stay ward at the Ysbyty Cwm Cynon carried out two preliminary anonymised surveys. This was to provide an understanding of ward culture towards continence care and provide a baseline with which to compare the findings from the survey undertaken after the trial. The surveys were able to shed light on potential barriers to change, with the following issues identified as impacting on continence care:
- Culture and ward routines
- Timing and lack of support and resources
- Lack of continued bladder and bowel knowledge refreshment.
The main barrier identified was culture and ward routines. When a patient is admitted to an acute hospital setting, a baseline assessment should take place to ensure the correct bladder and bowel plan for the duration of their stay (All Wales Continence Forum, 2022).
However, the results of the surveys undertaken at Ysbyty Cwm Cynon showed that the majority of patients on the long-stay ward did not have a bladder and bowel plan in place, even though 73% of them had had a bladder and bowel assessment.
This indicated a ‘pad culture’ on the ward where there was routine use of continence pads instead of prescribed products (Northcott et al, 2022), which perhaps explained why 63% of patients experienced pad leakage, as the preliminary surveys found. However, this was not necessarily an indication that the ward staff were delivering inappropriate continence care. For example, all the nurses and health professionals (n=24) interviewed confirmed that the ward followed a four-hour pad-changing routine. Although this is not a personalised care approach, it did show that no patient experienced wearing a soiled pad for longer than they should (Andrews and Butler, 2014).
Can technology support positive continence change in an acute hospital setting?
Taking into account the barriers to effective care identified in the surveys, the hospital and the Bladder and Bowel Health Service within the Cwm Taf Morgannwg University Health Board discussed whether any technology was available that could be used to support better care. The hospital had been approached by Ontex, and the company's product, Orizon SMART, appeared to be the ideal technological solution to trial on the ward.
Orizon SMART is a small rechargeable sensor, which has been in development since 2017 (Figure 1). It attaches discreetly to the front pocket of a smart continence pad and notifies staff when a pad needs changing. The combination of high-quality Orizon SMART products and this technology ensures accurate monitoring of wetness saturation and alerts carers through a simple traffic light system when a product should be changed. One app enables a carer to quickly check the status of all users' smart continence products.
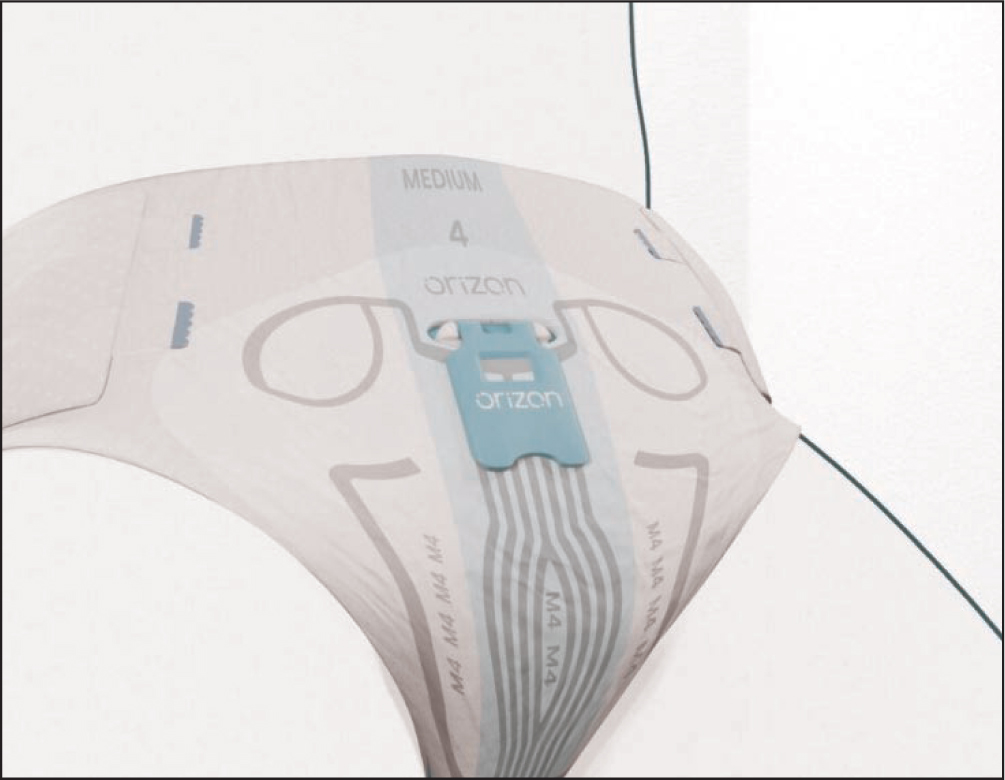
The Orizon SMART has multiple sensor fields, which facilitate the accurate monitoring of urine distribution and body posture information. The data are transmitted via a secure wireless data processing system, which is updated every 60 seconds, providing real-time reporting directly to the hospital, which nurses can view on a smartphone app or a desktop computer (Figure 2).

Although it may seem like a contradiction to say that data collecting can lead to a personalised approach, studies undertaken previously in other European countries by Ontex found this to be the case (details can be obtained by emailing marketing.uk@ontexglobal.com). This is because comparing data can make it easier to spot changes in voiding patterns, which can indicate a change in an individual's continence status. In one trial, in the case of one patient, voiding pattern data led to early detection of prostate cancer.
How Orizon SMART works
Working with nurses and patients at the Ysbyty Cwm Cynon in Mountain Ash, Aberdare, Wales, manufacturer Ontex conducted a six-week trial of the continence status of patients on a long-stay ward. After the initial training period provided by Ontex to nurses and other health professionals on the long-stay ward, the hospital was supported throughout, before final surveys and interviews were completed to analyse the results of the trial. The objective was to improve outcomes by changing the routine continence care culture to achieve more effective individualised patient-centred care. Some of the key benefits noted from the results of the surveys included:
- There were fewer unnecessary pad changes, with the data showing that average 24-hour pad usage dropped from six to 3.2, with no increase in leakage
- Before the trial, nurses saw on average 3.6 pad leakages per shift, 3.4 of which required a change of patients' clothes or bedding. During the entire 6-week Orizon smart trial, two leakages occurred, with 100% of nurses reporting that there had been no need for bedding changes
- According to post-trial survey results, 90% of the nurses involved in the 6-week Orizon trial thought that the smart system improved the overall dignity and wellness of an incontinent patient. They observed that the use of Orizon improved sleep patterns because patients were not routinely disturbed throughout the night for unnecessary pad changes, improving the user's mood and wellbeing.

Feedback provided by the nurses on the use of the Orizon sensor was overwhelmingly positive. Comments included:
‘Overall brilliant pilot and hopefully would be able to use the products in the future.’
Anonymous nurse
‘It has been a positive experience for patients as we are aware of their incontinence without interfering in their rest time or unnecessarily.’
Anonymous nurse
Data leads to a person-centred response
A patient who had been on the long-stay ward for 10 days was agitated, uncomfortable and aggressive. Following the use of Orizon SMART for a few days to monitor his continence, an unusual voiding pattern was noticed in the data collected. This led to a bladder scan, which revealed that, although the patient was voiding, more than 700 ml was being retained in the bladder. Once this had been noted, the patient was catheterised to manage his chronic retention. This resulted in a reduction in aggression and agitation.
Due to the busy nature of a ward, voiding patterns can go undetected for some time. The use of technology supports the comparison of data on the ward, highlighting an issue, such as the one described above, much earlier, leading to a better patient outcome.
Typical comments from the nurses included:
‘Many benefits, mainly providing patient dignity and not having to interfere with the patient's space …’
Staff nurse
‘Obviously, it's a good idea … in the long run, we'd probably see it right across the board and it would be good, especially with patients who are agitated [as it leads to them being] less distressed … it has highlighted how often we had been changing pads.’
Staff nurse
‘I think the trial has gone quite well … it has come down on laundry costs, pad costs and it's also given patients, most importantly, [the ability to] sleep at night as well … Feedback from staff is that it just saves them time and gives the patient more quality of sleep …’
Bladder and bowel specialist nurse
Discussion
Approaching continence care and change in an acute setting is challenging due to several factors, including fear of change. For example, when introducing Orizon SMART to the ward, 70% of the nurses were nervous about using innovative technology as part of care. However, with the correct support, these barriers can be overcome – as shown in the after-trial results, which showed that 100% of the nurses and health professionals surveyed (n=24) would continue to use Orizon SMART.
The overall objective of this trial was to identify whether technology could support a positive continence care culture change. Before the trial, each patient was being changed on a 4-hour routine disregarding of need, while during the trial, 87.5% of participants (n=24) changed products based on need, informed by the app instead of routine. Ultimately, the findings of the trial showed that technology can be used to promote positive change, reminding nurses on the ward about best practice and helping to break pad culture as part of a values-based healthcare approach.
As a side benefit, due to Orizon SMART supporting virtual checks, it was estimated that each staff member saved an average of 28 minutes per shift. Anecdotally, the Bladder and Bowel Service and Ontex were told that this had freed staff, leaving time for quality interactions with patients.
Overall, this meant that the trial ward was able to save 32.7 hours per week that had previously been spent undertaking ineffective continence tasks; using the Orizon SMART system left nurses with substantially more time to carry out other tasks, caring for patients was less of a physical burden, and the nurses reported improved job satisfaction.
In conclusion, acknowledging the pressures in an acute setting, and in a world where there is never enough time anymore, technology is an effective partner, which help ensure that the wellbeing of patients remains at the forefront of delivering care.
KEY POINTS
- Continence care is an important part of the everyday care protocol, yet it can be seen in a negative light, despite being at the heart of person-centred care
- With increasing pressures for health professionals, technology could provide a supportive solution as the next stage of evolution of value-based health care
- Using continence care technology, such as Orizon SMART, can reduce continence containment product leakages and, subsequently, wet clothing and beds, through accurate monitoring of urine distribution
CPD reflective questions
- Do patients in your workplace receive a holistic and thorough continence assessment? Consider how often a patient should be reassessed
- Are individuals experiencing frequent pad leakages and has this been investigated? Why do you think that this is occurring and what would be the appropriate steps to rectify this?
- Are patients having their products changed as part of ‘pad culture’ or routine on the ward? Think about how this culture could be improved or changed


