The endocrine system comprises several distinct glands and tissues, which are made up of specialised cells that synthesise, store, and secrete hormones. Hormones are chemical messengers that can act on nearby cells via interstitial fluid (paracrine effect), on the cell of origin (autocrine effect), at a distant site (endocrine or exocrine effects), or as neurotransmitters (Knight, 2021). Neurotransmitters across synapses contribute to the rapid actions of the nervous system. In contrast, endocrine effects tend to be slow to develop and result in prolonged responses potentially lasting weeks, as hormones travel in the bloodstream from an endocrine gland to another organ. Hormones control a wide range of physiological processes, including growth, metabolism, sleep, immune system response, ‘fight or flight’, reproduction, mood, and behaviour (Kumar and Clark, 2017). They also assist in maintaining homeostasis (a state of physiological equilibrium) by regulating the body's internal environment in response to changes in the external environment. The human body produces more than 100 hormones to carry out these processes, and research is continuing to further our understanding of their functions and interactions as well as identifying more hormones (Knight, 2021).
Endocrine and exocrine glands
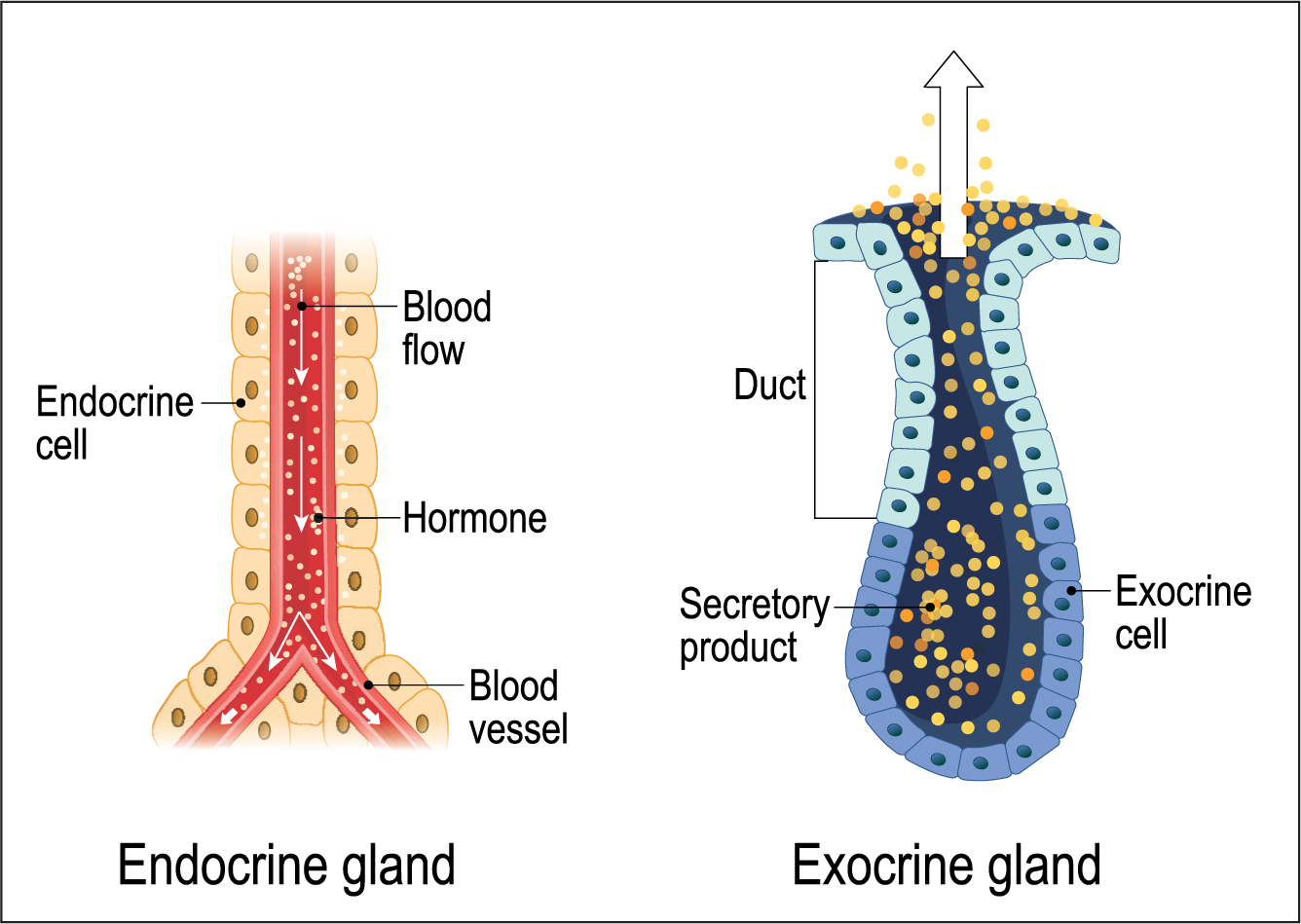
All glandular tissues produce secretions. Exocrine glands are arranged so they secrete theirs via a central duct, which directs the secretions (hormones) to the desired location, for example sweat from glands in the skin (Khan et al, 2022). In contrast, endocrine glands release their secretions into the bloodstream, as part of their primary function. Therefore, endocrine glands have a rich blood supply to ensure efficient transport of their hormones around the body and enable them to continuously monitor blood for changes that initiate hormone secretion (Fox et al, 2015) (Figure 1).
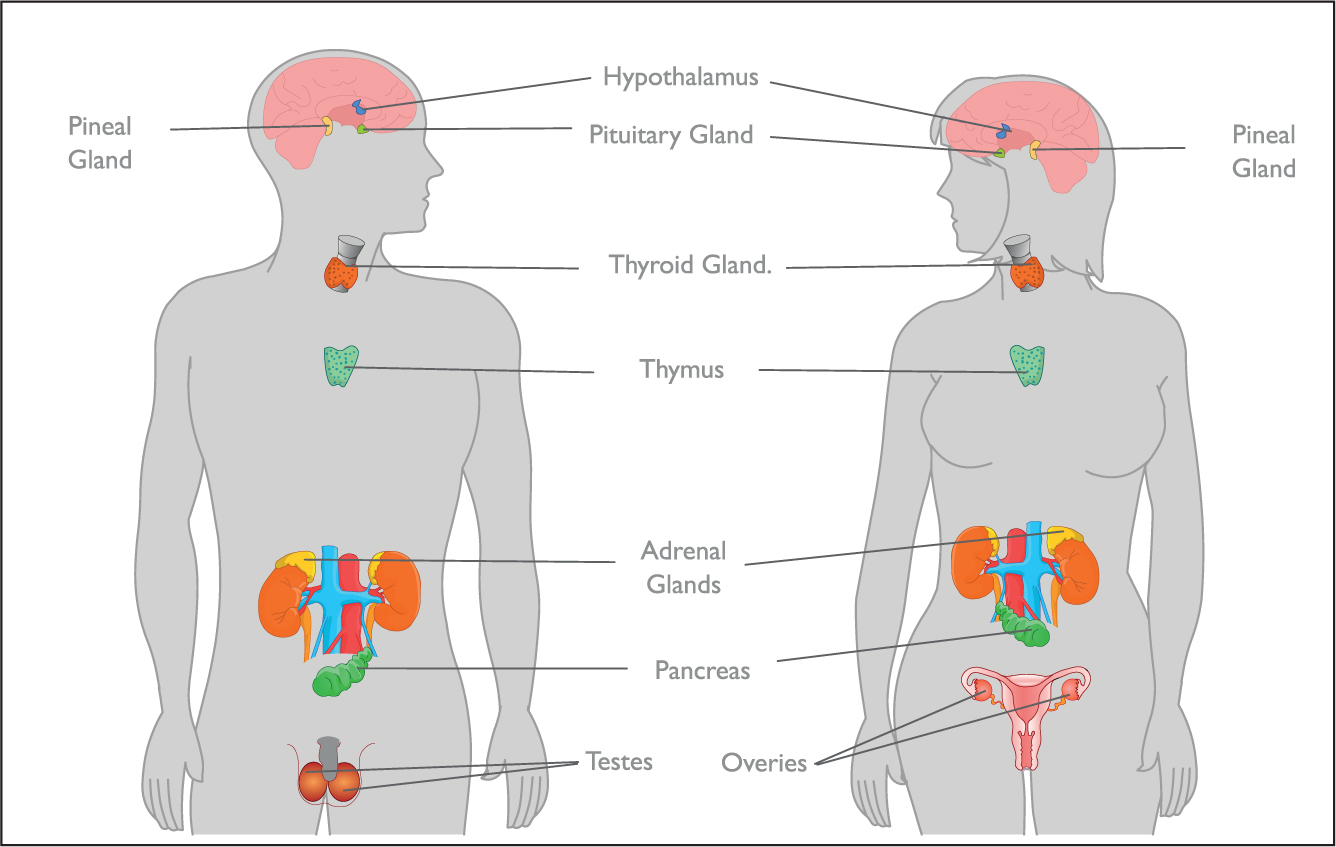
The hypothalamus is a part of the brain that releases several hormones, which affects other endocrine glands' hormone production, acting as the endocrine control centre and linking the nervous system with the endocrine system (Fox et al, 2015). This is connected to the pituitary gland, which produces hormones controlling growth, metabolism, and sexual development. The pineal gland is also located in the brain and produces melatonin, which affects wakefulness (Tan et al, 2018).
Outside of the brain there is the thyroid gland, which sets the body's metabolic rate, the parathyroid glands, which control the absorption and excretion of calcium and phosphate, and the thymus gland, which releases thymosin, stimulating the production of immune T cells (Fox et al, 2015). The adrenal glands, located on top of each kidney, control blood pressure, fluid and electrolyte balance, and the body's response to physiological and psychological stress (Andrade et al, 2021). The endocrine glands of the pancreas secrete insulin and glucagon, which together regulate blood glucose concentration. Reproductive glands (testes in males and ovaries in females) release sex hormones that enable reproduction and sexual maturation (Figure 2). In addition, the intestine and adipose tissue also secrete hormones as part of their primary function, although these are not major endocrine glands. Other organs, such as the liver, kidney, heart, and skin all have secondary endocrine functions (Fox et al, 2015).
Hormone signalling pathways
Hormones are grouped into three chemical classes: peptides, amines, and lipids (mainly steroids) and are synthesised by endocrine glands cells before being stored in preparation for rapid secretion as required (Fox et al, 2015). On release they are transported through the body in the blood, where they then employ their desired physiological effects by binding to specific receptors on the outer membrane or within their target cells. Intracellular binding directly affects the cell's gene expression, whereas extracellular binding changes the cell's metabolism through cascade reactions. Many medications have been created to target these receptor sites by imitating a hormone's action (for example, people with hypothyroidism can be given levothyroxine to mimic the thyroxine they are lacking), or by acting as a competitive antagonist, blocking target receptors to prevent the hormone from binding and employing its effect (for example, beta blockers can be used to treat the adrenaline-related symptoms of hyperthyroidism) (Knight, 2021). Once used, hormones are then released from the target cells either unchanged or inactivated and transported to the liver or kidneys to be broken down and excreted as bile or urine, respectively.
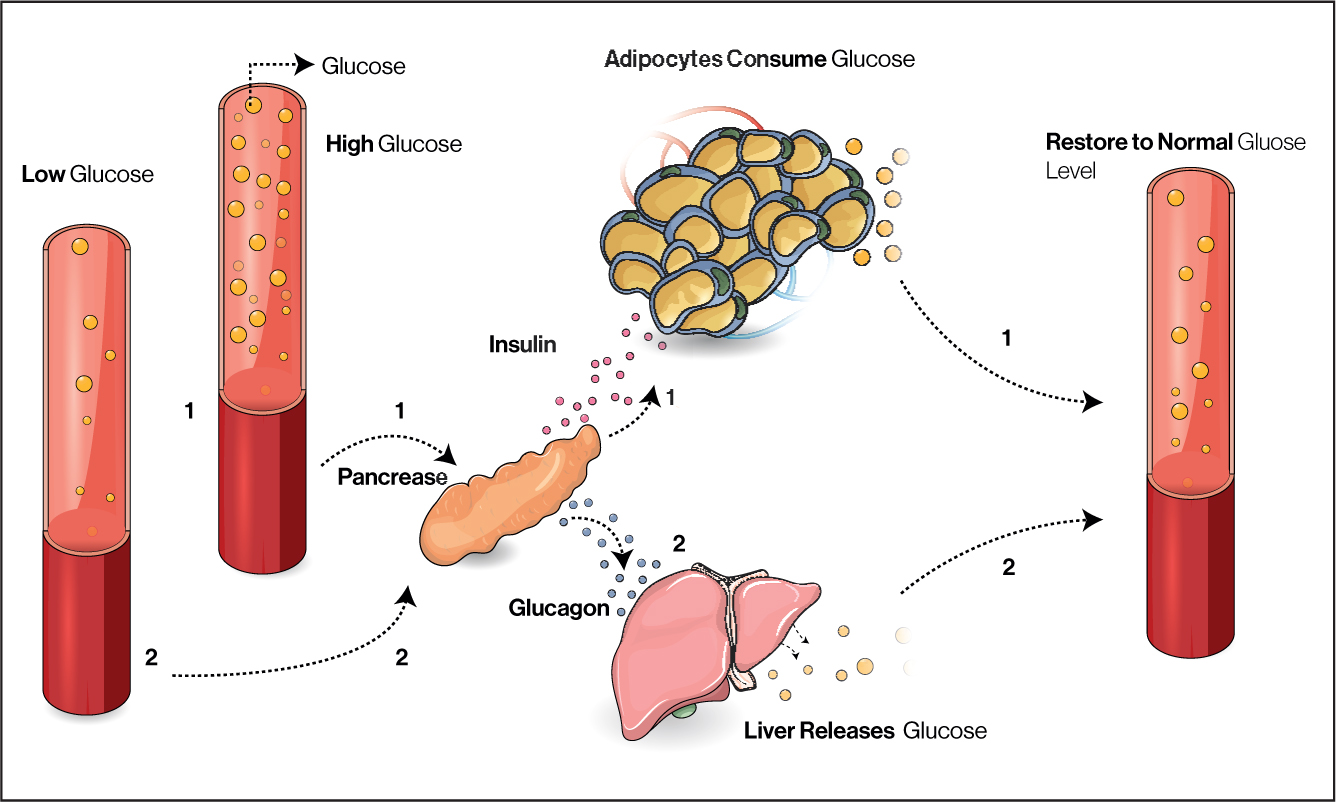
Hormone production is controlled with feedback loops. Most often these involve negative feedback mechanisms, where the effects of a hormone inhibit its release to maintain homeostasis, such as the mechanisms involved in blood glucose regulation (Figure 3). Hypoglycaemia and hyperglycaemia in diabetes mellitus demonstrate deviation from a normal range (in this case blood sugar), which can can be symptomatic and contribute to more severe pathology. In positive feedback mechanisms a hormone's effects stimulate its secretion, for example, in childbirth oxytocin is released, stimulating uterine contractions and pushing the baby towards the cervix, which stimulates the release of more oxytocin (Walter et al, 2021).
Aetiology of endocrine disorders
Disturbance at any point in these complex processes or development of these glands can result in disease. Endocrine disorders largely result from too much or too little hormone secretion. This hormonal imbalance may be due to a problem with the endocrine feedback system, genetic disorder, infection, injury or disease of the endocrine gland, or the growth of nodules or tumours in the glands (Kumar and Clark, 2017). For example, in Cushing's disease the negative feedback loop is disturbed so pituitary hormone ACTH production may become excessive as it is not inhibited by excessive cortisol, resulting in symptoms such as central obesity and high blood pressure. Ageing also lessens the endocrine system's functioning, as the secretion of several hormones is reduced, along with target cells sensitivity to the hormones produced. Examples include falling oestrogen levels triggering menopause, decreasing growth hormone causing loss of muscle mass, declining melatonin levels disturbing sleep, and insulin sensitivity reducing, which increases the risk of diabetes—although these changes fluctuate significantly between individuals (van den Beld et al, 2018). Children are also at risk of endocrine disorders, most commonly thyroidal dysfunctions, diabetes, cryptorchidism, precocious puberty, and pancreatic and thyroid cancers (World Health Organization (WHO), 2012).
Diagnosis of endocrine disorders is based on signs and symptoms, physical examination, medical history, imaging tests to detect tumours, and blood and urine analysis to determine the levels of hormone within them. Once diagnosed treatment can be targeted to the specific disorder and individual, managing their symptoms and maintaining homeostasis with medications, surgery, chemotherapy, or radiation therapy as required (Knight, 2021).
Endocrine disorders
Although not exhaustive, Table 1 gives some examples of hormones and disorders for key glands. Table 2 gives an elaboration of the cause and signs and symptoms for a disorder for each gland.
Table 1. Glands and their disorders
| Gland | Hormones produced | Disorders |
|---|---|---|
| Hypothalamus |
|
|
| Pituitary gland (anterior) (posterior) |
|
|
|
||
| Thyroid |
|
|
| Parathyroid |
|
|
| Pancreas |
|
|
| Adrenal |
|
|
| Ovary |
|
|
| Testes |
|
|
Table 2. Examples of signs and symptoms of endocrine disorders
| Gland | Disorder | Cause | Signs and symptoms |
|---|---|---|---|
| Hypothalamus | Central diabetes insipidus | Deficiency of AVP, an antidiuretic hormone that acts on receptors in kidney to promote water reabsorption (Arima, 2016) |
|
| Pituitary gland | Acromegaly | Excessive GH production by the anterior pituitary gland. Most commonly due to pituitary adenoma (Caron et al, 2019) |
|
| Thyroid | Grave's disease | Autoimmune disease that causes the thyroid to grow and produce an excess of thyroid hormone (Subekti and Pramono, 2018) |
|
| Parathyroid | Hypoparathyroidism | Inadequate parathyroid hormone production, most commonly due to damage or removal of parathyroid glands during surgery (Norman, 2018) |
|
| Pancreas | Type 1 diabetes mellitus | Autoimmune response damages pancreas cells so they are unable to produce sufficient insulin (Fox et al, 2015) |
|
| Adrenal | Addison's disease | The adrenal glands do not produce enough cortisol (Andrade et al, 2021) |
|
| Ovary | Polycystic ovarian syndrome | The exact cause of is uncertain, although some individuals make extra androgens such as testosterone (Escobar-Morreale, 2018) |
|
| Testes | Kallmann's syndrome | Genetic condition resulting androgen deficiency (Liu and Zhi, 2021) |
|
Hypothyroidism
Thyroid diseases are among the most common of the endocrine disorders and can affect people of all ages. The most common of these disorders is hypothyroidism, where the thyroid gland is underactive, resulting in a deficiency of T3 and T4 in the bloodstream (Knight et al, 2021). Hypothyroidism caused by diseases of the thyroid gland, such as infection, inflammation, or deficiency, is known as primary hypothyroidism and is more likely to affect women. When hypothyroidism results from pituitary or hypothalamic disorders, including benign or malignant growths or following head trauma, it is known as secondary hypothyroidism (Taylor et al, 2018). Autoimmune thyroiditis is the most common cause of primary hypothyroidism in high-income countries, but iodine deficiency remains a major cause in many parts of the world (Knight et al, 2021). Iodine is also vital during pregnancy as thyroid hormones are essential for neurological development and the foetus relies entirely on maternal thyroid hormones until about 14 weeks' gestation when it begins to produce its own (Taylor et al, 2018). Autoimmune thyroiditis with inflammation of the thyroid (goitre) is called Hashimoto's thyroiditis and occurs when the follicular components of the thyroid gland are progressively destroyed by the patient's own immune system, resulting in reduced secretion of T3 and T4, and a reduced metabolic rate. Most individuals with mild hypothyroidism have non-specific symptoms including tiredness, lethargy, weight gain and depression, all of which are common in the general population. Therefore, diagnosis is confirmed with biochemical tests (Taylor et al, 2018).
Once diagnosed treatment for hypothyroidism usually involves taking the drug levothyroxine, a synthetic form of T4. The dose of levothyroxine is calculated based on body weight, except in the case of people with ischaemic heart disease who are given a lower dose as it can precipitate severe angina (Kumar and Clark, 2017).
Hyperthyroidism
Hyperthyroidism is caused when an overactive thyroid gland excretes excessive amounts of hormones. This affects around 2% of women and 0.2% of men, with the incidence increasing with age in both sexes (National Institute for Health and Care Excellence (NICE), 2019). Graves' disease is the most common form of hyperthyroidism. It is an autoimmune disorder, characterised by the signs and symptoms shown in Table 2, where antibodies are produced that bind to the same receptors as TSH and subsequently increase metabolic rate, raising the body's core temperature, which leads to increased sweating and weight loss (Knight et al, 2021). Graves' disease can also cause a build-up of inflamed, fibrous, fatty tissue behind the eyes, causing them to bulge.
Risk factors for Graves' disease include smoking and being female (Wémeau et al, 2021). Hyperthyroidism can be treated using anti-thyroid drugs or radioactive iodine (radioiodine) therapy that works by damaging and killing some of the follicular cells that secrete hormones, although this is not suitable for pregnant or breastfeeding women (Subekti and Pramono, 2018)
Case study
Presentation
Ms Singh is 56 years old and attends her GP after a week of severe itching (pruritus) and noticing thick white vaginal discharge.
Initial interpretation
Sexually transmitted diseases should be considered as a potential cause of vaginal discharge. However, in a woman over 50 years old, thrush (Candida albicans) is the most common cause (Al Halteet et al, 2020).
History
Ms Singh had two previous episodes of thrush in the past few months, which she self-medicated with over-the-counter antifungal pessaries from the pharmacy. These temporarily improved her symptoms, which then reoccurred a few weeks later. She is finding the itching bothersome and was wondering if anything else can be prescribed to clear up the infection for good.
Her husband has no symptoms, and she has had no new sexual contacts in the last 30 years. In the past year she has been feeling increasingly tired and has put on 12 kg. Her older brother was diagnosed with diabetes mellitus and recently died following a stroke aged 64 years and her mother has several lower leg ulcers.
Physical examination
Ms Singh is obese with a body mass index (BMI) of 36.4 kg/m2. Her blood pressure is raised at 148/94 mmHg. A sample of her vaginal discharge, which is thick, white, and cottage-cheese like, has been sent for analysis.
Further investigations
Urinalysis identifies the presence of glucose in her urine (glycosuria). A random venous blood glucose reading of 12.8 mmol/litre is above normal range, and later her blood test results show her haemoglobin A1c (HbA1c), a marker of long-term glucose levels, is also high at 68 mmol/mmol. Table 3 shows the WHO reference levels for these tests in diabetes diagnosis.
Table 3. World Health Organization criteria for diabetes mellitus diagnosis
| Measurement | Normal result | Result in diabetes |
|---|---|---|
| Random venous plasma glucose concentration (mmol/L) | Variable | ≥ 11.1 |
| Fasting plasma glucose concentration (mmol/L) | ≤ 6 | ≥ 7 |
| Plasma glucose concentration 2 hours after 75 g anhydrous glucose in an oral glucose tolerance test (mmol/L) | ≤ 7.7 | ≥ 11.1 |
| Haemoglobin A1c (mmol/mol) | ≤ 41 | ≥ 48 |
Source: WHO, 2011
Interpretation of findings
Ms Singh has a strong family history of diabetes mellitus. Her obesity and ethnicity are also predisposing factors for type 2 diabetes mellitus (Goff, 2019). These factors alongside her test results lead to Ms Singh being diagnosed with type 2 diabetes. Her high glucose levels in the urine and blood allows yeasts to flourish and accounts for her recurrent episodes of thrush.
Treatment
Initially Ms Singh is given diet and lifestyle education to manage her diabetes, this will be reviewed in a few months to see how effective it has been. Her risk of further episodes of thrush will reduce as she improves her glucose control but, in this instance, she will be prescribed another antifungal pessary.
If her type 2 diabetes worsens or is unsuccessfully managed by diet and lifestyle adjustments, she may then be prescribed medications such as metformin and eventually even insulin (NICE, 2022).
KEY POINTS
- Endocrine glands produce hormones, which maintain homeostasis with feedback loops and control bodily processes
- Hormones travel via the bloodstream and bind with specific receptors to produce their desired effect on target cells
- Endocrine disorders largely result from too much or too little hormone secretion due to disruption in the gland or at any point in the complex feedback pathways
- Medications can be used to mimic hormones or block receptors to attempt to reverse the effects of endocrine disorders


