This article uses a case study and a personal account to highlight how trainee nursing associates (TNAs) and registered nursing associates (RNAs) support patients with complex care needs following a difficult diagnosis such as motor neurone disease, and the impact on the individual's health and wellbeing from a biopsychosocial perspective. The case study was originally presented by a trainee nursing associate during a viva voce assessment. A viva voce, or oral assessment, is one method for summative assessments and often used as part of higher education courses preparing health professionals, enabling students to showcase their knowledge and experience in patient care from a person-centred care perspective (Dobson, 2018). To maintain the reflective nature, the case study is presented here in the first person.
Background
Motor neurone disease (MND) refers to a group of neurological disorders that are progressive in nature causing damage to and destruction of motor neurones – the cells that control skeletal muscle activity such as walking, breathing, speaking, and swallowing (MND Association, 2022). There are various categories, but for the discussion here particular attention will be paid to progressive bulbar palsy, often referred to as progressive bulbar atrophy. This type of MND is a result of damage to upper and lower motor neurones in the brainstem. This is the area that predominately controls muscles used for oral functions such as chewing and swallowing (MND Association, 2022). Over time, symptoms worsen and difficulties arise with chewing, speaking and swallowing. In addition, people with progressive bulbar palsy may experience weakness in the tongue and facial muscles, and a significant reduction in the gag reflex, increasing the risk of choking.
Neurodegenerative disease such as MND is not without its complications, such as aspiration pneumonia – dysphagia can increase such a risk (Oliver, 2019). Therefore, when providing such complex care, this should follow a problem-solving perspective, take a person-centred care approach and consider the patient's best interests – at all times considering scope of practice and maintaining professional boundaries (Nursing and Midwifery Council (NMC), 2018). Although there is no cure for MND, research is working towards better treatment options (MND Association, 2024c). MND is currently high on the political agenda for improved health care, therefore it is important to showcase the significance of care from a multidisciplinary perspective.
Case study
This case study is about a patient in my area of practice, which is an older adult mental health ward. For confidentiality purposes, a pseudonym will be used to protect the patient's identity and she will be referred to as Dawn.
Dawn is age 69 and was admitted to the ward following a suicide attempt. She was slightly underweight with a BMI of 17.9. On admission, we performed physical observations using the National Early Warning Score assessment tool, NEWS2 (Royal College of Physicians, 2017), Dawn scored a NEWS2 of 0.
Therefore, it was decided that in line with local policy these physical observations would be carried out twice a day. In line with the NMC Code, as a TNA or RNA, I can carry out these observations if competent to do so (NMC, 2018).
The suicide attempt followed a diagnosis of MND. The type of MND that Dawn has is progressive bulbar palsy, affecting the upper and lower motor neurones and impacting the oral facial process. Symptoms can impact the tongue, lips, speech and swallowing, ultimately requiring nutritional support.
Dawn had attempted suicide and for her own safety was detained under section two of the Mental Health Act 1983 for assessment, which gave the care team up to 28 days to assess Dawn and start the treatment plan for her. Initially, Dawn was started on a low dose of 50 milligrams of sertraline, a selective serotonin reuptake inhibitor (SSRI) (Joint Formulary Committee, 2025). Serotonin is a hormone that needs to be increased in people with depression and 50 milligrams is the lowest dose according to the British National Formulary (Joint Formulary Committee, 2025). The maximum dose for the patient is 200 milligrams, which is titrated in 50 milligram steps – this can be done weekly. This element of prescribing is beyond my scope of practice, but I acknowledge that I should be aware of when the dose may need to be increased.
The SSRI dose is further considered in our multidisciplinary team meeting on a weekly basis, where we ask how Dawn is feeling then a decision can be made about whether it needs increasing or not. Naturally, there are some side effects: sertraline can affect the gastrointestinal tract – for example, it can cause constipation or diarrhoea – and it can also make patients dizzy and drowsy (Joint Formulary Committee, 2025). This is also something to be mindful of, especially with MND already causing muscle atrophy, as it could increase Dawn's risk of falls and other mobility issues.
Nutrition and associated issues
Dawn's weight was 46 kg and her BMI 17.9, which is considered underweight - her ideal weight would be at least 47.4 kg. A consequence of dysphagia is loss of weight alongside muscle wastage. The dietitian was involved in her care, and provision of supplements was considered to ensure adequate nutrients and prevent malnutrition (Rosenfeld and Ellis, 2008; Coates et al, 2023). Dawn was also offered the option of having supplementary Fortisip Compact (a liquid food supplement) as required where she has not had sufficient dietary intake. Progressive bulbar palsy affects Dawn's mouth, tongue and swallowing, so she has some issues with adequate diet intake and requires a level 5 (minced and moist) diet and thickened fluid. Sometimes, if Dawn is struggling to swallow – for example, if she's tired – then her dietary intake can be impacted. In addition, there could be a risk of aspiration if she were to inhale any food or fluid, which could cause complications such as pneumonia (Oliver, 2019).
For Dawn, privacy is something that is very important and she spends a lot of time in her room. I try to encourage patients to come to a dining room and eat together, but from Dawn's point of view this makes her uncomfortable, because the progressive bulbar palsy gives her paralysis of the mouth, so when she's eating her lips no longer seal and food falls out of her mouth. Dawn uses a flannel to protect her dignity and eating is a very private process for her. The NMC Code (2018) and the Standards of Proficiency (NMC, 2024) emphasise the importance of communication with colleagues. I informed colleagues that I thought it was more important for Dawn that she had the privacy of her own room to eat, than for her to be made to go to a dining room to socialise and eat in front of lots of people.
Dawn has a percutaneous endoscopic gastrostomy (PEG) tube in situ, which is common with people with MND. The decision to insert a PEG tube is usually made quite early on, which means that when she does start to struggle with swallowing, fluid, food or medication can be given through the tube, reducing the risk of aspiration. As part of the nutritional management for some people with MND, feeding through the PEG tube plays a significant role in maintaining adequate nutritional support for those who cannot tolerate food orally as a result of dysphagia, and reducing the risk of aspiration pneumonia. Rosenfield (2009) outlined the problems associated with dysphagia, which ultimately leads to weight loss and increased mortality, and stressed the importance of early intervention with PEG tube feeding to ensure adequate nutrition.
Sertraline can also be dispersed in water and given via the PEG tube; however, the pharmacokinetics of sertraline involves a slow absorption process and the half-life is 4-10 hours following ingestion. Although not widely researched, it has been proposed that a low concentration can lead to a reduced efficacy, whereas increased concentration naturally leads to a risk of toxicity (Huddart et al, 2020). The hospital pharmacists covered the ward area and they would have dispensed the medication, but the prescription was not complicated enough for the pharmacist to be involved directly, given that the doctor and psychologist on the mental health ward were very experienced with the prescribing process for specialist medication.
The Mental Capacity Act (MCA) 2005 is the legal framework to assist health professionals in the assessment of capacity. The overarching principle states that one should assume capacity unless considered otherwise. Dawn has capacity so she can make decisions about eating. If she were having a day where she did not feel like she was eating enough or couldn't swallow then she could choose to have additional nutritional supplements such as Fortisip via the PEG. The aim of such supplements is to ensure adequate nutrients and prevent malnutrition (Rosenfeld and Ellis, 2008). Any diet that the hospital orders in for Dawn will need looking at and she should receive a speech and language therapy referral as part of the multidisciplinary team, just to make sure that the texture/thickness level of diet and fluid is still appropriate.
One of the things that Dawn enjoys is grapefruit. On one occasion where she was not eating much, I went to the shops to buy some things she would eat, and she asked if I could buy some grapefruit juice. It is important to avoid grapefruit when on sertraline, because grapefruit can block the effect of cytochrome P enzymes, which help to break drugs down in the liver, and therefore increase the levels of the drug in the system (Kiani and Imam, 2007). So, as a compromise, I bought some grapefruit soup that she could smell, which she loved.
One of the things that was important to Dawn was a vegetarian diet. I made sure that this was documented and communicated to colleagues.
Communication
The muscle weakness caused by MND has taken away Dawn's ability to speak, therefore she uses an iPad to communicate. She had been diagnosed with MND and was already non-verbal when she came into our care. It was never discussed whether she was ever offered voice or message banking. Dawn's hearing is unaffected so you can speak to her and she will reply on the iPad. I think it is important to give Dawn the time to reply on the iPad without assuming what she's going to say and then speaking on her behalf, and I have discussed this with other team members. Dawn commented on how well I communicated with her – I used my previous experiences with non-verbal patients.
Communication issues arise as a result of damage to neurons in the brain and spinal cord (Paynter et al, 2022). Therefore, having an awareness of individual patients and their preferences is paramount. We put in place a ‘This Is Me’ form, which gives information about Dawn, her diagnosis, what she likes and dislikes, how she communicates and so on, and that has worked very well. On one occasion, I went into Dawn's room, and noticed someone had been writing things on a notepad because they thought that she could not hear – in fact, this notepad was only there to be used by Dawn when her iPad was charging, she had no issues with hearing. I feel it is important to make colleagues aware that Dawn's inability to communicate verbally does not affect the fact that she can hear and has capacity. MND does not tend to affect cognitive ability – the MND Association (2024a) says that it can have a mild effect on thinking and behaviour but only a few people experience severe effects – so although the rest of the body is shutting down, Dawn still very aware in terms of communication and her options.
Cave and Bloch (2021) suggested that 80% of people living with MND experience speech difficulties that impact on overall quality of life, such as loss of identity. High-profile cases, such as Stephen Hawkins and the rugby player Rob Burrow, have further highlighted the advances in computerised technology and artificial intelligence that assist with communication. For example, in some augmentative alternative communication devices, movements of the person's eyes can be used to communicate their words via a computer screen, to be voiced by the system. MND does not affect the ability of the eyes to move. Less desirable aspects of such systems include that a voice synthesiser is often regarded as impersonal in comparison with a person's true voice. Although the majority of people with MND will pursue augmentative alternative communication in some shape or form (Cave and Bloch, 2021), not all choose to pursue voice banking – that is, recording samples of their speech so that a personalised synthetic voice can be created. The main reason given is that it is not close enough to their own personal voice. Dawn did not pursue this, and when she arrived on the ward, she had already lost the use of her voice.
There is a recommended summary plan for emergency care and treatment (ReSPECT) in place for Dawn and the ward has the original, which is essential. The ReSPECT document outlines Dawn's instructions in the event of an emergency (Resuscitation Council UK, 2025). Although not legally binding – clinical judgment must be used if something happened in an emergency – it affected Dawn as she will not be to be able to tell you verbally in any detail what needs to happen, and may not be able to type or write because she could potentially be very unwell.
Motor neurone disease
It was important for me to have an understanding of the pathophysiology of MND, to better assist Dawn with managing the difficulties that the disease process presents. There are several different types of MND. MND affects people in different ways and there is a difference in how quickly each type of MND progresses. They include (National Institute of Neurological Disorders and Stroke, 2025):
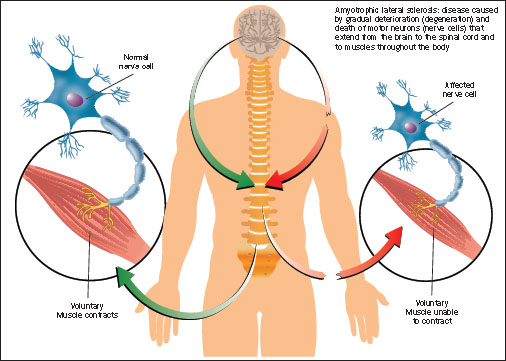
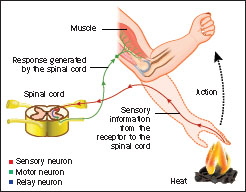
With normal function, neurones are found in the brain, the brain stem and spinal cord and they are responsible for taking messages from the brain down the motor neurone into the muscles, to trigger movement (Figure 1). There is also the reflex arc, as shown in Figure 2. The sensory neurones here are picking up the sense that the finger is burning, that message is transferred to the brain and at the same time a message is relayed through the inter neurones to the motor neurones to quickly move the hand away. For someone with MND, these motor neurones die and are not replaced, which causes muscle atrophy because the muscles are not being used.
For Dawn's particular type of MND, it affected the muscle in her tongue, her lips, her epiglottis and her oesophagus, which are all involved in eating and swallowing. Other types of MND may show signs in the legs or arms first. One of the first symptoms of MND can be the progression of swallowing difficulties, although this was not the case for Dawn.
Incidence
Currently around 5000 people in the UK are living with MND, with approximately a 1 in 300 chance of being diagnosed. There are around six people a day diagnosed and around six people a day die from the condition. As there is currently no cure for MND, the patient experience and the patient care are vital (MND Association, 2024b)
Predisposing factors
The older you get, the more likely you are to have MND (Turner, 2022). Regarding genetics, about one in 10 people may be affected due to a faulty gene (MND Association, 2025a). There is currently limited research on MND, but in 2021 the previous government pledged £50 million pounds of funding for research into MND (Department for Science Innovation and Technology et al, 2023).
An excess of glutamate, a chemical messenger in the motor neurone, has been suggested as a contributor to development of MND (Babu et al, 1998). Possible lifestyle factors that have been proposed also include serving in the military, or professional athletes (Chen et al, 2022; MND Association, 2025b)
Tests/diagnosis
Unfortunately, there is no particular diagnostic test other than history taking and examination for MND – most of the tests are done to rule out other things. Electromyography is used in assessment of nerve cells and surrounding muscle and assists with the diagnosis of the tongue (Turner, 2022). For dysphagia, clinicians might request an MRI scan to rule out a stroke, which is another cause of paralysis, dysplasia and dysarthria. Other tests may include blood tests and lumbar puncture to rule out infection, and possibly a scan of the spine, since if there is any degeneration of the spine that can affect the spinal cord and cause some paralysis (Jones, 2011).
Treatment options
There is one drug for people with the ALS form of MND, called riluzole, which suppresses the glutamate in the motor neurones; however, it can only give about 2 or 3 months extra life expectancy (National Institute for Health and Care Excellence, (NICE), 2001; MND Association, 2024b).
Biopsychosocial aspects and the multidisciplinary team
It is important recognise that somebody with MND is still a person first – they are someone who just happens to have MND. A holistic approach that is person-centred considers the patient's perspective and what can be done to make their life better (Engel, 1981). This includes aids that they can be given to help them with showering, eating, breathing and additional care needs to enhance quality of life. It also considers their wishes with end-of-life care. Unfortunately, with Dawn's diagnosis the prognosis was 6 months to 2 years. A psychologist was involved in her care and met weekly with Dawn at the multi-disciplinary team (MDT) meetings. Occupational therapists were also involved at the MDT meetings and group therapies. They engaged with Dawn on a one-to-one basis with assessments to see what support was needed in addition to assistance with the arts and crafts activities available. Dawn preferred to stay in her room over attending group therapy.
The physiotherapist assessment identified the things that we could assist with on the ward and one of those was for her to walk, but it is a busy ward, and Dawn was quite shy so she would not do that on her own. I would go to her room on my shifts and take her for a walk around. There is a garden, so we went to pick some lavender for us to touch and smell, which had a therapeutic effect, and we were able to communicate using her iPad.
We focused on Dawn's ability to do things rather than what she could not do. The team provided appropriate adaptations to make her as comfortable as possible while she was on the ward and after discharge so that she could live life comfortably with what she has and what time she has left. I made sure the team supported Dawn where it was required but also made sure that she had her own voice and patient choice rather than telling her what to do. Given that she has full capacity, when Dawn was given the time to talk (type) she was able to say what she needed.
It's not unusual for who has been diagnosed with MND to be depressed because of the ever-changing symptoms (Edge et al, 2020). In terms of the attempted suicide, Dawn was a very intelligent person, very aware of how this disease was going to progress and did not really want to see that through to the end. So, while in the care home she had decided that she was going to attempt to take her own life. Given that the ward where I work is a mental health ward for older adults, there are the relevant safety elements in place and risk assessment processes. There are different observation levels, for individuals deemed at a high risk of suicide a level of observation is in place where they are constantly watched or checked every 15 minutes. There is a reduced risk of self-injury by ligature on the ward as it has been adapted to take this into account. Dawn came in to us on the ward as the risk in this environment was reduced compared with that in the care home and the staff are trained to carry out observations.
Dawn's life is changing, financially and mentally. Her condition is also changing the way that she works socially. There may be issues with eating in a social group for people with MND due to the stigma, and also fear of choking caused by loss of control and weak muscles in the neck. The main cause of death in people with MND is respiratory dysfunction (Oliver, 2019) and ultimately the dysphagia eventually leads to end-of-life care. Up to 15% of people with MND develop frontal temporal dementia (Oliver, 2019), although this was not an issue for Dawn. The team on the ward can access information on how best to help Dawn as she progresses through the end of life and pass that on to the care home.
Relevance for future practice
This case study has explored MND from pathophysiological perspective and the problem-solving approach involved in diagnosis. It outlines the care required from a holistic approach that considers aspects of the patient's best interest and biopsychosocial elements, all of which are pertinent to the provision of safe, effective care. The case presented indicates that care for MND is not prescriptive, with reasonable adjustments patient-centred care can facilitate safe effective practice for those with challenging physical aspects of MND (NICE, 2019).
The learnt experience from this case study highlights that person-centred, compassionate care is paramount when caring for patients with such complex needs. The team around the patient, including the TNA or RNA, focuses on building a rapport and professional relationship with patients who are reliant on the health professional to be their advocate when they are rendered non-verbal. The TNA has a pivotal role to play in modern health care for people living with MND.
Modern medicine and technology has placed health professionals in a good position to support patients with such complexities as outlined in this case study. Person-centred compassionate care is paramount alongside scope of practice, knowledge of pertinent legislation such as the MCA 2005 and Mental Health Act and how they guide practice to ensure competence and patient safety. Thus, informed consent and inclusion in decision making, however small, is essential and ultimately impacts patients’ health and wellbeing. This case study illustrates the significance of understanding complexities involved in health conditions both during training and as a future registrant.
Conclusions
Healthcare practitioners can relate and understand the importance of empathy, compassion, privacy and dignity that are crucial at any stage of a person's health deterioration. How to facilitate care within an MDT and maintain professional boundaries, ensuring that individuals are safe and competent to do so, is paramount. Improved knowledge and understanding of complex health conditions ultimately aids continuous professional development and ensures that professionals are better equipped to support the patient's journey throughout the healthcare system and to deliver person-centred care.

