Inside the brain resides a system of reservoirs (ventricles) that house cerebrospinal fluid (CSF). The purpose of CSF is to provide the brain with buoyancy, to act as a protective ‘shock absorber’ and to aid in the distribution and removal of products to cells across the brain. CSF is produced chiefly in the lateral ventricles and flows through the ventricular system and subarachnoid spaces of the spine before being reabsorbed (mainly via the arachnoid granulations of the superior sagittal sinus system) (Figure 1). Hydrocephalus is a condition characterised by excess CSF fluid build-up within the brain, which can be due either to excess production of CSF, obstruction in the usual CSF pathways or blockage of the usual mechanisms that reabsorb CSF. The condition remains difficult to treat, with the major strategy being diversion of CSF away from the brain to relieve excess pressure on the organ. This article presents the case of a child with an inoperable brain tumour and hydrocephalus who was treated in an unusual manner using long-tunnelled external ventricular drains (LTEVDs).
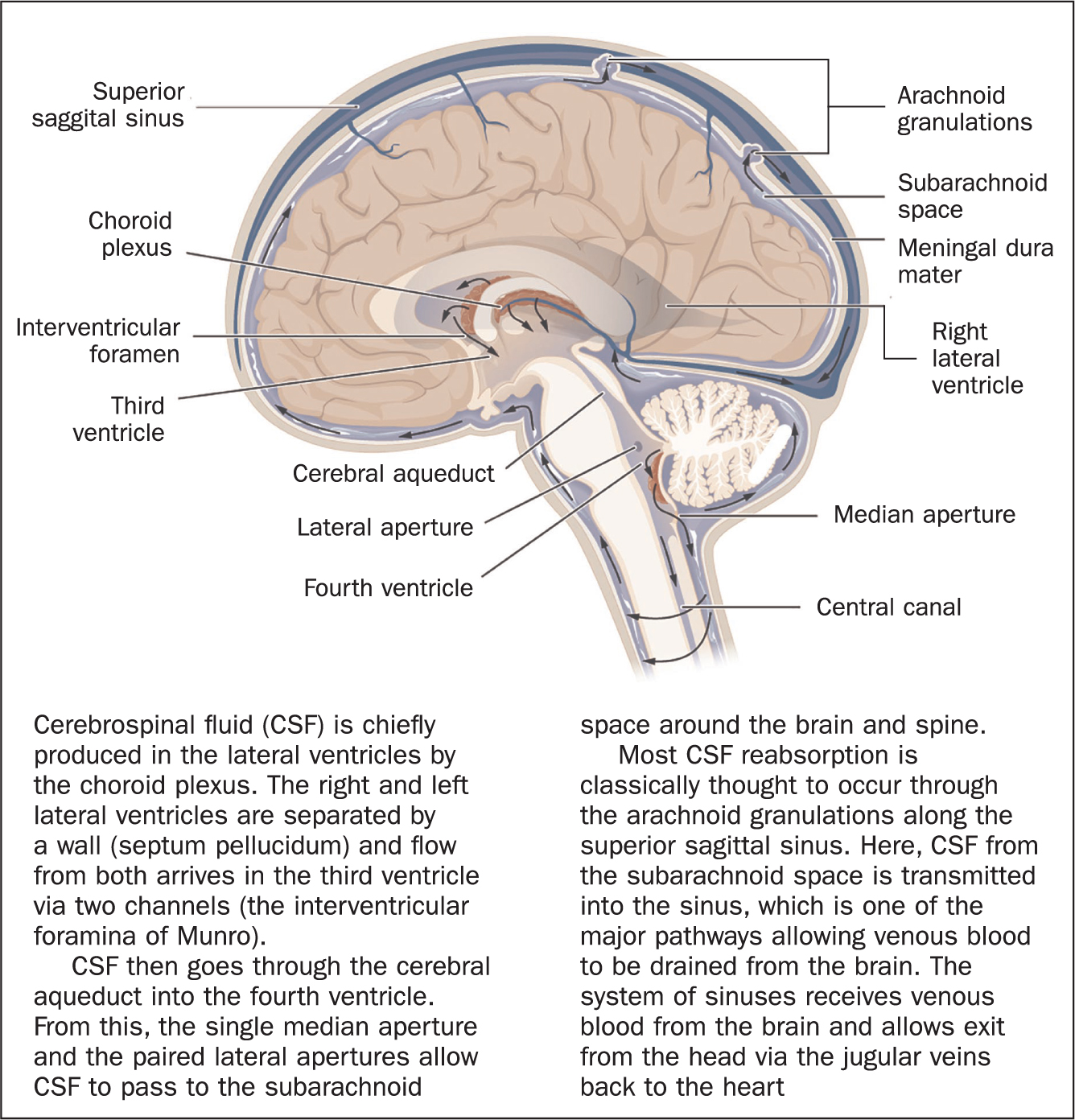 Figure 1. Cross-section of the middle of the brain (sagittal view), illustrating the cerebrospinal fluid (CSF) pathways
Figure 1. Cross-section of the middle of the brain (sagittal view), illustrating the cerebrospinal fluid (CSF) pathways
The ‘normal’ value for intracranial pressure (ICP) in children is not truly known, because much of the data used to generate a hypothesis of ‘normal’ value is based on patients with neurological conditions who undergo monitoring of their pressure. In general, widely accepted values are <5 mmHg in infants, <10 mmHg in older children, with pressures in teenagers reaching those of an adult patient at around 15 mmHg (Wiegand and Richards, 2007). In the context of hydrocephalus, the pressure may be much higher and lead to symptoms.
Children with tumours may develop hydrocephalus due to physical obstruction blocking the natural pathways of CSF around the brain. As fluid collects upstream of the blockage, excess pressure develops within the brain. In infants, this may lead to increasing skull size (occipital frontal circumference) because the sutures of the skull are open and so excess pressure in the brain drives expansion of the skull. The anterior fontanelle closes between 9 and 18 months. When the sutures and fontanelles close, the ability of the skull to expand and compensate for increased ICP is lost and so a child may deteriorate more rapidly. Tumours may also contribute to hydrocephalus because they divide rapidly and may generate increased levels of protein in the CSF, making it more viscous and reducing the capability of the system to reabsorb CSF.
In infants, as the head enlarges, notable features when examining the patient include fullness of the fontanelle, splaying of the cranial sutures, distended scalp veins, ‘sunsetting’ of the eyes (increased pressure prevents the child from looking upwards), irritability and failure to thrive. Once the child's sutures have fused and the fontanelle is closed, the predominant symptoms are headaches (usually worse in the morning, after lying flat), nausea/vomiting and eventually reduced conscious level.
In order to treat hydrocephalus, ventriculo-peritoneal (VP) shunts are commonly used to divert CSF from the lateral ventricles into the peritoneal cavity of the abdomen. However, tumours often secrete high protein levels into the CSF, which can make the CSF more viscous and, as a consequence, the shunt prone to blockage. In a series of 1250 children under the age of 18 years with brain tumours, Wong et al (2011) reported that 56.7* of patients demonstrated symptomatic hydrocephalus, with 51.5* of children's first presentation to hospital being due to hydrocephalus. In the vast majority of cases (98*), the hydrocephalus was predominantly obstructive as a result of the tumour mass.
VP shunts are commonly performed by neurosurgeons, but potential complications can include infection, blockage of the shunt, kinking/fracture of the shunt tubing, over- or under-drainage of CSF, seizures and injury to organs/major blood vessels during the procedure, and nurses will be involved in managing many of these consequences either post-operatively on the wards or in the community following discharge from hospital. Shunts are an excellent method to manage hydrocephalus, but unfortunately they are prone to failure due to obstruction, infection or mechanical failure. Typically, an operation to revise the shunt hardware or implant new hardware is required in 30-40* of children by 1 year following initial shunt implantation, and in 50* of cases by 2 years (Hanak et al, 2017). Children with tumours are even more prone to shunt failure compared with those with hydrocephalus due to other reasons (Tuli et al, 2000). Therefore a child with an inoperable brain tumour and resultant hydrocephalus may be committed to undergoing multiple revision operations if a shunt is placed.
An alternative strategy is to place an external ventricular drain (EVD), which is a tube/catheter that diverts CSF from the lateral ventricles to an external drainage bag (Figure 2A). EVDs are commonly used in trauma settings, whereby an external drain is used for a short period (typically <2 weeks) in order to divert CSF until drainage is no longer necessary (eg once the swelling has settled). These devices also have high complication rates, with one study of children undergoing insertion of an EVD demonstrating a 26* complication rate (Ngo et al, 2009). Complications include infection, bleeding, malposition or obstruction. The benefit of using EVDs is that they allow CSF flow to be assessed without the need for an operation, because they are externalised drains (unlike a shunt), thus preventing the need for general anaesthetic and surgical intervention. Infection is the most common and concerning complication; however, there is some evidence that the risk of EVD infections can be reduced if the externalised catheter is tunnelled underneath the skin to a site distant from the ventricle (Figure 2B) (Collins et al, 2014; George et al, 2019; Zhou et al, 2019).
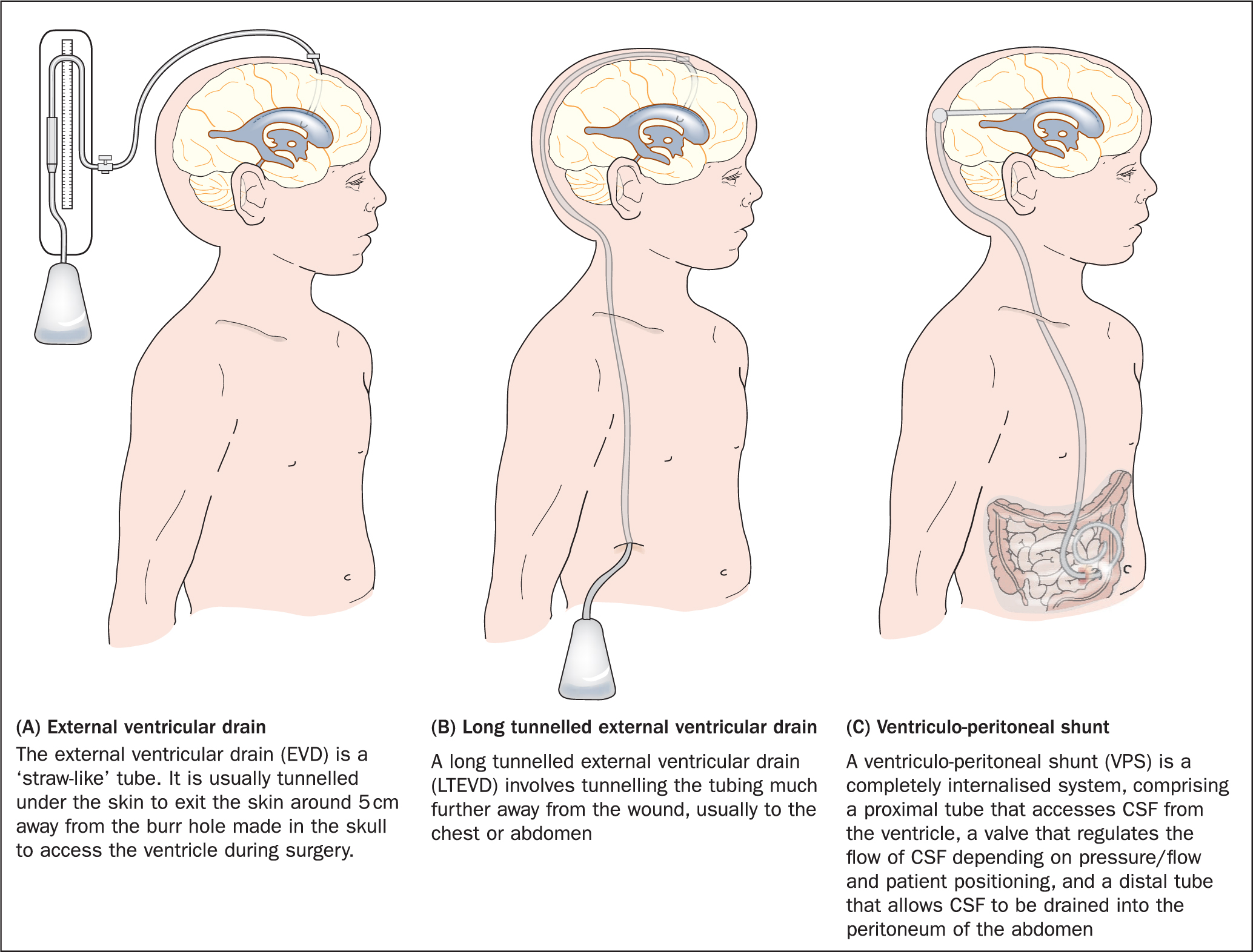 Figure 2. Alternative strategies for drainage of cerebrospinal fluid from the ventricles
Figure 2. Alternative strategies for drainage of cerebrospinal fluid from the ventricles
The catheter tubing from the EVD is connected via a three-way tap to a drainage system. This system comprises a collection chamber that is hung from an intravenous pole at the head of the bed (Figure 3). The collection chamber can be moved up and down against a pressure scale next to the chamber, allowing the neurosurgeon to control the maximum permitted ICP, which will be individualised depending on the patient's underlying clinical condition and may vary during their recovery. The pressure scale usually displays pressure in both cmH2O and mmHg (Figure 3). Drainage depends on gravity, so the height of the drainage system is vital in managing CSF diversion.
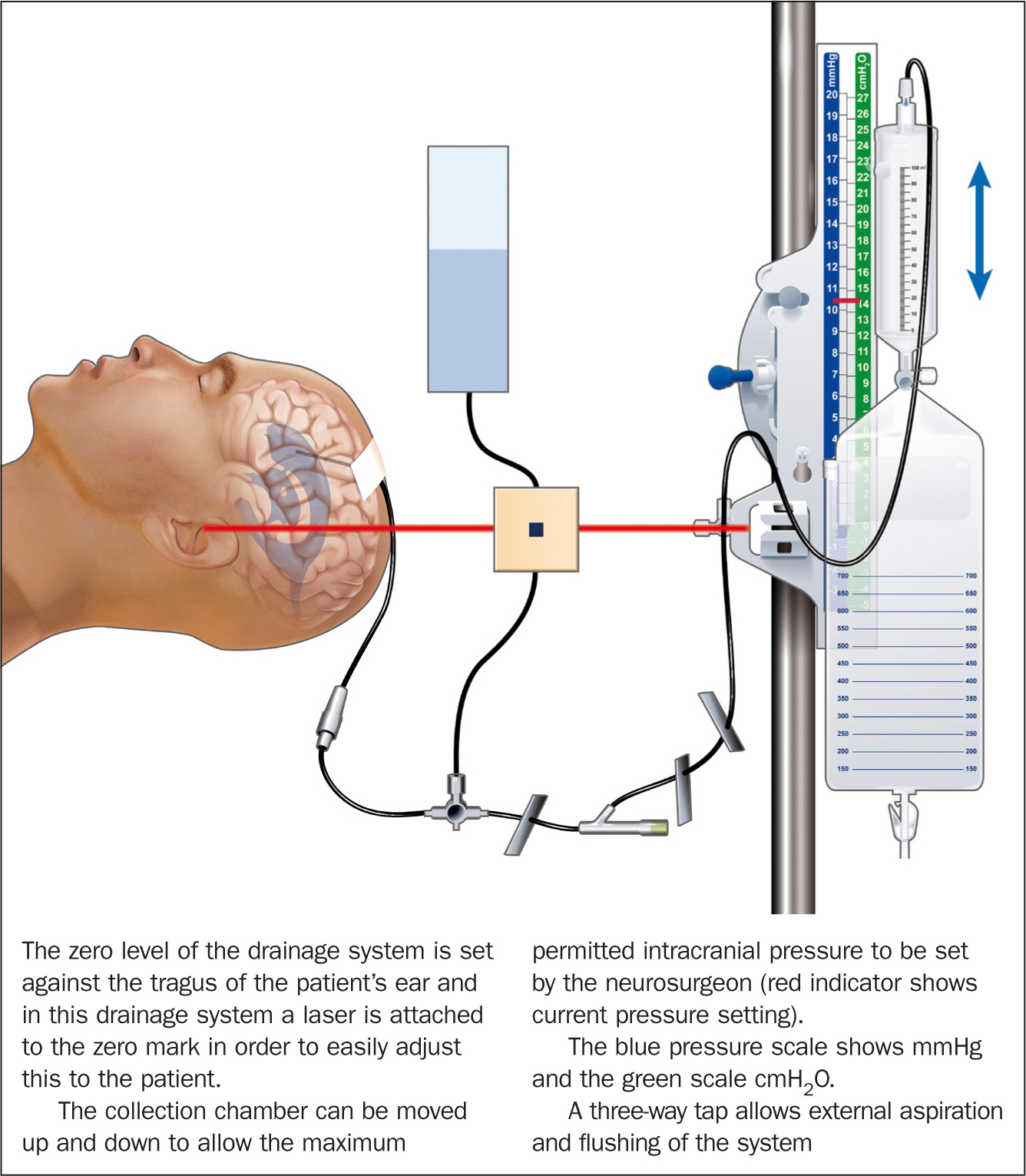 Figure 3. Key components of a CSF external drainage system
Figure 3. Key components of a CSF external drainage system
The zero point of the drainage system should line up with the patient's ear (the tragus), which is roughly at the level of the inter-ventricular foramen (of Monro), at the centre point of the brain. The collecting chamber is then set at a prescribed level above the zero point depending on the neurosurgeon's judgement, based on the underlying clinical condition and the findings of the patient's imaging. Whenever ICP exceeds the prescribed pressure setting, CSF is diverted from the brain into the collecting chamber, controlling maximum ICP in order to prevent symptoms of hydrocephalus. The zero level should be adjusted in accordance with the patient's position (eg sitting/standing/lying) as soon as it changes, so that over- or under-drainage does not occur. Under-drainage may lead to symptoms of hydrocephalus, while over-drainage may collapse the ventricles, causing the brain to ‘sink’, with subsequent headache and stretching of the subdural veins that bridge the space between the brain and its overlying membrane, the dura. Stretching of these veins can lead to bleeding (subdural haemorrhage).
A stopcock at the base of the collection chamber permits hourly measurements of CSF drainage and connects to a drainage bag below, enabling the collected fluid to be emptied.
Case study
Presentation
At the age of 4 months, Sam (not his real name) was admitted to the Royal Hospital for Sick Children (RHSC) in Edinburgh for investigation of failure to thrive. On admission, he was noted to have disconjugate eye movements, and a subsequent MRI scan of his head revealed an avidly enhancing suprasellar tumour of 5.2 cm × 4.4 cm × 5.2 cm in size (Figure 4). A biopsy was obtained via an endoscopic right frontal trans-cortical, intraventricular approach, with a right frontal Ommaya reservoir (intraventricular device implanted under the scalp) left in situ in anticipation of future development of hydrocephalus. A diagnosis of a hypothalamic World Health Organization grade I pilocystic astrocytoma (Louis et al, 2016) was made.
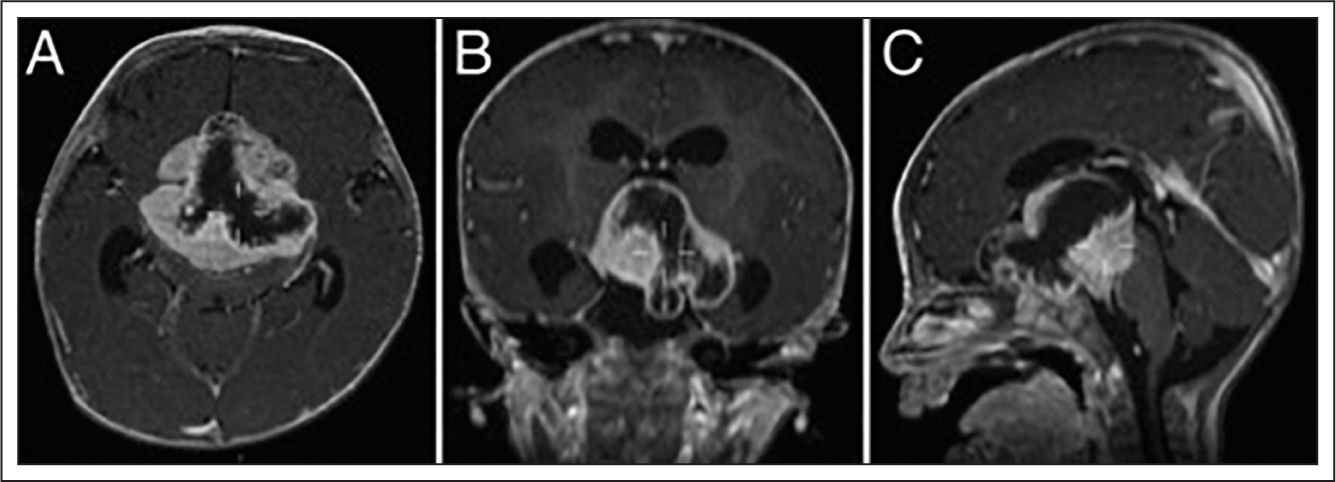 Figure 4. Preoperative MRI scans (axial, coronal, and sagittal), showing the suprasellar lesion extending superiorly into the third ventricle and occluding both interventricular foramina (of Munro). Prominent temporal ventricular horns suggest impending hydrocephalus
Figure 4. Preoperative MRI scans (axial, coronal, and sagittal), showing the suprasellar lesion extending superiorly into the third ventricle and occluding both interventricular foramina (of Munro). Prominent temporal ventricular horns suggest impending hydrocephalus
Initial treatment
A few days after the operation, Sam began to demonstrate evidence of raised intracranial pressure. Hydrocephalus was diagnosed on imaging of the head, which revealed enlarged ventricles. Sam therefore underwent insertion of a VP shunt. One week after shunt insertion, he again developed evidence of raised ICP. A CT scan revealed that the shunt catheter had migrated from the ventricle, requiring another operation to remove and replace the cranial tubing. Sam recovered well after this.
The case was discussed at the paediatric neuro-oncology multidisciplinary team meeting (consisting of paediatric neurologists, oncologists, neurosurgeons, radiologists, microbiologists, palliative care experts, and hospital and community nursing staff), and the tumour was considered to be inoperable due to its size and location. Therefore, Sam was treated with a 6-week course of chemotherapy (three cycles of vincristine and carboplatin, with two concurrent cycles of temozolomide). Unfortunately, the tumour proved unresponsive to chemotherapy, and a decision was made by the multidisciplinary team to treat Sam palliatively. The palliative care team and local children's hospice were involved at this stage and provided fantastic support to the parents, with both psychological support and helping with the practicalities of managing Sam's condition at home. The importance of excellent communication within the multidisciplinary team, including the hospital, hospice and community team, was paramount—Sam's and his family's quality of life was always at the centre of all decision-making.
Although the tumour was inoperable, there was still a role for surgery in treating the hydrocephalus, and palliative care included CSF diversion to relieve raised ICP whenever the VP shunt blocked. Over 35 months Sam went on to have 12 surgical VP shunt revisions. His VP shunt was then converted to a ventriculo-atrial shunt, whereby the distal portion of the shunt is placed through the external jugular vein into the right atrium where CSF is drained. This is less commonly employed than the peritoneal route, but a viable alternative in the case of difficulty accessing the peritoneal cavity. The multiple operations on Sam's abdomen had made access to the peritoneal space difficult due to adhesions. Again, shunt blockage proved problematic and Sam required a further two revision operations within the following month.
Treatment using long tunnelled EVD
At this stage, a decision was made to attempt treatment using an LTEVD, rather than continue to face problems with the shunt system. This was discussed with the parents, and offered as a potential long-term management strategy with support of the multidisciplinary team.
The proposed benefit of an LTEVD was that, when a malfunction was suspected, CSF flow through the tubing could be checked without the need for any surgery, given that the tubing was externalised. This would reduce the risks and morbidities associated with surgical exploration, exposure to additional radiation through recurrent imaging, the cumulative effects of general anaesthetics and the requirement for hospitalisation, along with the psychosocial distress to the family and complications associated with hospital admission, such as hospital-acquired infections.
Under general anaesthetic, a frontal valveless antibiotic-impregnated catheter was inserted into the lateral ventricle and tunnelled subcutaneously down to the para-umbilical area where it was externalised.
As long as Sam's symptoms were controlled, he was able to maintain a good quality of life, playing with his friends and family, and feeding normally. When his ICP increased, he would suffer symptoms—such as headache, becoming agitated or sleepier—that prevented these activities, and the LTEVD allowed the withdrawal of extra CSF on such occasions. Although early warning systems, such as a paediatric early warning score (PEWS), are excellent tools for identifying deterioration in hospital patients, they have been chiefly developed with respiratory and cardiovascular changes in mind and, although raised ICP may manifest with changes in the PEWS score and changes in pupil function, this tends to happen after the traditional symptoms of hydrocephalus occur. Therefore, the team did not want to overmedicalise Sam's home life and considered that treatment on the basis of his symptoms was the best option for the situation.
Sam's parents were educated on the management of the EVD. The neurosurgical team instructed them on the basics of the anatomy and physiology of CSF and how the drains both functioned and malfunctioned. They were taught how to change the collection bag in a sterile manner by the nursing staff on the neurosciences ward, how to recognise signs and symptoms of under-drainage, and how to manually drain CSF from the drain in a sterile manner. They were also taught how to recognise issues with excess flow and how to clamp off the LTEVD in case of over-drainage. Sam's parents were made aware of the signs and symptoms of infection and when to re-present to the hospital. Long-term prophylactic antibiotics (rifampicin) were prescribed on the advice of microbiology in order to prevent infection of the drain system, and Sam and his parents were given open access to the neurosurgical ward at the RHSC, alongside his community nursing care.
Initially, this was a huge amount of information take to in, and we understood the potential for this to overwhelm the parents. It is a testament to both their fortitude and the strength of the support of the acute and community nursing teams that, despite their own journeys through the grieving process, the parents were able to take in this information and manage Sam's drains independently. Although this initial phase of education and support was a significant investment on behalf of the entire clinical team, it proved wholly worthwhile because Sam's parents became experts in managing the drains and were able to understand when they needed to intervene to drain off extra CSF or, indeed, when Sam was in need of acute hospital admission.
Setting up Sam's care at home involved the creation of patient-specific protocols that were initially used to educate his parents about the signs/symptoms that they should be aware of and monitor, and how to drain CSF and attempt to unblock the drains. These protocols were then used for the clinicians who helped look after Sam both in the community and within acute services, including doctors and specialist nurse practitioners. The protocols were created using a multidisciplinary approach, and Sam's parents were included in the process because they added to the subtle signs and symptoms that he often displayed when a problem arose with his drains.
The protocol outlined patient-specific signs/symptoms of raised ICP, including:
- Changes in behaviour (being quiet or agitated)
- Pallor
- Sleepiness/low energy levels
- Gagging, retching
- Eye squinting, rapid eye movements
- Irritability/crying out
- Holding his head.
If there was concern regarding CSF drainage, the first step was to check that the position of the patient and the drainage system were correct. If no CSF had drained for 6 hours, or symptoms of raised ICP manifested, then the LTEVD could be aspirated in an attempt to unblock the tubing. Aspiration was performed first in order to clear the tubing proximal to the three-way tap, following which the three-way tap could be flushed distally towards the drainage bag with saline in order to clear the distal tubing of debris. Flushing of saline through the three-way tap to prevent blockage was performed routinely, twice daily, and also as required.
If neither aspiration nor flushing the tubing to unblock the LTEVD and reinstate CSF flow worked, then the situation was escalated to the neurosurgical ward and the on-call team.
Complications
Following initial insertion, the left LTEVD was in situ for 58 months in total, with six revisions: two due to proximal catheter blockage, three due to distal catheter blockage, and one due to both proximal and distal blockage. After treatment using the LTEVD for 4 years, a decision was made to insert another LTEVD on the other side of the head in the right ventricle, given that the tumour had grown so much that it was impeding the flow between the two ventricles. The new LTEVD was in situ for 10 months in total, with two revisions (one due to proximal catheter blockage, and one due to blockage of the distal tubing).
A septostomy was also performed approximately 2 months after insertion of the second LTEVD: when revising the shunt for obstruction, a hole was made in the septum separating the walls of the two lateral ventricles in order to improve CSF flow across the ventricular system. This meant that, if one drain blocked, the other drain could maintain drainage of both ventricles, again reducing the risk of Sam requiring more surgery. Unfortunately, following this operation Sam developed a CSF infection with Serratia marcescens and Staphylococcus aureus. This was treated with a 3-week course of antibiotics and Sam made a good recovery. Sadly, a few months later, he again developed CSF infection and, despite antibiotic therapy, he continued to deteriorate. At this stage, a decision was made by the treating clinical teams together with the parents that, in his best interest, Sam's care should be wholly taken over by the palliative care team who had been deeply involved in his care from the beginning. He was transferred to the local children's hospice, which he knew well, and he died there peacefully with his family by his side.
Discussion
Empowerment of parents/guardians in the management of their children's condition is not new in health care. Chronic conditions often require parents/guardians to undertake medical or nursing duties above and beyond their usual duties as parents. In order to achieve this, education of the parents/guardians is key so that they can identify and respond to symptoms appropriately. As they learn more and more about the particular condition and how to best manage it for their child, they expect to be heavily involved in care decisions, although research has suggested that they still require a great deal of support from health professionals in making difficult decisions through shared responsibility (Smith et al, 2015).
With regard to Sam's care, the whole team, including hospital and community clinicians, were aware of all facets of the case and were kept abreast of progress continually. Moreover, key information regarding the case, including the patient-specific protocols, was flagged up on the hospital system in order to be easily available if urgent hospitalisation was required and in case a clinician who had not been involved in Sam's care needed to assess him. The family were empowered to contact/attend the paediatric neurosurgical ward directly should they have any concerns, and this generally meant that they could contact a clinician who knew their case well, rather than going via the emergency department. Good education and support from the entire team meant that the parents were able to easily recognise symptoms of hydrocephalus at home and promptly aspirate CSF to relieve them, importantly keeping the family from having to attend hospital on numerous occasions and maximising quality of life of both Sam and his family. The benefits of this management strategy in terms of the psychosocial impact on the family and also the economic benefit to the NHS cannot be overstated.
In future similar cases, where an inoperable tumour is causing hydrocephalus and we feel that this is the best option, we would consider the use of LTEVDs much earlier in the patient's journey. Having been through the journey and reflected upon it in multidisciplinary team meetings and in governance meetings, we feel that, as a service, we are better set up to face the challenges of supporting families in similar circumstances in the future. The key factors that enabled success in the use of LTEVDs to maximise the patient's quality of life through the palliative process were good communication between different clinical teams within the hospital and the community, the setting up of patient-specific protocols, and having easily accessible information across the hospital IT systems, as well as allowing the patient and his family direct access to the neurosciences ward for advice/admission and always remembering that both his and the family's quality of life were paramount.
Conclusion
As a multidisciplinary team that includes neurosurgeons, we recommend that LTEVDs should be considered in patients with hydrocephalus related to tumours, especially in the context of progressive tumour growth without the option for surgical excision. In the case described in this article, two LTEVDs were used over a long period of time, with only two instances of infection. Although eight operations were required due to obstruction of the LTEVDs, the child's parents were taught to manage the drains in order to relieve excess pressure and, upon numerous occasions of catheter blockage, they flushed the systems in a sterile manner as per the patient-specific protocol, negating the need for hospitalisation or further operations.
The use of LTEVDs demonstrated a clear advantage over using an internalised shunt system, which would require surgical intervention in the case of obstruction. In Sam's case, the LTEVDs allowed relief of hydrocephalus and allowed him to continue to live a good quality life for a number of years, despite the progression of the tumour.
KEY POINTS
- A variety of techniques can be used to drain CSF from the ventricles and relieve the symptoms of hydrocephalus, including an EVD, long tunnelled EVD (LTEVD) and VP shunt
- An LTEVD is a valid treatment option for patients with hydrocephalus in a palliative care setting
- In the knowledge of the authors, this is the longest reported case of the use of a LTEVD for hydrocephalus
- Long-term antibiotics aid prevention of infection and choice of agent should be guided by the local microbiology team
- Parental education and empowerment is vital to successful management
CPD reflective questions
- What are the key differences between an EVD and a VP shunt?
- Where should the zero point on the collection chamber be set to against the patient?
- How should the three-way tap be cleaned when performing aspiration/flushing?


