This article focuses on non-invasive blood pressure (BP) measurement, using the manual technique. This vital observation is practised by all nursing fields in primary and secondary healthcare environments.
What is blood pressure?
A BP measurement in its simplest form is a determinant of individual cardiac output (the volume of blood pumped out of the heart and into the aorta per minute) and the systematic vascular resistance (the diameter of the arterial blood vessels) (Foley, 2015).
BP measurement is widely recognised as being a routine observation that can be used as a way to assess cardiac output and its effectiveness for adequate tissue perfusion (Odell, 2013). Thus, the presence of a BP is a requirement for human existence and BP measurement, which includes interpreting results and taking appropriate action, is considered a key clinical skill to acquire and maintain as results can determine patient care (Doughty and Lister, 2015).
Many factors can influence a BP reading, for example, age, sleep, emotions and activity. Consequently, evidence in the literature varies as to what constitutes a normal reading, and optimal parameters are often used instead (Moore, 2017). Dougherty and Lister (2015) state that the normal BP at rest has the range of 110–140 mmHg for systolic and 70–80 mmHg for diastolic BP.
Hypertension (high BP) refers to measurements that exceed the resting systolic parameters and hypotension (low BP) refers to those that fall below resting systolic parameters. Hypertension and hypotension, if left undetected and unmanaged, can have serious implications for an individual, including reduced tissue perfusion if hypotensive and cardiac ischaemia if hypertensive (Wallymahmed, 2008).
BP measurement consists of two readings, which are recorded like a fraction, with one reading on top and the other below, i.e. 120/80 mmHg (Box 1) (Moore, 2017). The uppermost reading, known as the systolic, is the first to be taken: it measures the peak force of blood as it pushes against the walls of the arteries as the heart's left ventricle contracts, pushing blood into the aorta and causing an increase in pressure (Fetzer, 2014; Foley, 2015). The lower reading, the diastolic, measures the force exerted on the walls of the arteries as the heart relaxes and refills.
Blood pressure basics
| Systolic | 120 |
| Diastolic | 80 |
Different arteries can be used to measure BP. However, due to ease of access, the manual technique is generally associated with measuring brachial arterial pressure, a major blood vessel that runs through the upper arms before dividing below the anticubital fossa.
What is involved in taking a manual BP?
Two main pieces of equipment are required to take a manual BP: an aneroid sphygmomanometer and a stethoscope (Figure 1a and Figure 1b).
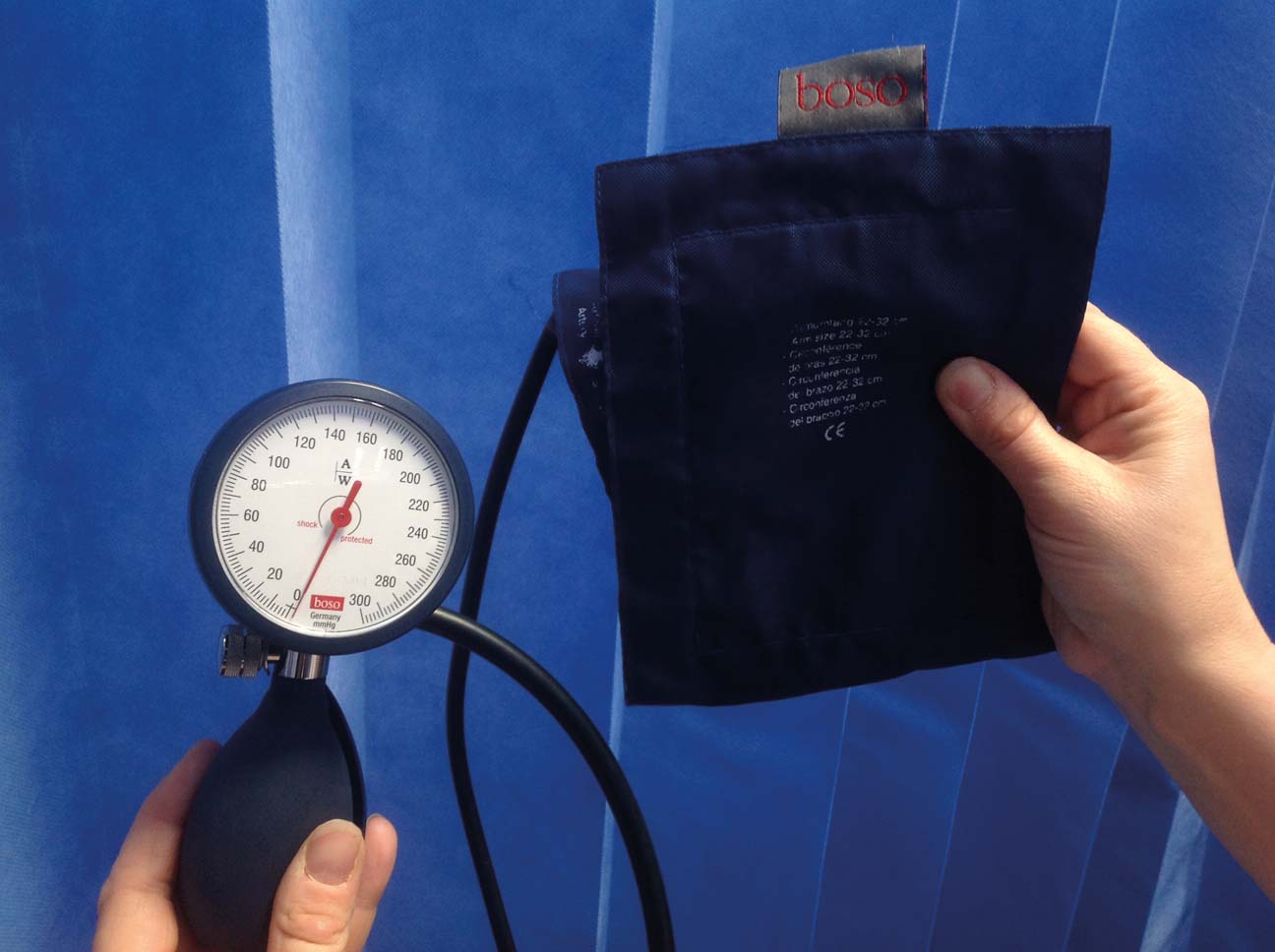
The sphygmomanometer consists of a cuff that houses an inflatable bladder, a manometer (dial) and a mechanism to pump up the cuff, known as the inflation bulb. Measurement of BP involves:
The following occurs during this process: the pressure in the bladder situated within the cuff fills to a point where pressure within the cuff exceeds the blood flow in the brachial artery. The cuff, therefore, acts like a tourniquet, by temporarily excluding blood flow to the artery. Opening the valve attached to the inflation bulb slowly releases air from the bladder, the cuff pressure falls and, when the systolic pressure becomes greater than the pressure remaining in the cuff, a sound will be heard through the stethoscope (Levick, 2010).
The sounds that can be heard are referred to as Korotkoff sounds; these can often be described either as a faint tapping, thudding or ticking sound — it is the first Korotkoff sound (Table 1) that is used to determine the systolic reading (Foley, 2015). As air continues to be released from the bladder, pressure in the cuff decreases further, reducing restrictions on the arteries, the blood flow starts to return to normal and the Korotkoff sounds disappear, indicating the diastolic reading (Fetzer, 2014).
| Silence will be heard before cuff inflation. Sounds will be heard only when Phase I starts | |
| Phase I | First tapping, thudding sound (volume and clarity of sound vary between patients) |
| Phase II | Sounds change to a murmur and can be distinguished as a swishing sound |
| Phase III | The sounds in phase III are louder than phase I and are distinguished as knocking sounds |
| Phase IV | Sounds become muffled as pressure in the cuff decreases. They can again be distinguished as swishing sounds |
| Phase V | Silence |
Source: Dougherty and Lister, 2015
Electronic versus manual devices
While the manual auscultation technique is considered the gold standard for BP measurement, advances in medical technology have resulted in alternative ways of measuring and monitoring BP (James and Gerber, 2018).
The Nursing and Midwifery Council (2018) and the National Institute for Health and Care Excellence (NICE) (2011) advocate the use of either manual or technological devices, with neither option being favoured over the other. However, there are advantages and disadvantages to both methods—a level of clinical knowledge and skills for manual and electronic measurements are requirements within clinical practice. Moreover, while electronic devices have become the ‘go to method’, it is essential that nurses maintain the skills and confidence in using the manual method (Moore, 2017), especially for patients with hypertension, hypotension or pulse irregularities. Pulse irregularities can cause inaccuracies in electronic readings (NICE, 2011; Foley, 2015) and this can lead to false diagnosis and incorrect treatment.
In addition, if there are any doubts over an electronic BP reading, a manual reading should be obtained to verify BP (Dougherty and Lister, 2015). Using clinical judgement when doubts arise is often associated with the art of noticing (Tanner, 2006; Watson and Rebair, 2014: Lancaster et al, 2015). Failure to interpret and, ultimately, respond appropriately to clinical cues to uncover clinical signs of deterioration linked to changes in BP can have serious consequences (Watson and Rebair, 2014; Lancaster et al, 2015).
How to take a manual BP
Poor technique is another factor that can lead to inaccuracies in BP measurements. It is therefore important to follow the correct technique (Dougherty and Lister, 2015; O'Brien, 2015; Moore, 2017; British and Irish Hypertension Society, 2017):


Common causes of error
Top tips for using a stethoscope
Inaccuracies with the readings often result from reduced hearing, which can be caused by the incorrect opening of the diaphragm of the stethoscope and incorrect insertion of the earpieces (i.e. being placed in the ear canal in the wrong direction) (Wallymahmed, 2008; Tomlinson, 2010; Dougherty and Lister, 2015):
Tops tips for cuff application
Loose and incorrectly placed cuffs are a common problem associated with inaccurate BP measurements. So ensure that:

Tops tips for using the valve on the inflatable bulb and reading the measurements on the dial
Opening, closing and controlling the valve, in particular the speed, are common problems that lead to inaccurate readings. This can be avoided, so:

