Osteoarthritis (OA) refers to a clinical syndrome of joint pain accompanied by varying degrees of functional limitation and reduced quality of life (National Institute for Health and Care Excellence (NICE), 2014). The most affected peripheral joints are the knees, hips, and small hand joints. Pain, reduced function, and effects on a person's ability to carry out their day-to-day activities can be important consequences. Pain in itself is also a complex biopsychosocial issue, related in part to a person's expectations and self-efficacy (that is, their belief in their ability to complete tasks and reach goals), and is associated with changes in mood, sleep and coping abilities. There is often a poor link between changes visible on an X-ray and symptoms of osteoarthritis: minimal changes can be associated with a lot of pain, or modest structural changes to joints can occur with minimal accompanying symptoms. Contrary to popular belief, OA is not caused by ageing and does not necessarily deteriorate (NICE, 2014).
Epidemiology and risk factors
OA is the most prevalent form of arthritis and a leading cause of pain and disability worldwide (NICE, 2014; O'Neill et al, 2018; Vina and Kwoh, 2018). It affected 303 million people globally in 2017 (James et al, 2018). In the UK approximately 8.5 million people have joint pain related to OA (NICE, 2014). A recent review by Kloppenburg and Berenbaum (2020) suggested that epidemiological studies are needed to confirm premature mortality in OA and its associated physical disabilities.
OA involves degradation of the articular cartilage, synovium, and subchondral bones causing joint pain, functional limitation and reduced quality of life (Cooper et al, 2013). OA can affect any joint. The knee, hip, hand and spine are the most common sites of OA—Deshpande et al (2016) estimated that 14 million people in the USA have symptomatic knee OA—but it can also occur in the ankles and wrists (Arden and Nevitt, 2006).
The UK Clinical Practice Research Datalink (CPRD) comprising data on nearly 17.5 million patients was used for a UK prevalence of osteoarthritis study (Swain et al, 2020). The standardised incidence of any OA in 2017 was 6.8 per 1000 person-years (95% CI 6.7 to 6.9) and prevalence was 10.7% (95% CI 10.7–10.8%). Both incidence and prevalence were higher in women than men. The incidence of any OA decreased gradually over 20 years at an annual rate of −1.6% (95%CI -2.0 to −1.1%), and the reduction was faster for people born after 1960. The prevalence of any OA increased gradually at an annual rate of 1.4% (95% CI 1.3–1.6%). Although the prevalence was highest in Scotland and Northern Ireland, incidence was highest in the East Midlands. Both incidence and prevalence reported highest in the knee followed by hip, wrist/hand, and ankle/foot.
The risk factors for OA can be divided into person-level factors, such as age, sex, obesity, genetics, race/ethnicity and diet, and joint-level factors including injury, malalignment and abnormal loading of the joints (Johnson and Hunter, 2014). Age is the single greatest risk factor for the development of OA (Shane-Anderson and Loeser, 2010). Women are at greater risk of OA and women have more severe symptoms than men, especially after menopausal age (Srikanth et al, 2005). Other risk factors associated with OA can be seen in Box 1 (Harris and Crawford, 2019).
Box 1.Risk factors for osteoarthritis
- Age
- Female gender
- Obesity
- Lack of osteoporosis
- Occupation
- Participation in sports
- Previous injury
- Muscle weakness
- Proprioceptive deficits
- Family history of osteoarthritis
- Acromegaly
- Calcium crystal deposition
Source: Harris and Crawford, 2019
Osteoarthritis characteristics and diagnosis
OA is characterised pathologically by localised loss of cartilage, remodelling of adjacent bone and associated inflammation (NICE, 2014). A variety of traumas may trigger the need for a joint to repair itself. OA includes a slow but efficient repair process that often compensates for the initial trauma, resulting in a structurally altered but symptom-free joint. In some people, because of either overwhelming trauma or compromised repair, the process cannot compensate, resulting in eventual presentation with symptomatic OA; this might be thought of as ‘joint failure’. This in part explains the extreme variability in clinical presentation and outcome that can be observed between people, and at different joints in the same person.
OA can be diagnosed clinically, pathologically, or radiographically (Zhang and Jordan, 2010). Primarily, clinicians may define OA by examining the patient's signs and symptoms, and risk factors. According to the NICE (2014) OA guidelines:
‘OA should be diagnosed clinically without investigations if a person: is 45 or over and has activity-related joint pain and has no morning joint-related stiffness, or morning stiffness that lasts no longer than 30 minutes.’
Laboratory testing such as inflammatory markers are not usually required to diagnose OA. Generally, inflammatory markers, such as erythrocyte sedimentation rate and C-reactive protein level, are normal in OA patients (Sinusas, 2012). Radiography such as plain X-rays could be used to confirm the diagnosis. The most common radiographic grading system for OA is the Kellgren and Lawrence grade, which scores the severity on a scale of 0 to 4. A score of 2 or above in Kellgren and Lawrence indicates definite radiographic osteoarthritis (Kellgren et al, 1963).
Recommendations for practice
The Osteoarthritis Research Society International has stated the goals of OA management include pain management and optimal functional ability. To that end, it has updated and expanded on its guidelines regarding the management of OA of the hip and knee by developing patient-focused treatment recommendations for individuals with knee, hip, and polyarticular OA that are derived from expert consensus and based on objective review of high-quality meta-analytic data (Bannuru et al, 2019).
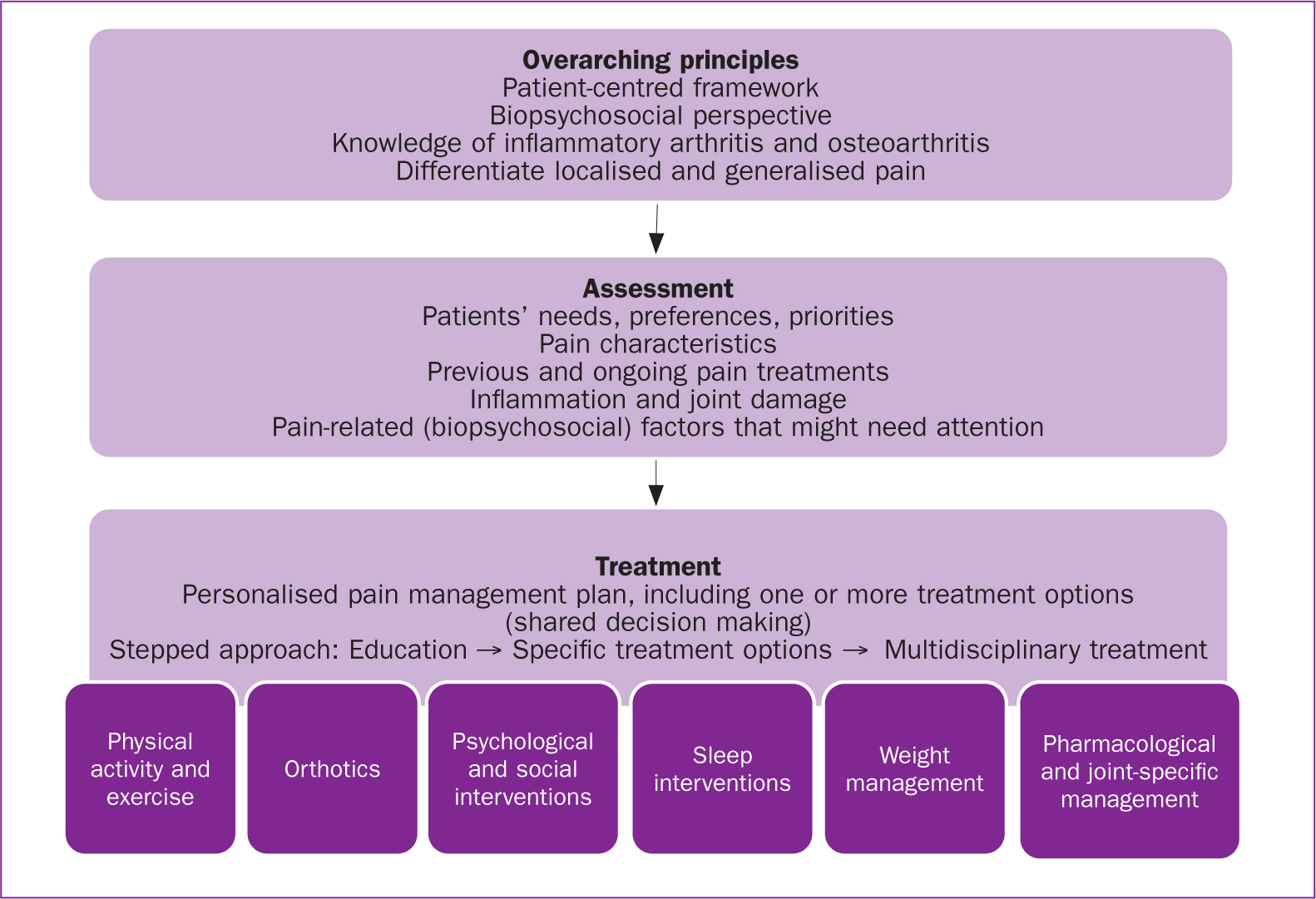
European League Against Rheumatism (EULAR) recommendations for the health professional's approach to pain management in inflammatory arthritis and osteoarthritis are guided by expert opinion and partly underpinned by a considerable number of systematic reviews and meta-analyses. An expert group developed and launched the first set of recommendations that enable health professionals to provide knowledgeable and evidence-based pain-management support for people with inflammatory arthritis and OA (Geenan et al, 2018) (Figure 1).
Since there is as yet no cure for OA, the management of risks and predisposing factors is vital in delaying disease progression. The treatments that are currently available for OA are aiming for pain reduction, correcting deformities, and improving joint function to improve the quality of the patient's life (NICE, 2014). Nurses have a vital role in reducing the pain and disability caused by OA. In 2011, an OA symposium convened experts in areas of nursing, epidemiology, rheumatology, public policy, geriatrics, pharmacotherapy, physical therapy, and complementary modalities to discuss the importance of nurses in reducing the disability caused by OA (Robbins and Kulesa, 2012). The symposium produced five important themes to be considered: knowledge of OA burden, OA national initiatives to help raise awareness, risk and progression assessment for OA, interventions to relieve OA symptoms, and minimising progression/self-management support. These themes emphasise that there is no single treatment that can work for all. OA management must incorporate different treatment options, primarily non-pharmacological, then pharmacological, and finally surgical interventions.
Non-pharmacological
Non-pharmacological treatments for OA include patient education, exercise, weight loss, and physiotherapy (Geenan et al, 2018). NICE (2014) recommends that the non-pharmacological treatments should be considered for all OA patients irrespective of age, comorbidity, pain severity or disability. Although they may show a limited effect in reducing symptoms, one of their main advantages is that they pose no inherent risks (Scott and Kowalczyk, 2007).
NICE (2014) advises people with osteoarthritis to exercise as a core treatment irrespective of age, comorbidity, pain severity or disability. Exercise should include local muscle strengthening and general aerobic fitness. It has not been specified whether exercise should be provided by the NHS or whether the health professional should provide advice and encouragement to the person to obtain and carry out the intervention themselves. Exercise has been found to be beneficial, but the clinician needs to make a judgement in each case on how to effectively ensure participation. This will depend on the person's individual needs, circumstances and self-motivation, and the availability of local facilities. Manipulation and stretching should be considered as an adjunct to core treatments, particularly for osteoarthritis of the hip.
Drug therapy
Several non-pharmacological and pharmacological measures are available, either individually or in combination, for treating the widespread disease and public health issue that is OA. Only some of those patients with radiologically detectable OA will actually suffer clinically relevant symptoms. However, when the arthritis becomes symptomatic and painful, drug therapy can then be useful. According to Steinmeyer et al (2018) pharmaceuticals represent an essential pillar of therapy, and a wide range of very different drugs, especially non-steroidal anti-inflammatory drugs (NSAIDs) in combination with other medications (eg proton pump inhibitors), opioid analgesics, potentially cartilage active agents and phytopharmaceuticals, have all found use. Topical agents are also popular since they exert fewer systemic side effects and enjoy a high level of acceptance from patients. In addition, glucocorticoids and hyaluronic acid preparations are among those medications used for intra-articular OA therapy.
The current NICE (2014) guidance suggests that paracetamol should be offered for pain relief in addition to the core treatment (exercise). Paracetamol does not have the high risk of adverse effects found with other potentially more effective options, such as NSAIDs or opioids. However, the Guideline Development Group highlighted that its evidence review relating to the effectiveness of paracetamol should be taken into account, pending a fuller review of pharmacological treatments.
NICE (2014) recommends that alternative or additional medication should be considered for patients who do not experience adequate symptomatic relief with exercise and paracetamol or topical NSAIDs. Systemic NSAIDs and cyclooxygenase-2 (COX-2) inhibitors have been shown to be effective in reducing pain and inflammation but they are associated with gastrointestinal, liver, kidney and cardiovascular side effects ranging from mild to severe (Fraenkel and Fried, 2008; Al-Omari, 2017). Thus, topical NSAIDs are recommended ahead of oral. NSAIDs and COX-2 inhibitors may be regarded as a single drug class but NICE (2014) continues to use the two terms for clarity, and because of the differences in the side effect profiles.
Opioid analgesics can be considered to treat pain associated with OA (NICE, 2014). However, they should be the last choice when other medications fail to provide adequate pain relief (NICE, 2014)—taking into account their risk:benefit profile (Freynhagen et al, 2013).
Intra-articular (IA) steroid injections offer a potentially useful therapy as it is directly targeted at the affected joint with few systemic effects. Guidelines produced by EULAR (Zhang et al, 2005), the American College of Rheumatology (ACR) (Hochberg et al, 2012), and Osteoarthritis Research Society International (Zhang et al, 2008) also recommend their use in the management of hip OA. However, as acknowledged by the ACR expert panel ‘few trials have been performed in patients with symptomatic hip OA,’ and their recommendations are based on their assessment that ‘patients with hip OA should be treated in a similar fashion to those with knee OA’ (Hochberg et al, 2012). Variations in the degree of pain relief reported by patients with OA following IA corticosteroid injections are well recognised. In their systematic review Hirsch et al (2013) concluded that previous research had not identified reliable predictors of response to IA corticosteroid injections, and that further studies are required if this question is to be answered. McCabe et al (2016) noted that international guidelines recommend IA steroid injections in the management of hip OA, although these recommendations are extrapolated primarily from studies of knee OA. Their systematic review focused on the efficacy of this treatment on pain in hip OA. The conclusion was that hip IA steroid injections may be efficacious for short-term pain reduction in those with hip OA, though the quality of the evidence was relatively poor. Further large, methodologically rigorous trials are required to verify whether IA corticosteroids are beneficial and for how long.
Surgery
The final choice of treatment is surgical interventions such as joint replacement. The non-pharmacological treatments for OA are recommended at all levels of disease severity, whereas surgery is only recommended when patients meet certain criteria that include prolonged and established functional limitation and severe pain with a substantial impact on quality of life (NICE, 2014).
Conclusion
OA is a chronic disabling condition that still has no cure. Managing OA includes pharmacological and non-pharmacological treatment to control the disease progress, reduce pain and improve mobility. Arthritis and its complications can severely impact an individual's health and quality of life. With thorough assessment, suitable referrals, and appropriate interventions, nurses can help patients with OA lead safe, active, and optimally independent lives.
LEARNING OUTCOMES
- Improve awareness of the risk factors for osteoarthritis
- Be aware of the multifactorial nature of osteoarthritis management
- Understand the key role of non-pharmacological treatments and self-management support

