December 2022 saw the start of the first ever strikes by Royal College of Nursing (RCN) members, simultaneously presenting a mixture of feelings, including sadness, pride, and solidarity. Sadness that the nursing workforce has been compelled to take this action through decades of government shortfalls, but pride in the solidarity of nurses seeking to safely staff our profession in the long term, ultimately protecting our patients.
However, the Health Secretary and mainstream media seem intent on focusing on ‘unreasonable pay demands’ and ‘maintaining safety’ during any disruptions. The picket lines tell a different story. This isn't just about nursing salaries, this is about safe staffing and a sustainable professional workforce in the NHS, both now and in the future. We know wages have remained stagnant in relation to inflation, presenting nurses with real terms pay cuts as living costs are rising faster than salaries, but this is only one contributing factor to the workforce issues we are facing.
‘NHS providers are expected to support and deliver the NHS Long Term Plan, to invest in their workforce and support the wellbeing of staff, yet in practice this is hard to achieve with chronic underfunding and bureaucracy.’
Since August 2017, government policy reforms have meant nursing students in England are no longer able to access NHS bursaries (Department of Health, 2017), instead having to access student loan systems for tuition fees and living costs, leaving them typically with £54 000 of debt once they graduate. This may be particularly difficult to swallow as a nursing student, given that undergraduate training involves both academic study and hours of workplace-based shift placements, unpaid but unquestionably supporting the existing NHS workforce. These reforms have contributed to a decline in nurse graduates, and a decline in university applications for nursing programmes. UCAS, the university and colleges admissions service, recently revealed a worrying 10% drop in the number of students accepted onto nursing courses across the UK in 2022 (UCAS, 2022), supporting valid concerns for workforce recruitment and sustainability for the years to come.
In addition, data from NHS England revealed 47 496 registered nurse vacancies in September 2022, an increase from 39 931 from the same period the previous year (NHS Digital, 2022a). Fewer applicants for undergraduate training places and increasing nursing vacancy rates provide growing support for the theory that nursing is no longer deemed an attractive or affordable career option, and drives long-term concerns for safe staffing, patient safety and service delivery.
The RCN employment survey in October 2021 found that 75% of nursing staff were regularly working beyond their contracted (paid) hours at least once per week, with 17% doing this daily (RCN, 2021). Only one in four shifts was staffed sufficiently with nurses, with 83% of nurses reporting insufficient staffing to meet patient needs (RCN, 2021). This is unsustainable practice, and the intensification of work across the system and profession is leading to increased sickness absences for anxiety, stress, depression and other psychiatric illnesses, accounting for 20% of all reported sickness absence episodes in April 2022 (NHS Digital, 2022b).
The NHS in England is the largest employer in Europe, and the world's largest employer of highly skilled professionals (NHS England and NHS Improvement, 2019). Our NHS providers are expected to support and deliver the NHS Long Term Plan (NHS England and NHS Improvement, 2019), to invest in their workforce and support the wellbeing of staff, yet in practice this is hard to achieve with chronic underfunding and bureaucracy. These issues were only amplified with the impact of ‘Brexit’ as the UK removed itself from the European Union (EU), and applications to the Nursing and Midwifery Council register from the European Economic Area (EEA) for trained and highly skilled nurses, has dropped from 10 000 to around 1000 per year (Ciupijus et al, 2022). Ministers would argue they have made it easier to attract and recruit internationally trained nurses to compensate for the shortfalls after Brexit, but this is often a lengthy and costly process, and over the past 5 years almost 15 000 EEA-trained nurses and midwives left the NHS, with only a little over 4000 joining (Ciupijus et al, 2022), further highlighting the detrimental impact on NHS providers' ability to attract and retain nurses.
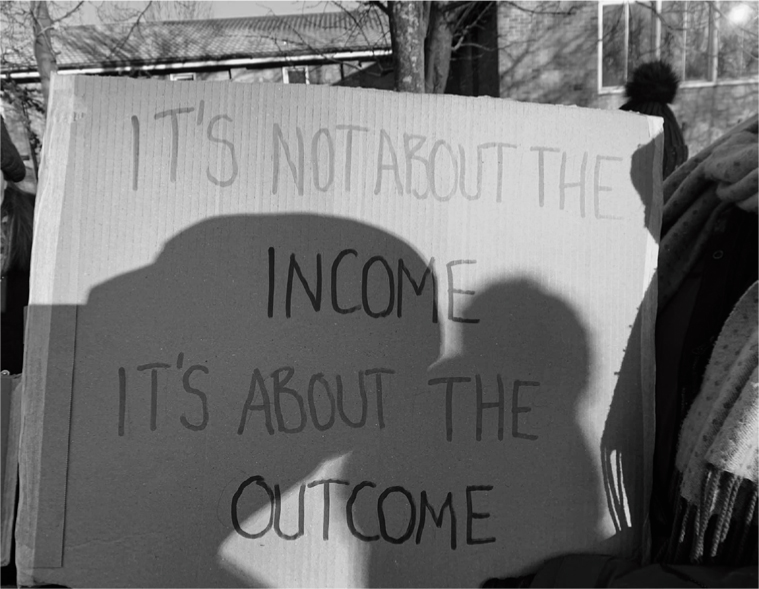
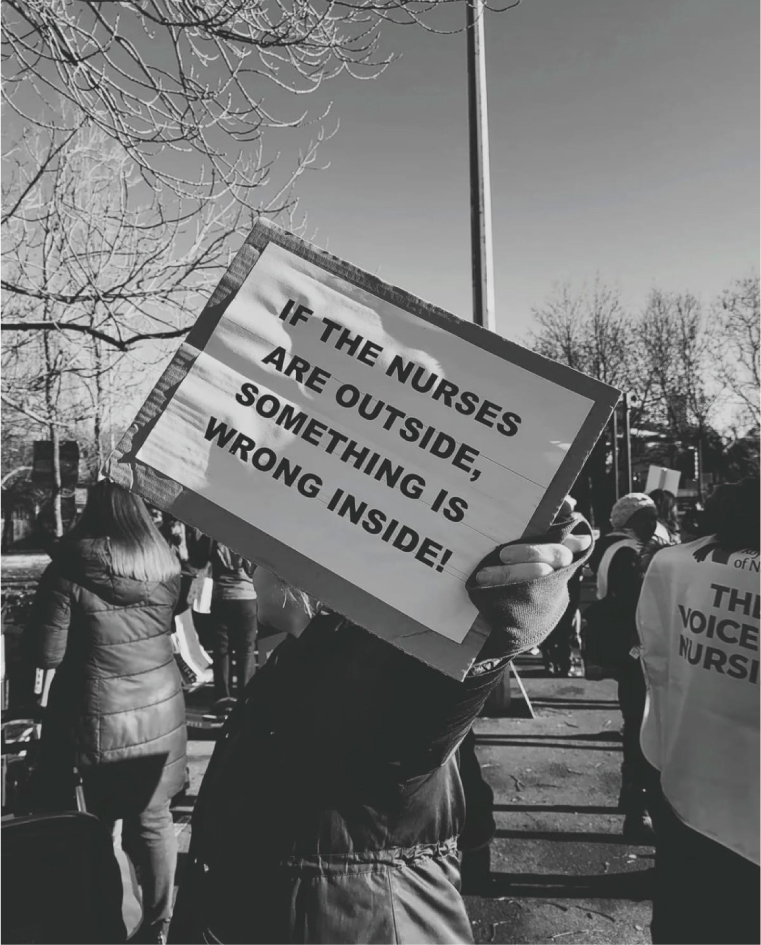
It is these daily safe staffing concerns, practice intensification pressures, recruitment and retention issues and long-term sustainability challenges, that are truly represented on the picket lines. Imagery from the first day of strikes clearly shared these sentiments, demonstrating the solidarity of our nursing workforce, to support each other and our patients. Many placards highlighted safe staffing concerns and amplified the drivers for much needed reforms. The government must not be complacent, ministers simply cannot keep scapegoating previous political party reforms, or blaming COVID-19 and austerity measures.
Despite the government's current position, existing NHS pressures and the inevitable impact on service delivery, public support for the RCN strike action has risen this year, with 64% of poll respondents supporting action, and 75% responding to suggest there are not enough nurses in the NHS to deliver safe care (RCN, 2022). This was felt on the picket lines too, with multiprofessional colleagues and members of the public attending to share warm drinks, donate food, talk, listen and cheer, with drivers and ambulances honking horns to show their support as they filed past.
It is imperative to understand that health professionals do not want to strike, but those who can, will. They will stand in solidarity with each other, for patients and for the NHS, ultimately demonstrating that if nurses are outside on the picket line, there is something very wrong inside.


