The incidence of urinary and faecal incontinence is increasing with the ageing population. It is estimated that the number of individuals living in the UK with urinary incontinence is approximately 14 million, with a further 6 million experiencing faecal incontinence (Royal College of Nursing (RCN), 2021; Bladder and Bowel Community, 2023). Although the incidence of incontinence is increasing, it should not be assumed that it will be a symptom of getting older (Goodman et al, 2013; Xu and Kane, 2013; Day et al, 2014; Schluter et al, 2017). Incontinence is one of the main reasons for care home admissions (Association for Continence Advice (ACA) Consensus Guidelines Group, 2021) and it is estimated that over 50% of care home residents have some form of incontinence (Leung and Schnelle, 2008).
The risk of incontinence increases with age and is a reason for care home admission (Schluter et al, 2017). It is important to remember that incontinence is a symptom, not a disease. The impact of incontinence on a person's quality of life has been found to be similar to that of diabetes or high blood pressure, affecting a person's independence, their productivity, sleep, and mental wellbeing (ACA Consensus Guidelines Group, 2021). Dignity and quality care are at the heart of continence care provision. Skilled and trained staff across health and social care communities are fundamental to delivering this (Rantell et al, 2016). Patients who have been identified with an incontinence issue should have a clinical assessment and an appropriate treatment/management plan implemented. Should the person be identified as having a clinical need for products to manage their incontinence, the emphasis shifts from that of treatment to that of management. The Guidance for the Provision of Absorbent Pads for Adult Incontinence: A Consensus Document (ACA Consensus Guidelines Group, 2021) recommends that incontinence products (also referred to as pads) should not be issued until a clinical assessment and a treatment programme has taken place.
The assessment and management of incontinence using containment products can be challenging for care home residents, nurses and care staff. For a resident, associated dermatitis is often a consequence (Boronat-Garrido et al, 2016), along with the risk of increasing morbidity (Damián et al, 2017) and an increased risk of developing a pressure ulcer (Gray and Guiliano, 2018). It can also lead to psychological consequences and decreased quality of life. For health professionals, urinary incontinence can contribute to an increased workload, as there are additional tasks such as changing disposable absorbent products or conducting behavioural interventions, for example, prompted voiding and toileting programmes. This also incurs higher costs than interventions associated with usual care (Wagg et al, 2017). Ostaszkiewicz et al (2016) also found that a care worker's self-identity was significantly affected by the stigma associated with managing urinary incontinence.
It is estimated that the NHS spends around £80 million per year on product costs (NHS England, 2018). Broken down, the monthly individual cost of products is estimated at £34.73 for products used during the day and £43.64 for night-time products. In addition, treating pressure ulcers costs the NHS more than £3.8 million every day (NHS Improvement, 2018).
It is clear from the available research and clinical evidence that there is the need for an appropriate assessment to identify the most suitable, cost-effective product to meet the resident's needs, without compromising on their care and dignity.
As advised in Guidance for the Provision of Absorbent Pads for Adult Incontinence: A Consensus Document, a clinical assessment should be completed by a qualified professional who can demonstrate the necessary theoretical knowledge, skills and expertise (ACA Consensus Guidelines Group, 2021). They are accountable for the choice of containment product, which should be based on the correct type and absorbency of pad that provides the best clinical outcome for the resident in terms of containment, skin health and personal dignity (Medicines and Healthcare products Regulatory Agency (MHRA), 2014).
To support the nurse with the clinical assessment and product choice, Attends developed the Attends Product Selector Tool in the late 1990s. This tool has since been developed to improve product effectiveness in-use. The Attends Product Selector Tool uses a simple scoring system based on activities of daily living and can be used as a guide for initial product selection (Table 1).
Table 1. Product selector tool
| Product assessment scorePlease complete by ticking the most relevant box under each category and adding scores at the end | ||||||||
|---|---|---|---|---|---|---|---|---|
| Mobility | Day | Night | ||||||
| Ambulant | 0 | |||||||
| Immobile | 1 | |||||||
| Walk with assistance | 2 | |||||||
| Communication | Day | Night | ||||||
| No problems | 0 | |||||||
| Difficulty | 1 | |||||||
| Non-communicating | 2 | |||||||
| Hearing/eyesight | Day | Night | ||||||
| No problems | 0 | |||||||
| Poor | 1 | |||||||
| Deaf/blind | 2 | |||||||
| Mental status | Day | Night | ||||||
| Fully alert | 0 | |||||||
| Slightly confused | 1 | |||||||
| Disorientated | 2 | |||||||
| Manual dexterity | Day | Night | ||||||
| Good | 0 | |||||||
| Restricted | 1 | |||||||
| Very limited | 2 | |||||||
| Toileting | Day | Night | ||||||
| Self-caring | 0 | |||||||
| Needs assistance | 1 | |||||||
| Fully dependent | 2 | |||||||
| Incontinence | Day | Night | ||||||
| Occasionally | 1 | |||||||
| Usually urinary/toileting programme | 2 | |||||||
| Doubly incontinent | 8 | |||||||
| Faecal only – Faecal Pad F6 Faecal smearing only – Insert Pads, Contours Regular 4/5 Faecal Incontinence/catheter or sheath in situ – Faecal Pad F6, Contours Regular 6/7 | ||||||||
| Frequency of urination | Day | Night | ||||||
| Less than 4 times | 6 | |||||||
| 4–7 | 4 | |||||||
| 8–10 | 2 | |||||||
| More than 11 times | 1 | |||||||
| Average void of urine | Day | Night | ||||||
| Less than 100 ml | 1 | |||||||
| 100–200 ml | 2 | |||||||
| 200–300 ml | 4 | |||||||
| 300–400 ml | 6 | |||||||
| More than 400 ml | 10 | |||||||
| Total score | ||||||||
| Product guide | ||||||||
| Score | Product choice | |||||||
| 3–11 | Soft 0–3, For Men level 1–3, Pull-Ons Discreet 3 | |||||||
| 12–18 | Contours Regular/Air Comfort 4/5/6, Soft 4/5/6, For Men Level 4, Pull-Ons 4/6, Lady Night 6 | |||||||
| 19–34 | Contours Regular/Air Comfort 7/8/9, Soft 7, Slip Regular 8/9, Slip Active 8/9, Pull-Ons 8, Flex 8/9 | |||||||
| 35+ | Contours Regular/Air Comfort 10, Slip Regular 10, Slip Active 10, Slip Classic 10, Flex 10, Adjustable 10, Pull-Ons 10 | |||||||
Currently, the Attends Product Selector Tool is used successfully by nursing staff and health professionals throughout the NHS and independent care, supporting product selection and forming part of their product requirement for ordering products.
The purpose of this observational study was to:
- Review and understand how effective the Attends Product Selector Tool is when used to assess a resident for an appropriate disposable incontinence product
- Select the correct type and absorbency of containment product to be used
- Review product usage and effectiveness.
The study
Before commencing the study, verbal consent was obtained from the three care home management teams for the Attends observer to review the assessments and the used products. There was no patient contact throughout the study. The three care homes belonged to the same care home group:
- Home 1: 61-bed care home, consisting of nursing, dementia, and residential care
- Home 2: 32-bed care home, consisting of nursing, dementia, and residential care
- Home 3: 53-bed care home, consisting of nursing and dementia care.
Staff from homes 1 and 3 who had previously received formal training completed the residents' assessments using the Attends Product Selector Tool. Home 2 was a new acquisition to the care home group and although the residents had assessments completed, they had not been updated to reflect current needs.
Method
During the 48-hour study period, the care home staff collected the used products in a labelled bag and the Attends observer visited the homes regularly during the evaluation period to collect the data and to weigh the products to ascertain the voided volume. Data collected included:
- Product name and absorbency level
- If a shaped pad was used, was it used in conjunction with Stretch Pants?
- The date and time the product was removed
- If the product contained urine, faeces, or both
- The weight of the product
- If the product had leaked
The Attends products used in the study have all been through the ISO 11948-1 (Rothwell) process, which is the industry standard for measuring the performance of disposable body-worn incontinence products. It measures the total absorption capacity of the product using weight in a laboratory environment. However, the test and this observational study do not reflect the in-use experience for users of disposable products or the benefits of product features, for example core technology, acquisition layers and leakage barriers, which are all features that help to reduce the risk of leakage from a product and help to keep the skin dry.
Findings
During the study period, 316 products from 92 residents were observed - 36% of the products were from male residents and 64% were from female residents. 246 products contained urine only, 70 products contained both urine and faeces or faeces only. Products containing faeces were not included in the study.
All the products observed were designed to manage heavy urinary incontinence and/or faecal incontinence, therefore demonstrating that the clients were assessed as being heavily incontinent or doubly incontinent.
- 76% of the residents used Attends Contours Regular in combination with Attends Stretch Pants
- 21% of the residents used Attends Slip Regular
- 3% of the residents used Attends Pull-Ons
Even though the residents in the study had been assessed as requiring a heavy urinary incontinence product, the average volumes of urine in the products did not reflect the amount of urine the pad can absorb. Table 2 shows the minimum, maximum and average volume of urine in the changed pad. This is expressed as ‘load’, where 1 gram (g) of load is equivalent to 1 millilitre (ml) of fluid.
Table 2. Urine load of observed changed products
| Product name | Minimum load | Maximum load | Average load |
|---|---|---|---|
| Attends Contours Regular 7 | 21 g | 346 g | 174 g |
| Attends Contours Regular 8 | 9 g | 619 g | 213 g |
| Attends Contours Regular 9 | 11 g | 950 g | 290 g |
| Attends Contours Regular 10 | 12 g | 216 g | 123 g |
| Attends Slip Regular 8 Medium | 111 g | 350 g | 230 g |
| Attends Slip Regular 8 Large | 12 g | 567 g | 221 g |
| Attends Slip Regular 9 Medium | 8 g | 326 g | 141 g |
| Attends Slip Regular 9 Large | 33 g | 567 g | 191 g |
| Attends Slip Regular 10 Large | - | - | - |
| Attends Slip Regular 10 Ex Large | 280 g | 609 g | 485 g |
| Attends Pull-Ons 6 Medium | 9 g | 389 g | 149 g |
The products with minimum volumes of urine (less than 33 g) tended to be the products changed in the morning when residents were being washed and dressed, even though the product had recently been changed by the night staff. This highlighted that staff were not using the wetness indicator to check if the product required changing. An explanation for this was that ‘it's routine practice to put a new pad on when dressing’, rather than a need-based approach. This therefore increases staff workload and product costs.
By ensuring that there is a focus on an individual's product needs, professionals can also take steps to protect the environment. For example, choosing the correct type of product helps to reduce waste, and using products to their maximum capacity reduces the burden on the planet.
Throughout the observational study, 48% of products observed were being changed before they had reached their full capacity. This was due to the care home staff changing the resident's continence products before they had reached their full capacity and not all residents always used their prescribed product.
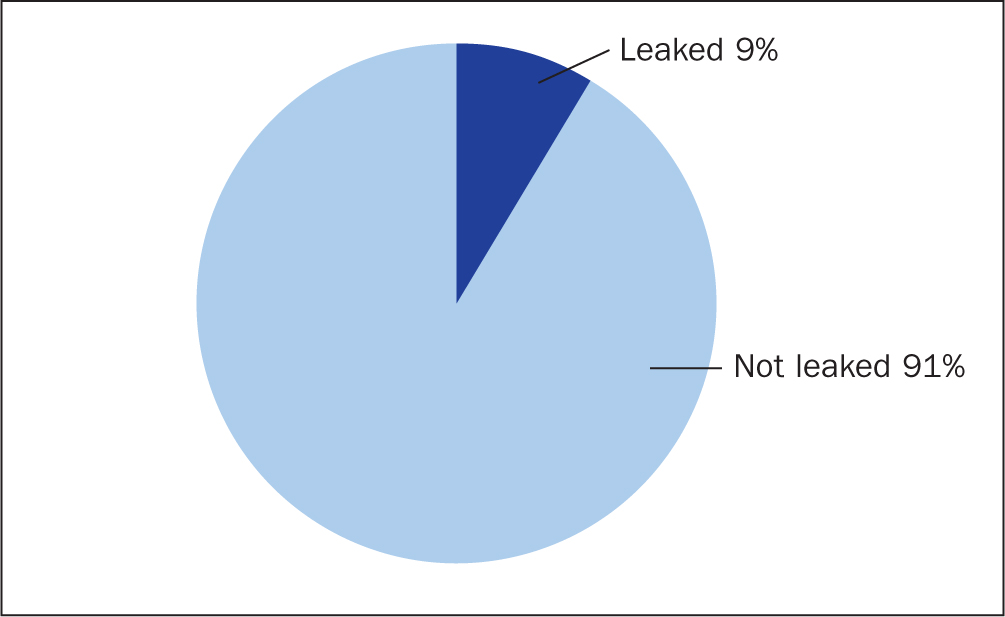
It was also interesting to note that out of the 316 products observed, only 28 (9%) had leaked (Figure 1). A common cause of a product leaking is an incorrect size being selected or choosing the wrong absorbency level. Throughout the study, it was acknowledged that some residents were not using their assessed products, which could have had an impact on leakage. From observing the style of products used, only 34% of the residents included in the evaluation were consistently in their prescribed products, for example, a lower absorbency. Incorrect product sizes or alternative products were being used, which could have an impact on leakage and skin moisture.
At the time of this evaluation, the home staff reported no skin issues or deterioration in Braden Scale scores (for pressure ulcer risk), even though inappropriate use of too high or too low an absorbency can contribute to an increased risk of skin damage (Holroyd, 2021).
Although the fitting of the products was not observed by the Attends observer, the low levels of leakage may also be attributed to the correct fitting of the products by staff. This may be as a result of initial training provided to staff, which included product assessment, product selection and hints and tips on fitting eg the use of the correct size of Attends Stretch Pant with Attends Contours Regular (two-piece system) and correct sizing and fitting for the all-in-one product category. In addition, educational material (product fitting guides and fact sheets) was provided to reinforce the training and for new and agency staff to read until formal training was provided.
The recommended average change rate is four products per day (ACA Consensus Guidelines Group, 2021). During the study, not all products were saved so it was difficult to determine an accurate change rate. An explanation given for this was ‘not all staff were aware that all used products needed to be saved over the 48-hour period’. However, this was addressed following discussions with the staff. Based on the individual resident data collected and feedback from nursing staff on when the pads that had not been saved were changed, it was evident the change rates were within the recommended four products each day.
Conclusions and recommendations
The Attends Product Selector Tool was effective in enabling staff to select an appropriate type of containment product. However, when it came to selecting the absorbency, the assessor tended to choose a higher absorbency rather than starting at the lower absorbency in the product guide range. The results demonstrated the products were effective if used appropriately. Not all residents were using their assessed products, which occurred mostly at night, and only 9% of the products leaked. However, it is evident that work needs to be undertaken with the homes to change staff practice, for example, using the wetness indicator to determine a product change, rather than following routine practice. Further education needs to be given to staff to encourage them to initially select a lower absorbency pad when they review the product choices available.
Staff should apply the correct product that the resident had been prescribed to better manage their clinical needs. This will also support the cost-effective management of incontinence in care homes. Nursing staff also need to be aware that a containment product is classified as a medical device (MHRA, 2014) and therefore its safety and fitness for purpose is fundamental in achieving quality care. Fortunately, during the study there was no documented changes in skin issues or deterioration in Braden Scale scores, however, inappropriate product use increases the risk of skin damage (Holroyd, 2021).
Due to the high rates of staff turnover and agency staff being unfamiliar with the Attends Product Selector Tool and the assessed products for the individual residents, ongoing product training is essential (Castle, 2009). This training should include information regarding the product range available, hints and tips on fitting the products, when products should be changed, use of the wetness indicator and the knowledge that the product can be reapplied if it contains small amounts of urine.
As a result of the study, to help provide a holistic approach to continence care, ‘continence champions’ have been introduced into the care homes. Evidence has demonstrated that continence champions are effective in change implementations (Miech et al, 2018). Continence champions are nurses or senior healthcare assistants who have been given additional product training to oversee the assessment and the management of incontinence, using the Attends range. They are responsible for answering questions about the Attends product range and appropriate use. The continence champions are also involved in keeping the Product Selector Tool up to date, ensuring that the prescribed products are being used in an effective way with the support of the Attends team if required.
KEY POINTS
- It is estimated that over 50% of care home residents have some form of incontinence
- Health professionals are accountable for the choice of containment product, which should be based on the correct type and absorbency of pad that provides the best clinical outcome for the resident in terms of containment, skin health and personal dignity
- Using the Attends Product Selector Tool helps staff select an appropriate and effective containment product following a continence assessment
- The Attends containment products are shown to be effective if used appropriately
CPD reflective questions
- How do you assess for containment products in your workplace?
- Why is it important to assess residents for containment products?
- If inappropriate containment products are used, what consequences will this have?
- How will this study help improve your practice?


