Incontinence, the involuntary leakage of urine, faeces or both, is a common and burdensome condition, especially for older adults. If not handled appropriately, it can have a significant negative impact on their physical, social and psychological wellbeing (Minassian et al, 2003; Abufaraj et al, 2021). Incontinence is a globally recognised issue that contributes to significant social and economic costs (Kanerva Rice et al, 2018). Incontinence-associated dermatitis (IAD) refers to skin injury and inflammation that occurs as a consequence of prolonged exposure of skin to urine, stool, or both (Beeckman, 2017; Wang et al, 2018). Various factors such as chemical irritants in incontinence, changes in skin surface pH and microorganisms are considered to negatively impact the skin and contribute to IAD (Beeckman, 2017).
Prolonged skin contact with moisture due to incontinence results in stratum corneum damage. The main function of this layer is to protect the skin from microorganisms, heat, abrasion and chemicals (Ersser et al, 2005; Van Damme et al, 2018). A healthy skin surface is acidic, with a pH of 4–6, providing resistance to bacterial invasion and colonisation (Ersser et al, 2005; Mugita et al, 2021). However, a variety of factors, such as skin moisture, sweat and anatomical site, can affect skin pH (Falloon et al, 2018). An increase of pH to an alkaline level can disrupt the skin barrier and deteriorate the so-called acid mantle of the stratum corneum (Shigeta et al, 2009).
Several interventions have been implemented to exclusively treat the cause or manage incontinence. Absorbent continence products of different sizes, shapes and absorbencies are frequently used to manage incontinence (Chartier-Kastler et al, 2011). There is wide variety of absorbent continence products on the market. However, the extensive range of products can be confusing for patients, caregivers and professionals when choosing the most appropriate product (Knifton et al, 2018). Moreover, the literature contains inadequate information on product descriptions and performance to aid users to select the most appropriate product for each individual.
It is necessary for healthcare providers to match patients with suitable and effective absorbent continence products (Kanerva Rice et al, 2018). Urinary incontinence and incontinence care routines, including changing the continence pad frequently, are contributing factors to disrupted sleep in older patients with dementia and nursing home residents (Ouslander et al, 1998; Schnelle et al, 1998). In addition, changing continence pads several times a day can be burdensome for caregivers (Arkan et al, 2018).
Appropriate products, which have a high absorption capacity and wicking properties, can efficiently transport and distribute moisture throughout the product, resulting in a dryer skin micro-environment. These characteristics promote a healthy microclimate between the absorbent product and the skin and minimise skin occlusion. Maintaining a normal skin pH also plays an important role in protecting the skin from the irritating effects of urine and faeces. The continence product must be able to absorb urine at the highest possible flow rate and retain urine without leaking until it is changed. Malodour control and the softness of a product provide comfort and prevent unnecessary changes. This allows patients with incontinence to sleep better, and also reduces sleep disruption and fatigue during the day. In addition, using the right product will enable healthcare providers to save time required for daily care routines; this will reduce workload, leaving more time for care activities (Van Gysel et al, 2012; Bliss et al, 2017; Buckley, 2019; Sayabalian et al, 2019). Ease of opening the packaging and applying the product are also important features, especially for individuals who may have dexterity and mobility difficulties (Getliffe et al, 2007).
This study investigated the perception of continence care nurses in a care home setting regarding their experience of using MoliCare Premium Form products for patients with incontinence.
Methods
Study design
Nurses from 11 nursing facilities caring for patients with incontinence (urinary, faecal, or both) and/or dementia in Germany successfully completed this study. The nursing homes were approached by medical advisers, who identified the appropriate living areas in the homes, to ensure the survey covered the relevant population of residents, that is, those using continence products with the absorbency that the authors wanted to test. A total of 74 nurses working across different shifts participated in the study.
The nurses were provided with MoliCare Premium Form products, and the product manufacturer's continence advisors attended the homes to demonstrate the correct usage and fitting of the products. The nurses then tested the products with residents for about 1 week.
A quantitative survey was developed and administered to the staff to elicit their views on the use of MoliCare Premium Form products. The survey consisted of statements about the significant features of absorbent continence products. The questionnaire was administered to two nursing cohorts (n=35 and n=39), with additional feedback on product characteristics requested of nurses who took part in the first round of the survey.
The study complied fully with ethical, governance and data protection requirements.
Development of the survey
Both rounds of the survey (n=35 and n=39) included a brief introduction, which described the changes and modifications in the design features and materials of the new MoliCare Premium Form product. Information on the name of the institution, type of nursing shift and special characteristics of the residents (eg faecal incontinence, dementia and medication) was collected. In the first round, the introduction was followed by 10 statements relating to features of product performance, each of which nurses were asked to rate in order of importance. The statements were based on aspects identified from a literature review and the significant factors that influence whether products are considered effective or acceptable by users (Getliffe et al, 2007; Buckley, 2019). The second round of the survey (n=39) did not include these 10 statements for nurses to rank.
For the statements shared across both rounds (n=74), nurses were asked to rate their level of satisfaction with each statement on a scale of 1-5, where 5 was the highest possible level of satisfaction, and 1 the strongest level of dissatisfaction. Respondents were also asked to answer four statements to evaluate the product packaging, and five statements were designed specifically to compare the new MoliCare product with the previous design in terms of performance and user preference.
The ratings were combined into three categories: ‘good’/’agree’ (combined from 5 and 4 on the Likert scale) to indicate that the product worked well and the nurses would like to continue to use it; ‘OK’/’neutral’ (3 on the Likert scale) indicating that the product was thought to work fairly well and that the respondents would consider using it; ‘and poor’/’disagree’ (2 and 1 on the Likert scale) to indicate that the product did not meet expectations and the nurses would not wish to use it again.
MoliCare Premium Form products
The design and materials of the absorbent core used in the product were changed to promote skin dryness and maintain an acidic pH at the surface of the continence pad. The initial design used curled fibre, a specially processed type of cellulose fibre, which was modified in an acidic citric environment and introduced between the top skin-facing layer and the absorbent core. Beneath this layer, a normal cellulose and super absorbent polymer matrix absorbs and holds fluid to keep moisture away from the skin (Beguin et al, 2010). However, this specific cellulose type (curled fibre) increases costs and is difficult to introduce into the manufacturing process.
The key feature of the new design (Figure 1) is the acquisition distribution layer (ADL), which is composed of non-woven fabric placed underneath the top sheet. The ADL facilitates the thorough distribution and penetration of the liquid into the inner core of the continence pad and prevents the moisture returning to the top sheet under external pressure. Beneath the ADL, normal cellulose, supplemented with super absorbent polymer, locks in the moisture and prevents the liquid from re-wetting the skin. The cellulose-containing layer above the backsheet helps utilise the entire amount of super absorbent polymer within the absorbent core and distributes the fluid within the continence pad over a wider area.
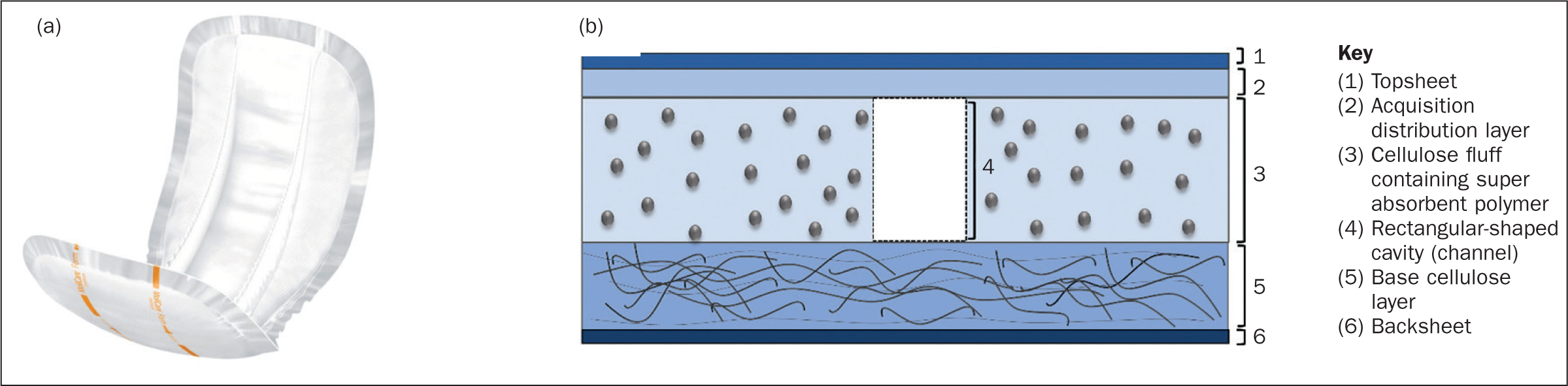
The product has been modified with monosodium citrate to create an acidic surface environment when wet. Another key design element is the inclusion of channel-shaped cavity in the pad at the most probable urine entry point. This further accelerates urine absorption through the quick and even distribution of liquids throughout the pad. Figure 1 illustrates the new design.
Data analysis
All descriptive statistical analyses were performed using SPSS v27.0 (IBM Corp, Armonk, New York, USA).
Findings
Evaluation of absorbent product features
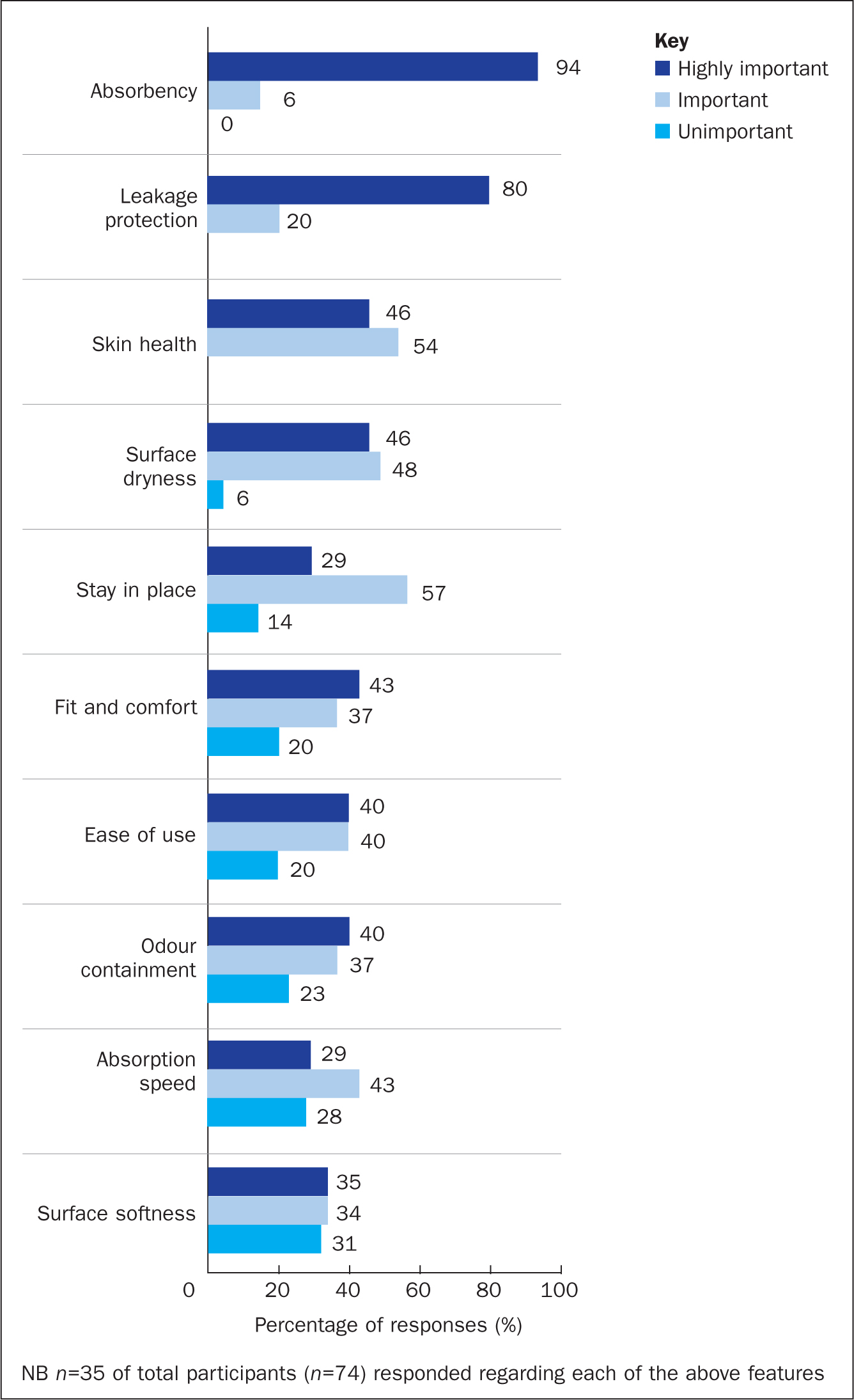
Figure 2 represents the first round of responses (n=35) from nurses who were asked for additional feedback, who ranked the key product performance features in terms of importance. From the respondents' perspective, product absorbency was the most important feature: this was rated as ‘highly important’ (94%), followed by leakage protection (80%). The two next ‘highly important’ features, rated by 46% of nurses, were maintenance of skin health and surface dryness. The ability to stay in place was also seen as a ‘highly important’ or ‘important’ factor for most respondents (86%). About 80% of nurses considered wear comfort, ease of use and odour containment as ‘highly important’ or ‘important’ features. From the nurses' point of view, absorption speed and surface softness were slightly less important than the other characteristics.
The evaluation of the key aspects of product performance by nurses is presented in Figure 3. This figure combines the feedback from both cohorts (n=74). Figures 4–6 also combine responses from both rounds of the survey.
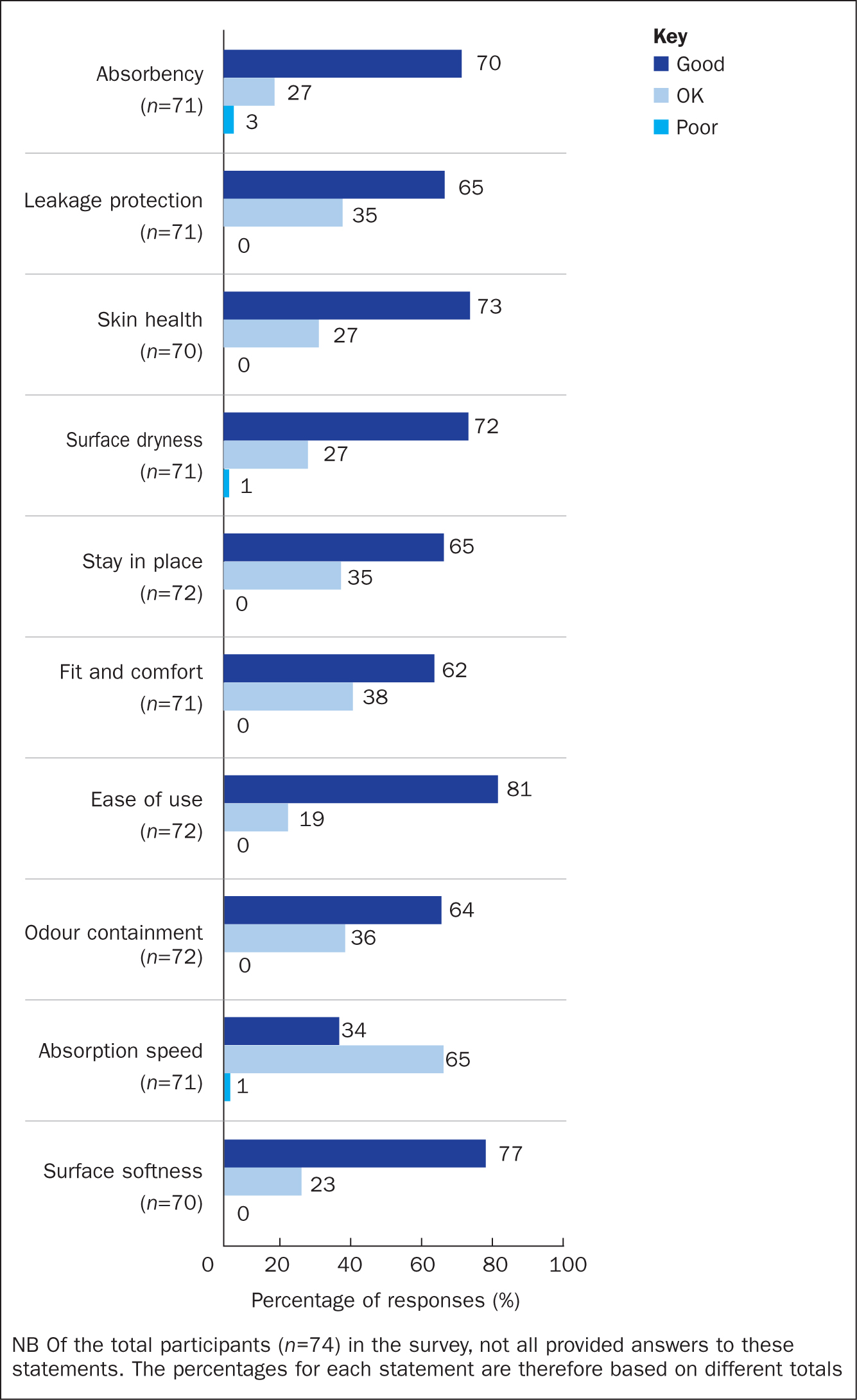
Most product features received a ‘good’ rating from the majority of nurses (ranging from 62% to 81%), with less than 3% of respondents rating any of the features as ‘poor’. Specifically, 1% rated surface dryness and 1% absorption speed each as ‘poor’. The absorbency of the product was rated ‘good’ by 70% of caregivers, and just 3% as ‘poor’. None of the other features was rated as ‘poor’. Almost 65% of respondents rated leakage protection, the product's ability to stay in place and odour containment as ‘good’, while the rest considered these features to be ‘OK’. Around three-quarters of the nurses found the ability of the product to maintain healthy skin and surface dryness to be ‘good’. The ease of use of the product was rated as ‘good’ by the highest proportion of nurses (81%). Most respondents (62%) rated the product as comfortable to wear, with less than half rating it product as ‘good’ in terms of absorption speed (34%); 77% rated surface softness as ‘good’.
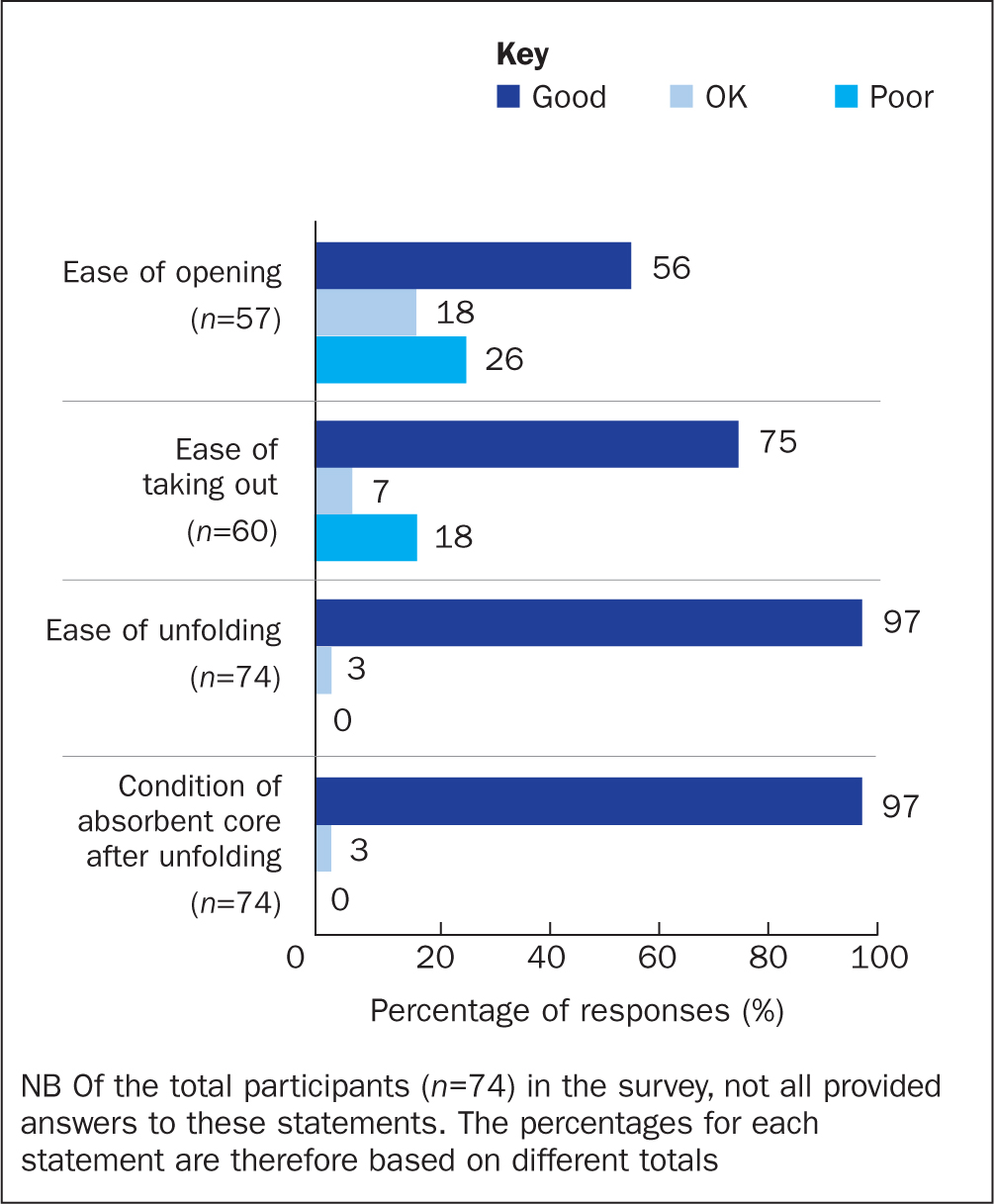
Figure 4 shows the percentages of participants who evaluated the packaging and handling of the product after opening the package. More than 70% of the nurses found opening the packaging and taking out the product easy, rating these features as ‘good’ and ‘OK’. The product was considered to be easily unfolded, and 97% of respondents rated the condition of the absorbent core after unfolding as ‘good’.
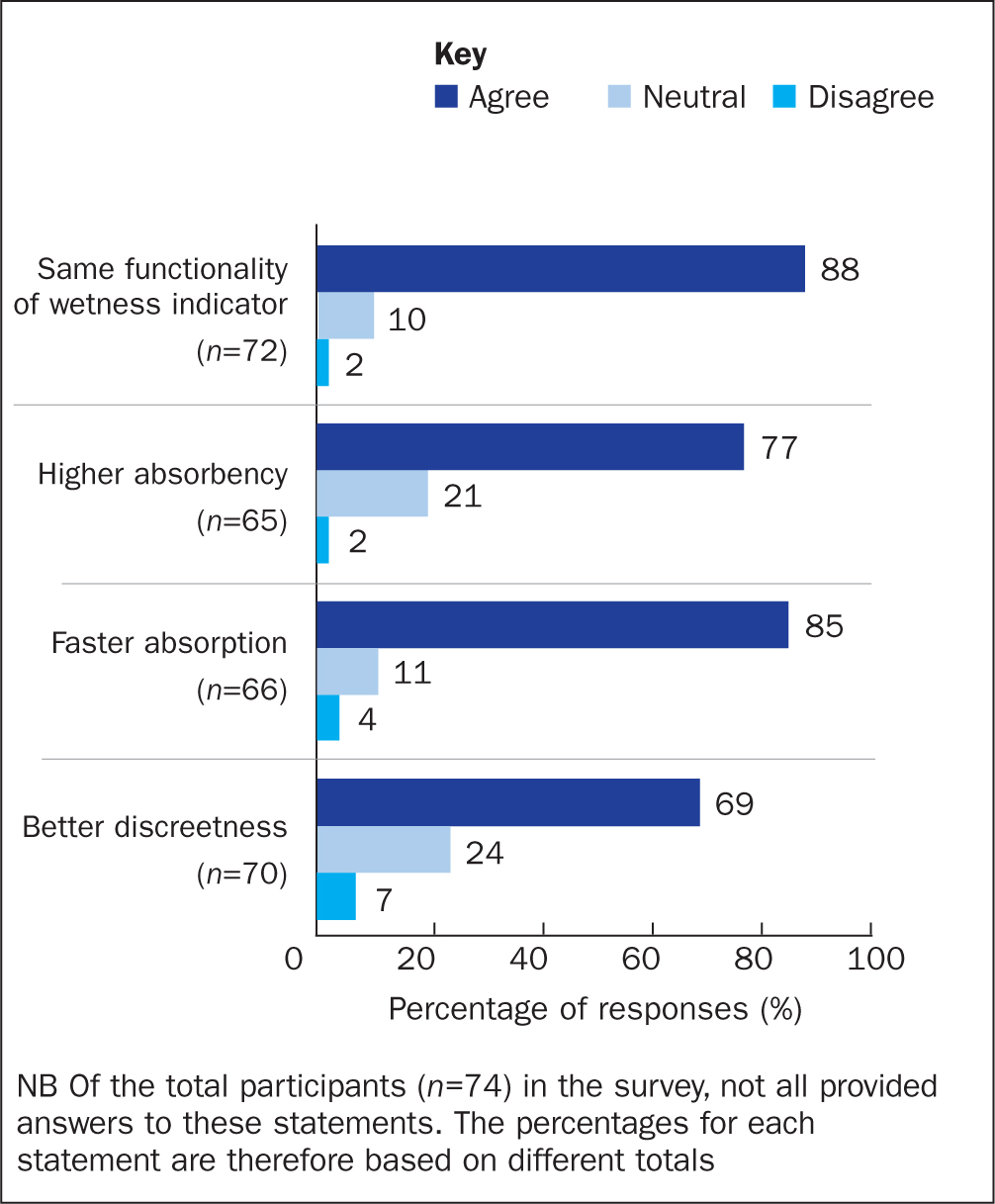
The nurses were also asked to rank whether certain aspects of the new MoliCare pad with optimised design and materials performed better than the old product. They also responded to one statement regarding their overall preference for either the new or old product designs (Figure 5 and Figure 6). The wetness indicator of the new design was considered to perform as well as the previous design by 88% of respondents; 77% agreed that the new product design performed better in terms of absorbency and retaining urine. The new MoliCare design was considered to have faster absorption speed, with 85% of the nurses agreeing with this. Finally, 69% of them considered the new product design to have better discreetness (Figure 5).
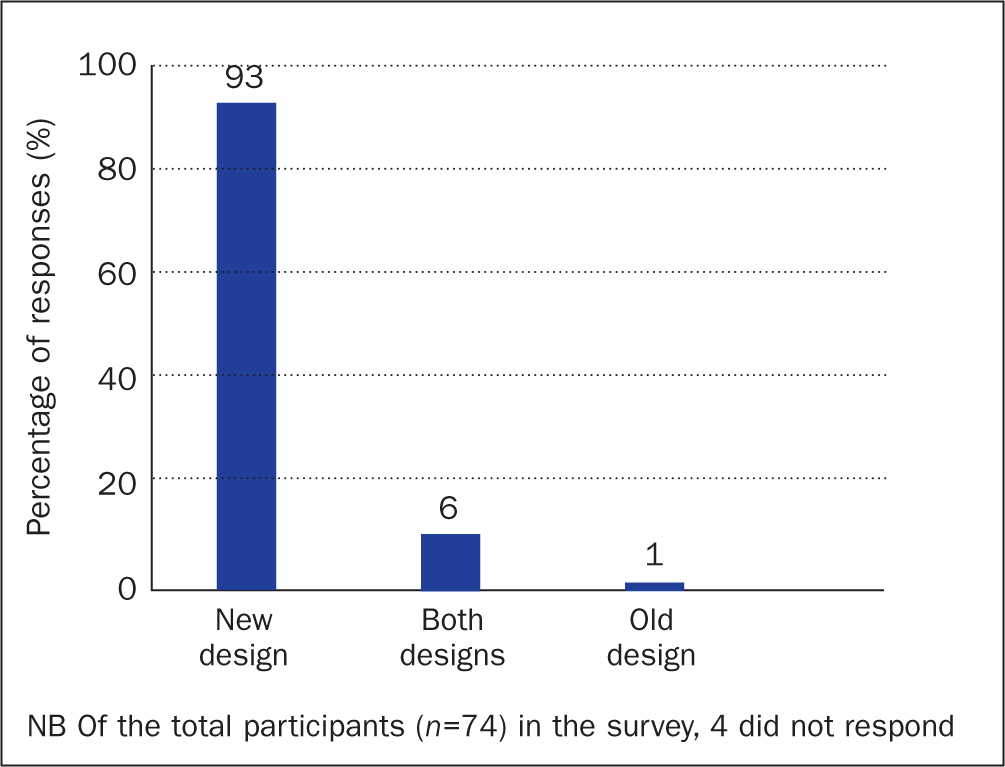
When nurses were asked to rate their preference for either the new or old product, 93% preferred the new MoliCare design over the previous version, 6% preferred both product designs, and only 1% voted for the previous MoliCare Premium Form design (Figure 6).
Discussion
Bladder and bowel dysfunctions can have a huge impact on an individual's quality of life, both practically and psychosocially. A wide variety of products is available to manage continence complications, with disposable absorbent pads being the most commonly used products to manage urinary incontinence (Buckley, 2019). Different factors in the design and features of an absorbent product can influence product effectiveness and acceptability. The authors developed a new MoliCare absorbent continence product with optimised design and features. Several improvements were made to meet the preferences of incontinence patients. The authors then conducted an in-use study to assess the key characteristics of product performance, developing a survey to help explore the perceptions of nurses in working in residential care homes regarding their experience of using both the old and new product designs.
The absorbency and leakage protection of an absorbent product are among the most important aspects of its performance. A continence product should absorb and contain urine without leakage, which can be achieved by using a special absorbent core design and sufficient absorbent materials in the correct place. Improved technology in the absorbent core of the new design of the MoliCare continence pad helps provide adequate absorbency and leakage protection.
The harmful effects of prolonged skin exposure to excessive moisture due to incontinence are a common health problem encountered in various care facilities (Voegeli, 2012). An increase in skin pH to alkaline level can disrupt the skin barrier and deteriorate the acid mantle, causing the skin to become more permeable to chemically irritating substances such as urine and faeces (Shigeta et al, 2009). In addition, increased skin wetness leads to an increased susceptibility of the skin to abrasion damage owing to higher friction against the skin, and to microbial growth (Dhiman and Chattopadhyay, 2022). Therefore, absorbent continence products should minimise skin wetness and keep it as dry as possible. The modification of MoliCare absorbent product provides an acidic pH surface adapted to the physiology of the skin's epidermal barrier, which helps maintain healthy skin (Beguin et al, 2010; Bliss et al, 2017). When incorporated within the design of a continence product, the ADL can contribute to providing ‘improved dryness’ by facilitating fast absorption and the distribution of urine to deeper layers of the continence pads, preventing fluid from returning to the surface of an absorbent product when subjected to pressure (Helmes et al, 2014).
The optimised product has been ergonomically designed to improve its fit, allowing the user to feel more comfortable and secure. The ability of an absorbent continence product to remain in place is an important feature because users can feel anxious owing to the risk of the pad moving and possibly leading to leakage (Buckley, 2019). Other important features for people who experience continence problems are the comfort and discreetness of absorbent products. In general, well-fitted products are more comfortable, absorb urine more efficiently and prevent leakage.
Odour containment is another important consideration for those who rely on continence products. Users assume that the smell of urine indicates that they are wearing absorbent continence products which will affect how others see them (Buckley, 2019). According to the rating by the survey respondents, based on the nurses' perceptions for this feature, the MoliCare product neutralised odours very well, and the smell of urine did not seem to be a problem with usage of this product.
Ease of use and handling of the pad after opening the package are of great importance to both patients and their caregivers. The packaging of some continence products is difficult to open, and the product itself is not easy to use for people who have limited dexterity (Getliffe et al, 2007; Buckley, 2019). Owing to the poor perforated region, the packaging was not ranked highly by users. If opened incorrectly, users found it difficult to easily remove each pad, potentially requiring extra force to take it out. Following the findings of the survey, which made this problem apparent, improvements were made to the packaging design to solve it. Artwork has been added, aiding users to cope better with continence issues, and promoting a greater degree of independence.
The new MoliCare Premium Form outperformed the old design in several aspects, and the majority of nurse respondents preferred using the new product, perhaps because of its optimised design and the materials.
Limitations
The current study was limited to the views of nurses assessing the MoliCare absorbent continence products for patients in 11 nursing homes. A larger sample size and demographic details of the residents involved in the trial would have been beneficial and added to the understanding of nurses' and users' views on using the product. However, as an early evaluation of the product, the authors considered that the nurses' feedback on the new design would be sufficient, so ethical approval to gather such data was not obtained.
Conclusion
This study has shown that the new design of the MoliCare Premium Form performed extremely well on each of the individual key performance features and outperformed the old design, demonstrating the high quality of the product. The new design with specific features and materials has shown its ability to meet the needs of patients and carers and fulfil the usability criteria for choosing absorbent continent products.
The high level of satisfaction with various continence pad performance features suggests that the redesigned MoliCare Premium Form product is highly suitable and effective for patients with continence problems.
KEY POINTS
- Improved technology in the absorbent core of the MoliCare Premium Form helps provide better absorbency and leakage protection
- The new design provides ‘improved dryness’ and prevents fluid from returning to the surface of an absorbent product when subjected to pressure
- The acidic pH on the surface of the MoliCare Premium Form supports the epidermal barrier function and may help reduce the occurrence of incontinence-associated dermatitis
- The new MoliCare design performed well on each key performance feature and outperformed the old design, demonstrating the product's high quality
CPD reflective questions
- What are the key performance characteristics of an absorbent continence product?
- What are the consequences of using an inappropriate absorbent continence product?
- How will this study help you in choosing the right continence product?


