Many people living with a stoma struggle with psychosocial and physical problems after stoma surgery, with leakage of stomal effluent and peristomal skin complications (PSCs) among the most common stoma-related issues experienced (Fellows et al, 2021; Jeppesen et al, 2022).
Although the term ‘leakage’ is widely used, there is no standard definition for this, and understanding of the term varies between users and health professionals (Down et al, 2021). Nafees et al (2018) suggested distinguishing between two broad definitions of leakage, ‘leakage underneath the baseplate’ and ‘leakage outside the baseplate’.
In a recent international survey, 65% of people living with a stoma had experienced leakage of effluent outside the baseplate at least once in the previous year and 26% had experienced this monthly (Martins et al, 2022). Another study found that leakage issues continued to be a problem from the early postoperative period to several years after surgery (Pearson et al, 2020). Leakage of stomal effluent progressing outside the baseplate (eg onto clothes or bed sheets) can be socially embarrassing, is often distressing and is always inconvenient for the individual to experience, with more than 90% of people living with a stoma worrying about leakage (Claessens et al, 2015; Jeppesen et al, 2022). Leakage of stomal effluent and the worry thereof have a significant negative impact on people's quality of life (QoL), especially when effluent progresses outside the baseplate, soiling clothes or bedsheets.
Despite innovations in stoma care products (pouching systems and supporting products), leakage of stomal effluent continues to be a problem for many people living with a stoma (Aibibula et al, 2022; Martins et al, 2022). It has consequently been ranked as the top research priority within stoma care, ie to develop solutions to reduce the risk of developing PSCs or experiencing incidents of leakage outside the baseplate (Hubbard et al, 2017).
Access to specialist stoma care nurses is important in reducing leakage-related complications (Aibibula et al, 2022). Guidelines are available for the assessment and treatment of people with a stoma for the selection of appropriate stoma care products based on the individual's body profile (Colwell et al, 2019). Nonetheless, 3 out of 10 people with a stoma in an international survey reported that they did not have access to stoma care nurses as needed and, of those who did, 1 in 4 never took the opportunity to consult one (Martins et al, 2022). Additionally, more than one-third never had a body profile assessment to establish if the pouching system (stoma bag and baseplate) currently used was still the optimal product to fit their body (Martins et al, 2022). Another study found that 2 out of 10 people experiencing stoma-related complications did not seek help from anyone (Richbourg et al, 2007), indicating that a significant proportion suffer in silence.
The psychosocial and physical problems associated with leakage have been investigated at individual level for people with a stoma (Jeppesen et al, 2022). However, the way the experience of leakage progressing outside the baseplate affects people's use of stoma care products and their likelihood of consulting a health professional to mitigate the risk of future leakage incidents remains inadequately understood. In the present study, the authors investigated how incidents of leakage outside the baseplate affected the use of pouching systems and supporting products, as well as interactions with health professionals during periods of leakage-related issues. The behavioural changes following such leakage incidents were used to estimate the cost of such events to the healthcare system.
Methods
The survey was conducted in 2021 as an online, retrospective, self-reported questionnaire developed by Coloplast. The survey was sent to members of the Coloplast Online Research Engine (CORE) survey panel (representing the UK, USA, France, Germany, and Denmark), consisting of people aged over 18 years with a stoma.
The survey contained questions regarding demographics and stoma characteristics. Participants were subsequently asked questions about the number of leakage incidents outside the baseplate (in the past 2 weeks and 3 months), and the consequences thereof, ie use of consultations with health professionals (nurses and general practitioners), as well as changes in the use of pouching systems and supporting products. Questions related to the consequences of leakage outside the baseplate were only asked of respondents who had experienced at least one leakage incident outside the baseplate in the preceding 3 months. Every question concerning the consequences of leakage outside the baseplate had predefined response options, which are highlighted in the tables and figure accompanying the article.
This analysis focused solely on leakages outside the baseplate for people living with a colostomy or ileostomy. The impact of urinary leakage was outside the scope of this investigation.
Ethical approval and consent
Before accepting to join the CORE panel and taking part in the survey, all participants consented to taking part and allowed Coloplast to use the data collected in an aggregated and anonymous representation for internal and publication purposes.
Cost analysis
The cost per event of leakage outside the baseplate was estimated based on the reported increase in healthcare resource utilisation related to experiencing leakages outside the baseplate and based on UK unit pricing. Costs were calculated based on the outcomes of visits to health professionals, and the increased use of pouching systems and supporting products in the respondent's routine following a leakage event. The costs of interactions with health professionals were calculated using the weighted responses of participants and the costs of nurse and GP consultations taken from NHS reference costs (NHS England, 2021) and the Unit Costs of Health and Social Care from the Personal Social Services Research Unit (Curtis et al, 2019). The cost of pouching systems was derived using the manufacturers with the highest market share in the UK (Coloplast, Hollister, Salts, Convatec and Dansac), using the Prescription Cost Analysis (PCA) data available at the time of the study (NHS Business Services Authority, 2021). To simplify the calculation, the costing for all supporting products used in the calculation were from the same brand (Coloplast). Due to low overall cost variations between brands, this was considered to be a representative estimate.
Statistics
Descriptive statistics were conducted in Microsoft Excel and SAS JMP (v13.1.0 for Windows; SAS Institute Inc, Cary, NC).
Results
Demographics of respondents
A total of 2029 people living with a stoma from the CORE panel were invited to take part in the study, of whom 819 opened and started the survey. A total of 602 individuals with a colostomy or an ileostomy completed the survey, but six respondents were excluded because they reported having both an ileostomy and a colostomy. The remaining 596 individuals from five countries (USA: n=146; UK: n=158; Germany: n=154; Denmark: n=87; and France: n=51) were included in the analysis. Of the survey population, 53% were female; 84% were aged 50 years or older (Table 1). In terms of stoma type, 38% had a colostomy and 62% had an ileostomy. Most respondents (93%) had had their stoma for at least 5 years (Table 1).
Table 1. Demographics of respondents
| n | % | |
|---|---|---|
| Total number | 596 | 100 |
| Age | ||
| 18–29 years | 3 | 0.5 |
| 30–39 years | 35 | 5.9 |
| 40–49 years | 58 | 9.7 |
| 50–59 years | 136 | 22.8 |
| 60–69 years | 148 | 24.8 |
| 70 years or above | 214 | 35.9 |
| Do not wish to answer | 2 | 0.3 |
| Gender | ||
| Female | 315 | 52.9 |
| Male | 281 | 47.1 |
| Country | ||
| UK | 158 | 26.5 |
| USA | 146 | 24.5 |
| France | 51 | 8.6 |
| Germany | 154 | 25.8 |
| Denmark | 87 | 14.6 |
| Stoma type | ||
| Colostomy | 229 | 38.4 |
| Ileostomy | 367 | 61.6 |
| Time since surgery | ||
| 0–12 months | 8 | 1.3 |
| 1–2 years | 10 | 1.7 |
| 3–4 years | 21 | 3.5 |
| 5–10 years | 149 | 25.0 |
| >10 years | 407 | 68.3 |
| Do not wish to answer | 1 | 0.2 |
| Occupation | ||
| Retired | 349 | 58.6 |
| Working full time | 104 | 17.4 |
| Working part time | 57 | 9.6 |
| Sick leave | 10 | 1.7 |
| Unemployed | 23 | 3.9 |
| Other | 43 | 7.2 |
| Do not wish to answer | 10 | 1.7 |
Number of leakage incidents outside baseplate
Respondents were asked to recall the number of incidents of leakage outside the baseplate in the past 2 weeks, with a mean of 1.1 incidents of leakage outside the baseplate reported (Table 2). More than half (58.1%) had not experienced leakage outside the baseplate during this period, 19.3% had had a single incident, 10.1% had had two incidents, with the remainder (12.6%) experiencing three or more incidents of such leakage during the past 2 weeks (Table 2).
Table 2. The number of leakage incidents outside the baseplate
| Number of incidents | Past 2 weeks (n=596) | Past 3 months (n=595)* | ||
|---|---|---|---|---|
| n | % | n | % | |
| 0 | 346 | 58.1 | 211 | 35.5 |
| 1 | 115 | 19.3 | 113 | 19.0 |
| 2 | 60 | 10.1 | 83 | 13.9 |
| >3 | 75 | 12.6 | 188 | 31.6 |
| Total | 596 | 100.0 | 595 | 100.0 |
| Mean | 1.11 | 3.81 | ||
| Median | 0 | 1 | ||
| 5th percentile | 0 | 0 | ||
| 25th percentile | 0 | 0 | ||
| 75th percentile | 1 | 3 | ||
| 95th percentile | 5 | 12.3 | ||
| Maximum | 30 | 100 | ||
Respondents subsequently reported the number of leakage incidents outside the baseplate during the preceding 3 months. One individual was excluded due to an ambiguous response. Over this period, respondents on average experienced 3.8 incidents of leakage outside the baseplate (Table 2). About one-third (35.5%) had not experienced leakage outside the baseplate over this time, 19.0% had had a single incident, 13.9% had experienced two incidents, with the remainder (31.6%) experiencing three or more incidents of leakage outside the baseplate over the past 3 months (Table 2).
Worry about leakage outside the baseplate
Eighty-nine percent of respondents worried about leakage outside the baseplate to a varying degree, with 11% saying they were ‘not at all’ worried about it (Figure 1A). Those who worried about leakage to a ‘very high’ degree on average experienced 2.7 (per 2 weeks) and 10.3 (per 3 months) leakage incidents. The lower the worry about leakage, the fewer such incidents experienced by respondents. Those who reported they were ‘not at all’ worried about leakage on average experienced 0.2 (per 2 weeks) and 0.3 (per 3 months) leakage incidents outside the baseplate.
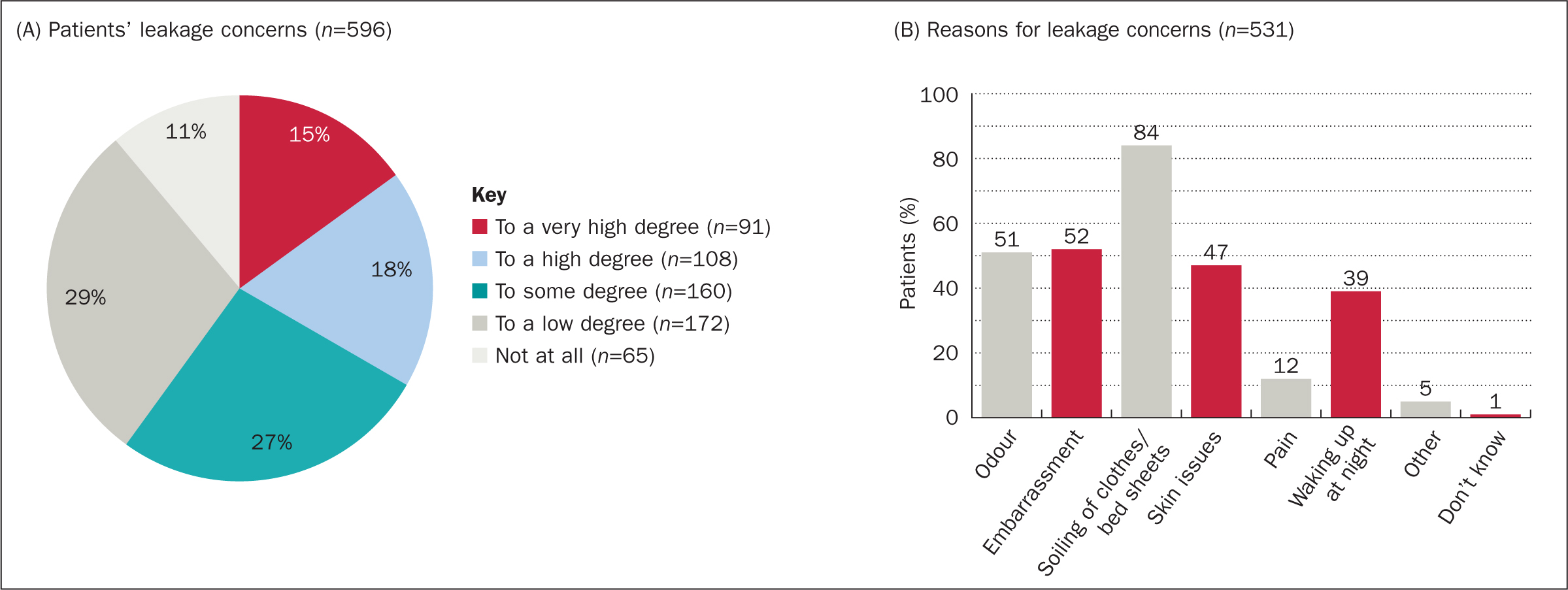
Most respondents (84%) who worried about leakage outside the baseplate reported that this was due to the risk of soiling clothes or bedsheets; respondents also reported concerns about odour (51%), embarrassment (52%), skin issues (47%) and waking up at night (39%). Only a few (12%) people worried about leakage due to pain (Figure 1B).
Interactions with health professionals following leakage issues
Respondents who had experienced leakage outside the baseplate at least once in the preceding 3 months were asked about their interactions with health professionals following such incidents (n=384). Most (78.6%, n=302) had not been in contact with a health professional, with the remainder 21.4% (n=82) reporting contact with one or more health professionals following such incidents. Of the respondents (n=384) who reported leakage outside baseplate at least once during past 3 months, 9.9% had had physical contact with a stoma nurse, 2.9% had had physical contact with a home care nurse, and 1.8% with a GP. Furthermore, 15.4% of the 384 respondents had had remote consultations with a stoma care nurse via the telephone or online (Table 3).
Table 3. Consultations with health professionals following incidents of leakage outside the baseplate (n=384)
| Type of consultation | % | |
|---|---|---|
| Physical visit with a stoma care nurse (in the hospital, practice, or your home) | 38 | 9.9 |
| Telephone or online consultation with a stoma care nurse | 59 | 15.4 |
| Physical visit from a home care nurse | 11 | 2.9 |
| A face-to-face visit with a general practitioner (GP) | 7 | 1.8 |
| Don't know | 4 | 1.0 |
NB Respondents could choose more than one type of consultation if they had been in contact with multiple health professionals within the past 3 months. Percentages are the proportion of all respondents (n=384) experiencing leakage outside the baseplate at least once over the 3 months
Usage of pouching systems following incidents of leakage outside the baseplate
Participants were asked about how their pattern for using pouching systems had changed, the duration of this change, and the average increase of changes of pouching systems per week in periods when they experienced issues related to leakage outside the baseplate.
More than half of respondents (54.4%) had not changed their usage pattern when experiencing issues with leakage outside the baseplate, while 45.6% reported making changes to their usage pattern by increasing the number of pouching systems and/or changing the type of pouching system (Table 4). Four out of 10 (39.6%) increased their number of pouching system changes and few respondents changed their type of pouching system (6.3%) (Table 4).
Table 4. Change in respondents' usage pattern for pouching systems (n=384)
| ‘During periods with issues of leakage outside the baseplate have you changed the usage pattern of your pouching system (stoma bag/baseplate)?’ | n | % |
|---|---|---|
| I increase the number of pouching system changes for a period | 152 | 39.6 |
| I change the pouching system type (flat/convex/concave) | 24 | 6.3 |
| I do not change my pouching system usage pattern | 209 | 54.4 |
| Don't know | 0 | 0.0 |
Respondents could choose more than one applicable option
NB Responses from patients who experienced leakage outside the baseplate at least once in the preceding 3 months (n=384)
Of the 152 users who increased the number of pouching system changes, 146 quantified the increase to 6.4 changes per week on average (median 7 changes per week, interquartile range 3.5–7 changes per week) (Table 5). The 130 users who quantified a temporary increase had done so for an average of 4.2 days (median 3.5 days, interquartile range 1.5–5.5 days), whereas 15 users among the 152 (9.9%) reported a permanent increase; 7 responded ‘don't know’ (Table 5).
Table 5. Respondents who increased use of pouching system (n=152)
| ‘On average, when increasing the number of pouching system changes for a period due to leakage, how many extra changes does that constitute?’ | n | % |
|---|---|---|
| Two additional changes per day | 27 | 17.8 |
| One additional change per day | 53 | 34.9 |
| One additional change every second day | 38 | 25.0 |
| One additional change every third day | 15 | 9.9 |
| One additional change per week | 11 | 7.2 |
| Less than one additional change per week | 2 | 1.3 |
| Don't know | 6 | 3.9 |
| ‘When increasing the number of changes of pouching systems due to leakage, how long is this period?’ | n | % |
| 1–2 days | 61 | 40.1 |
| 3–4 days | 36 | 23.7 |
| 5–6 days | 13 | 8.6 |
| 7–8 days | 7 | 4.6 |
| 9–10 days | 5 | 3.3 |
| More than 10 days* | 8 | 5.3 |
| Permanently | 15 | 9.9 |
| Don't know | 7 | 4.6 |
NB Responses from patients who experienced leakage outside the baseplate at least once in the preceding 3 months and who reported increasing the number of pouching system changes (n=152)
Use of supporting products following leakage outside the baseplate
Participants were asked about the use of supporting stoma products in periods when they had issues with leakage outside the baseplate. Six out of 10 (58.9%) respondents who had experienced leakage in the preceding 3 months did not change their usage pattern of supporting stoma care products (Table 6).
Table 6. Changes in pattern of usage of supporting products/accessories (n=384)
| ‘During periods with issues of leakage outside the baseplate have you changed your usage of supporting stoma products/accessories? | n | % |
|---|---|---|
| I increase the existing usage of my supporting products/accessories | 96 | 25.0 |
| I add additional products to my change routine | 81 | 21.1 |
| I do not change my routine of supporting stoma care products/accessories | 226 | 58.9 |
| Don't know | 5 | 1.3 |
Respondents could choose more than one applicable option
NB Responses from patients who experienced leakage outside the baseplate at least once in the preceding 3 months (n=384)
One-quarter of respondents increased their use of existing supporting products (Table 6), of whom 73 users who reported a temporary increase in usage said that on average they had continued to do so for 5.0 days (median 3.5 days, interquartile range 1.5–5.5 days).
Finally, 21.1% of respondents added supporting products to their change routine following leakage issues (Table 6), such as skin protection (51.9%), tape (48.1%) or rings/seals (44.4%); many had also added paste (34.6%), powder (25.9%) or adhesive remover (24.7%) to their changing routines (Table 7).
Table 7. Use of additional supporting products during a change in routine following leakage issues (n=81)
| ‘When adding products to your change routine due to leakage, which supporting products do you add?’ | n | % |
|---|---|---|
| Rings/seals | 36 | 44.4 |
| Paste | 28 | 34.6 |
| Tape | 39 | 48.1 |
| Adhesive remover | 20 | 24.7 |
| Skin cleanser | 18 | 22.2 |
| Skin protection | 42 | 51.9 |
| Belt | 17 | 21.0 |
| Powder | 21 | 25.9 |
| Deodorant | 8 | 9.9 |
Respondents could choose more than one applicable option
NB Responses from patients who experienced leakage outside the baseplate at least once in the preceding 3 months and who reported adding additional supporting products to their change routine (n=81)
Cost of leakage outside baseplate
When applying unit costs relevant to the UK healthcare sector (Table 8) to the reported increase in healthcare resource utilisation (nurse and GP consultations, pouching systems, and supporting products), the cost of a single leakage event was estimated to be £32.47 in the first 3 weeks following a leakage incident (Table 9). The primary cost contributors were nurse and GP consultations (62%), with pouching systems accounting for 29% and supporting products for 9% of the cost (Table 9).
Table 8. Summary of cost input: pouching systems, supporting products, nurse consultations, and GP consultations.
| Input | Unit cost | Source | |
|---|---|---|---|
| Pouching systems | One-piece product, flat baseplate | £3.36 | Weighted average of 5 most prescribed pouching systems, Prescription Cost Analysis (PCA), February 2021 (NHS Business Services Authority, 2021) |
| One-piece product, convex baseplate | £4.77 | ||
| Supporting products | Ring/washer | £2.08 | Weighted average of most prescribed supporting products by manufacturer Coloplast. If single-use product was available (eg wipe) this was preferred, PCA, February 2021 (NHS Business Services Authority, 2021) |
| Paste strip | £0.84 | ||
| Tape | £0.69 | ||
| Adhesive remover wipe | £0.52 | ||
| Skin cleanser wipe | £0.36 | ||
| Skin protection wipe | £0.78 | ||
| Belt | £7.20 | ||
| Deodorant sachet | £0.24 | ||
| Ostomy powder | £2.53 | ||
| Nurse consultations | Visits to a stoma care nurse | £119.05 | One hour of patient contact with band 6 nurse, Personal Social Services Research Unit costs of health and social care 2019 (Curtis et al, 2019) |
| Online/telephone consultations | £19.04 | NHS reference costs 2019/20 (NHS England, 2021) | |
| Home care nurse visits | £71.44 | ||
| GP consultations | Physical visit with a GP | £184.00 | One hour of patient contact excluding direct care staff cost and without qualification costs (unit costs of health and social care 2019) (Curtis et al, 2019) |
Table 9. Cost contribution of health professional consultations, pouching systems and supporting products
| No of patients | Base no of patients | Probability | No of services to be included | Cost (£) | Sum (£) | Percentage of total cost | |
|---|---|---|---|---|---|---|---|
| Consultations * | |||||||
| Physical visit with a stoma care nurse (in the hospital, practice, or your home) | 38 | 384 | 0.099 | 1 | 119.05 | 11.78 | |
| Telephone or online consultation with a stoma care nurse | 59 | 384 | 0.154 | 1 | 19.04 | 2.93 | |
| Physical visit from a home care nurse | 11 | 384 | 0.029 | 1 | 71.44 | 2.05 | |
| A face-to-face visit with a GP | 7 | 384 | 0.018 | 1 | 184.00 | 3.35 | |
| Subtotal | 20.11 | 62% | |||||
For the 152 individuals who reported an increase in pouching systems, the extra number of units used per leakage outside the baseplate event was calculated using their reported additional use of pouching systems and their reported duration of doing so. This was subsequently costed using unit costs from Table 8. Assumptions for the calculation included the exclusion of 2-piece ostomy systems and a 50/50 split of flat and convex products based on UK market trends (NHS Business Services Authority, 2021)
***For each type of supporting product, the extra number of units used per leakage outside the baseplate event was calculated using respondents' reported additional use of products and their reported duration of doing so. This was subsequently costed using unit costs from Table 8. Assumptions for the calculation included the use of two pieces of tape per change (included in cost), belt could be counted only once, ostomy powder was assumed to use 1/30 of a bottle per change
NB Responses among patients who experienced leakage outside the baseplate at least once in the preceding 3 months (n=384)
Discussion
Leakage of stomal effluent, especially incidents where faeces progressed outside the baseplate and onto clothes or bedsheets, has a high impact on people's health-related QoL (Jeppesen et al, 2022; Rolls et al, 2022). Utility decrements for women suffering from faecal incontinence have been reported in the range of 0.04-0.09 (measured using Health Utility Index Mark 3 (HUI3), EuroQol Five-Dimension (EQ-5D) and Short-Form Six-Dimension (SF-6D) questionnaires) (Harvie et al, 2011), which are close in value to the range reported for experiencing leakage onto clothes for people living with a stoma (0.02-0.11, estimated using time trade-off) (Rolls et al, 2022). Despite the two studies by Harvie et al and Rolls et al using different methodologies to estimate the related utilities, this could indicate that leakage onto clothes carries a significant impact on health-related QoL similar to that of faecal incontinence. The health-related QoL impact of chronic conditions is highly complex due to the variable frequency and type of complications. Additional research is required to create greater transparency when comparing chronic disease areas.
Despite many attempts, innovations in stoma care have not yet properly solved the issue of mitigating the risk of leakage progressing outside the baseplate, and about 90% of respondents in the present study worried about leakage. On average, they experienced 1.1 incidents of leakage outside the baseplate within 2 weeks, with only about one-third (35%) not experiencing such incidents in the past 3 months. These data support the findings of previous studies on the prevalence of stomal leakage (Porrett et al, 2011; Claessens et al, 2015; Hedegaard et al, 2020; Martins et al, 2022), highlighting that leakage of stomal effluent continues to be an issue for many people living with a stoma, even for experienced users who have had a stoma for more than 10 years.
Following incidents of leakage outside the baseplate, 40% of respondents increased their use of pouching systems, 25% increased use of existing supporting products and 21% added supporting products to their change routine. The increased use of stoma care products (both pouching systems and supporting products) on average lasted 4-5 days following an incident of leakage. This study, therefore, highlights that experiencing leakage progressing outside the baseplate promotes behavioural changes to mitigate the risk of future leakage incidents and to cope with the associated worry. The cause of respondents' increasing use of pouching systems and supporting products following leakage incidents was not investigated in the study. The increase could be related to many factors, such as the respondent trying to self-manage, or recommendations from health professionals, product manufacturers or peer support. Further investigation is needed to better understand patient behaviour in stoma care.
A multinational survey (Jeppesen et al, 2022) found that worrying about leakage caused many people (about half the respondents) with a stoma to increase their change frequency of pouching systems and to use additional supporting products, whereas few sought advice from peers and product manufacturers on the topic. People worrying most about leakage more often used supporting products, such as rings/seals, paste, belts and tape, to mitigate the risk of future incidents (Jeppesen et al, 2022). Inappropriate use of stoma care products is a concern for healthcare authorities, and there are prescription guidelines in the UK to prevent this (PrescQipp, 2015). Together, the data presented here and previously (Jeppesen et al, 2022) suggest that reducing people's worry about leakage and the number of incidents of leakage outside the baseplate may potentially reduce the overuse of pouching systems and supporting products.
In this study, more than two-thirds (68%) of participants had had their stoma for more than 10 years. Despite this, most still experienced problems with leakage outside the baseplate and the majority (79%) of those who had experienced such incidents in the past 3 months had not been in contact with a health professional. These numbers are comparable with the proportion of people seeking advice from stoma care nurses due to worry about leakage (Jeppesen et al, 2022), suggesting that even experienced users could benefit from easier access to assessments of stoma-related complications. As an example, the UK patient pathway for stoma care provides the most support within the first year of stoma formation with recommendations for a subsequent annual review concerning stoma management and product use (Davenport, 2014). Davenport's (2014) study also found that the implementation of annual reviews with a stoma care nurse led to reductions in the use of supporting products and therefore brought sizeable cost savings.
A consensus study was recently published between Colostomy UK, Ileostomy and Internal Pouch Association UK, Urostomy Association UK and Coloplast Ltd, highlighting the need for lifelong support from stoma care nurses to reduce leakage issues and that access to such support should be consistent across the country (Aibibula et al, 2022). From this consensus research, it is clear that the delivery of individualised and holistic care is considered crucial to people living with a stoma.
The level of care needed by patients varies throughout the patient journey. Many need more support at the beginning of their journey following stoma surgery, when they need practical and emotional support, while others need greater support later, eg during significant life events. Stoma care nurses try to empower patients to be able to self-manage their stoma care, and patients may feel that they should be able to manage without contacting health professionals, which may account for the relatively low numbers seeking help. Another reason may be restricted access to stoma care nurse specialists, as there is a shortage of nurses or at least a shortage of nursing time. There is a wish from people living with a stoma for longer home-care visits to address specific care needs and the option to request access to stoma care nurses as needed (Bowles et al, 2022). Providing easier access to stoma care nurse specialists, for example, via increased use of remote consultations (Augestad et al, 2020; Oliquiano et al, 2021; Brewer et al, 2022), could potentially be a solution for struggling users to have more frequent interactions to help solve issues with leakage. Implementation of more remote consultations could lessen the number of home-based care visits needed and lessen the burden of travel to better prioritise the time of stoma care nurses.
This study adds to existing research by quantifying the impact of leakage events outside the baseplate in terms of cost. It suggests that such leakages incidents are associated with a substantial increase in the consumption of healthcare resources, both additional stoma care products and interactions with health professionals. The cost of a single leakage event was estimated to be £32.47 based on unit costs derived from the healthcare system in the UK. The cost is an attempt to map the impact of faecal leakage events on the UK healthcare system; supplementary studies around this subject should be conducted to further illuminate and understand the cost impact of leakage-related complications, for example, how leakage outside the baseplate can affect an individual's ability to work.
Implementation of stoma care innovations that can reduce the number of leakage incidents outside the baseplate and related concerns may potentially limit the overuse of other stoma care products people use to mitigate the risk of leakage. Digital health solutions, ie wearable devices and connected healthcare solutions, are increasingly being adopted in healthcare systems across many areas of patient care (Awad et al, 2021), however, implementation of digital health solutions remains limited in stoma care.
Limitations
The results presented in this study should be interpreted in the context of the following limitations. The respondents were recruited only from the CORE survey panel across five countries (UK, USA, France, Germany and Denmark), the majority of whom used a Coloplast product. Hence, the study results may not necessarily represent the global stoma population. Future studies including more countries and a wider stoma population could outline global trends and enable analyses of country-specific differences. The bias towards elderly and experienced users in this study warrants further analysis of how younger and/or newly operated users respond to incidents of leakage outside the baseplate.
The survey was developed to quantify the impact of leakage outside the baseplate in terms of healthcare resource utilisation, which has not previously been undertaken. However, as this research is solely based on user-reported recall data this could bias the results, especially because respondents were asked to recall as far back as 3 months for some questions. Leakage and the worry of leakage have also been shown to impact the individual in terms of overall mental wellbeing and ability to work (Jeppesen et al, 2022), and it could be hypothesised that the total cost impact of leakage was not investigated in this survey, potentially underestimating costs. Additional research should be conducted to measure real-life increases in healthcare resource utilisation following leakage incidents outside the baseplate, to increase the validity of the findings of this study.
Some assumptions were made in pricing the increases in healthcare resource utilisation relating to leakages outside the baseplate, which would have impacted the estimate to some degree. It was assumed that all the baseplates used were evenly distributed between flat or convex products, and that none of the respondents used concave products. For supporting products, Coloplast was used as the only manufacturer, mainly due to the large number of manufacturers and the variation in products in the market.
In the UK and most other countries, the coding system for tracking stoma-related complications is either not optimal or non-existent, meaning that the cost of stoma-related complications and associated costs are an ongoing area of research. Despite the limitations of this study, in the view of the authors it provides a relevant contribution to the research field of stoma care in trying to understand the cost impacts of stoma-related complications.
Conclusion
This study highlights that many people living with a stoma struggle with incidents of leakage progressing outside the baseplate, even though they have had their stoma for several years, and that most respondents worry about leakage. Experiencing episodes of leakage outside the baseplate promoted behavioural changes for about half the respondents, leading to increased use of stoma care products, both pouching systems and supporting products.
New stoma care products or solutions are warranted that can reduce the number of incidents of leakage progressing outside the baseplate to reduce people's worry about leakage. Such solutions could potentially reduce the usage of stoma care products that many people use to mitigate the risk of future incidents of leakage outside the baseplate.
KEY POINTS
- Leakage outside the baseplate is prevalent (1.1 episodes of leakage in the 2 weeks preceding the survey), even in a population of experienced people living with a stoma
- Following an incident of leakage outside the baseplate, many people increased their use of pouching systems and supporting products
- The increased use of pouching systems on average lasted 4.2 days following an incident of leakage outside the baseplate
- About 1 in 5 (21.4%) respondents had been in contact with a health professional following leakage issues, so many people experiencing leakage outside the baseplate suffer in silence
- A single incident of leakage outside the baseplate is estimated to cost the healthcare system £32.47, based on the increased use of stoma care products and health professional interactions 3 weeks after an incident
CPD reflective questions
- Leakage incidents outside the baseplate result in increased use of stoma care products and more health professional interactions. Consider the value for both patients and the healthcare system of reducing such incidents
- Reflect on initiatives that can ensure the proper use of stoma care products to alleviate concerns about leakage
- Reflect on initiatives that may ease access to health professionals for users struggling with leakage incidents outside the baseplate


