The incidence of stoma complications is difficult to determine, especially in Italy, where care provided varies between counties and is not homogeneous (Denti et al, 2020).
Despite the introduction of new surgical techniques and increasingly specific guidelines, many international studies have reported incidence rates for stomal, peristomal and skin complications of between 3% and 82% (Cottam et al, 2007; Kwiatt and Kawata, 2013; Salvadalena, 2013; Ambe et al, 2018; Malik et al, 2018).
Patient-related and surgery-related factors contribute to the risk of stomal complications (Hendren et al, 2015). The main risk factors associated with stomal, peristomal and skin complications include issues with the type and the position of the stoma, emergency surgery and comorbidities, such as heart disease (Chaudhary et al, 2015; Andersen et al, 2018; Denti et al, 2020).
Complications may cause negative outcomes, which contribute to a worsening quality of life (Person et al, 2012). These are divided into early and late complications. Early complications are those that commonly occur within 30 days of surgery and most frequently include peristomal separation, stomal necrosis, stomal retraction, skin complications, haemorrhage and abscess (Pine and Stevenson, 2014; Carmel et al, 2016). Late complications are those that usually occur at least 30 days after surgery and often include stomal stenosis, prolapse and hernia (Shabbir and Britton, 2010).
There are several types of complication:
- Peristomal separation is the detachment of stomal tissue from the skin surrounding the stoma from the mucocutaneous junction and may be a result of poor healing tension or infection (Colwell and Beitz, 2007)
- Stomal necrosis is the death of stomal tissue resulting from impaired blood flow (Colwell and Beitz, 2007; Shabbir and Britton, 2010)
- Stomal retraction arises when the stoma is flush with the abdomen or retracted into it, so the spout does not protrude above skin level (O’Flynn, 2018)
- There is no standard definition of skin complications in the literature and no standard way of categorising their severity. Different classifications of skin problem have been suggested eg contact dermatitis, mechanical or chemical injuries, and fungal or bacterial infection (Nybaek, 2009)
- Haemorrhage as a stoma complication can result from inadequate haemostasis during stoma construction, portal hypertension, trauma, underlying disease and because of some medications, such as prolonged use of analgesic anti-inflammatory drugs (Barr, 2004). Stomal haemorrhage should be categorised as either minor or major. Minor stomal haemorrhage is limited to the external mucosal surface of the stoma or the surrounding peristomal skin, which may bleed easily on touch and present with superficial abrasions. Major stomal haemorrhage is characterised by spontaneous and vigorous bleeding, often with blood visibly dripping down the abdomen. Heavy bleeding may indicate a damaged blood vessel (Coleman, 2020)
- An abscess is a collection of purulent material beneath the skin (Carmel et al, 2016)
- Stomal stenosis is the narrowing or contracting of the stomal tissue at the skin or fascial level, impairing effluent drainage (Colwell and Beitz, 2007)
- A prolapsed stoma is one that, essentially, telescopes out through itself, causing abnormal lengthening (O’Flynn, 2018)
- Parastomal hernia is a type of incisional hernia occurring in abdominal integuments near a stoma. Here, abdominal contents, typically the bowel or greater omentum, protrude through the abdominal integuments around the hernia sac at the location of the stoma (Styliński et al, 2018).
Aim
The aim of this study was to analyse the onset of stomal, peristomal and skin complications one month (30 days) after ostomy creation (early complications).
The complications of interest included stomal complications (retraction, oedema, haemorrhage, necrosis, prolapse, hernia, abscess and stenosis), peristomal separation and skin complications.
Method
A retrospective model was used for this study. This review analysed ETN (enteral stomal therapy nurse) reports of patients who had an ostomy created at the emergency surgery unit of the San Raffaele Hospital in Milan, Italy, between January 2016 and December 2020.
The ETN is a nurse who specialises in the management of patients with urinary and faecal diversions, draining wounds and fistulas, and faecal and urinary incontinence (Doughty, 1992). The ETN has a fundamental role in ostomates’ rehabilitation, which may be affected by the development of ostomy complications (De Paula, 1996; Carmel et al 2016; Ambe et al, 2018).
Exclusion criteria were: patient age <18 years, pre-existing skin pathologies, suprapubic catheter, fistula and percutaneous endoscopic gastrostomy (PEG) and nephrostomy.
Observations were made over the first 30 days after surgery and involved both elective and emergency operations, which included colostomies, ileostomies and urostomies. Demographic variables included age, sex and ostomy type. The following variables were studied: skin lesions, stomal complications and peristomal complications.
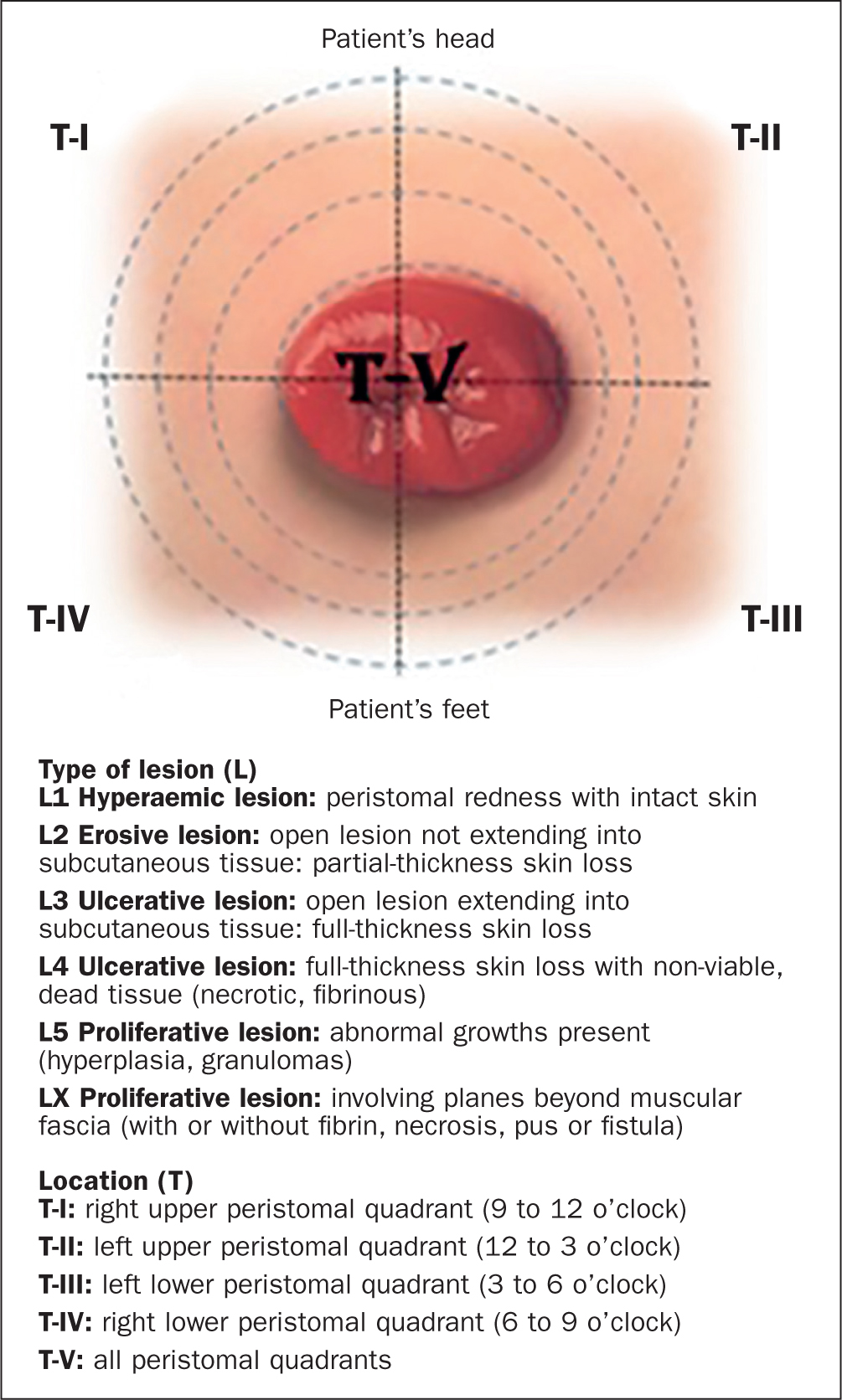
Data were collected then compared using statistical software Peristomal skin lesions were evaluated using the Study of Peristomal Skin Lesions 2.0 (SPSL) scale (SACS—studio sulle alterazioni cutanee peristomali 2.0 in Italian). This is a validated Italian tool, based on evidence and developed out of a clinical need, which provides standardised definitions of stomal skin lesions (Bosio et al, 2006).
This scale allows practitioners to assess and classify lesions according to six categories (L1-LX), identify lesion location on quadrants around the stoma (TI–TV) and document it (Figure 1).
Results
From January 2016 to December 2020, 1347 observations were carried out. Of these, 84 were excluded and the sample was consequently of 1263 reports. Seven of these involved patients with two types of stoma created simultaneously.
The sample’s characteristics are shown in Table 1. Of the sample, 61% were male and 39% were female. Colostomy was the most common stoma type (70%), while urostomy was the least common (4%).
Table 1. Sample characteristics (n=1263)
| n | % | |
|---|---|---|
| Sex | ||
| Male | 772 | 61 |
| Female | 491 | 39 |
| Stoma type | ||
| Colostomy | 889 | 70 |
| Ileostomy | 324 | 26 |
| Urostomy | 57 | 4 |
Age: average: 65.7 years; range: 18–94 years
The incidence of stomal and peristomal skin complications one month after ostomy creation was 1292. There were no complications in 37% of observations, while 63% of patients developed one or more complications. Skin complications were the most common (330) and abscess was the least common, with no cases recorded.
Complication types are shown in Table 2. The most detected stoma complication was oedema (293), while abscess was the least common stoma complication, not occurring at all. Of the cases of oedema, 207 were related to colostomy, 80 to ileostomy and six to urostomy. Patients with urostomies had no complications of haemorrhage, prolapse and hernia. There were 330 skin complications and 99 cases of peristomal separation. Skin complications were the most common complications in all stoma types.
Table 2. Total complications (n=1292)
| Complication | Retraction | Oedema | Haemorrhage | Necrosis | Prolapse | Hernia | Abscess | Stenosis | Peristomal separation | Skin complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Total n (%) | 288 (22%) | 293 (23%) | 23 (2%) | 107 (8%) | 28 (2%) | 27 (2%) | 0 (0%) | 97 (7%) | 99 (8%) | 330 (26%) |
| Colostomy | 220 (76%) | 207 (71%) | 17 (74%) | 69 (64%) | 21 (75%) | 17 (63%) | 0 (0%) | 68 (70%) | 71 (72%) | 252 (76%) |
| Ileostomy | 56 (20%) | 80 (27%) | 6 (26%) | 37 (35%) | 7 (25%) | 10 (37%) | 0 (0%) | 24 (25%) | 26 (26%) | 61 (19%) |
| Urostomy | 12 (4%) | 6 (2%) | 0 (0%) | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 5 (5%) | 2 (2%) | 17 (5%) |
Discussion
Data analysis showed 1292 complications: 863 (66%) stomal complications; 99 (8%) peristomal separation; and 330 (26%) skin complications.
Stoma complications were divided by type of stoma (Table 3). Oedema was the most detected stoma complication (34%), while abscess was not reported.
Table 3. Stoma complications (n=863)
| Complications | Colostomy n (%) | Ileostomy n (%) | Urostomy n (%) |
|---|---|---|---|
| Retraction (33%) | 220 (36%) | 56 (25%) | 12 (50%) |
| Oedema (34%) | 207 (33%) | 80 (36%) | 6 (25%) |
| Haemorrhage (3%) | 17 (3%) | 6 (3%) | 0 (0%) |
| Necrosis (13%) | 69 (11%) | 37 (17%) | 1 (4%) |
| Prolapse (3%) | 21 (3%) | 7 (3%) | 0 (0%) |
| Hernia (3%) | 17 (3%) | 10 (5%) | 0 (0%) |
| Abscess (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Stenosis (11%) | 68 (11%) | 24 (11%) | 5 (21%) |
The incidence of oedema in literature has been reported at about 25% (Denti et al, 2020). Among colostomies, 619 stoma complications were found, with retraction (36%) the most common. In ileostomy, 220 stoma complications were observed, with oedema (36%) being the most common. There were 24 stoma complications found with urostomy and retraction (50%) was the most common. No haemorrhage, prolapse, hernia or abscess were found in urostomy.
One of the most common stoma complications was retraction (33%). A systematic review has found this complication to occur in 1%–11% of all stomas (Szymanski et al, 2010).
All stoma type had a significant frequency of retractions: 36% in colostomy, 25% in ileostomy and 50% in urostomy. Retraction was classified as a complication because stomas are easier to manage when the spout projects at an appropriate level above the skin. It can result from multiple factors such as a short mesentery, obesity, a thickened abdominal wall, excessive scar or adhesion formation, and inadequate stomal length (Butler, 2009). The rate of retractions was significant, and these could have led to further complication.
The least common stoma complication was abscess: in the early postoperative period, parastomal abscesses are relatively uncommon, with a reported incidence of 2–14.8% (Kann, 2008).
Necrosis accounted for 8% of stomal complications. Their incidence has been reported to be about 13% (Krishnamurty et al, 2017).
In the sample, haemorrhage was 2%; no data were found in the literature on the incidence of stoma haemorrhage (Coleman, 2020).
All these complications were common in the first 30 days for several reasons, such as proximity to surgery, predisposing factors, and changes in the conformity of the abdomen and ostomy in the first postoperative days (Carmel et al, 2016).
In addition, patients initially lacked knowledge in how to manage their ostomy and carry out correct ostomy care (Porrett and McGrath, 2006). An appropriate collection system is one of the most important factors contributing to patient wellbeing (Black, 2000).
While the data analysed concerned ETN reports made within 30 days of surgery, 152 (17%) late stomal complications were detected, of which 97 (7%) were stenosis. Of these, 70% were related to colostomy, 25% to ileostomy and 5% to urostomy. The incidence of stomal stenosis has been reported as being between 2% and 23% (Carmel et al, 2016). Stenosis may be attributable to surgical construction techniques, excessive scar formation, irradiation of the bowel segment, peristomal sepsis or trauma owing to an ill-fitting pouching system (Barr, 2004).
Prolapse accounted for 2% of stomal complications. Its incidence has been reported as 7%–26% (Murken and Bleier, 2019).
Parastomal hernia is a relatively common complication among stoma patients, with an incidences of between 2% and 56% (Jones et al, 2018). Hernia accounted for 2% of stomal complications, and 63% of hernias occurred in colostomies.
There were 323 peristomal and skin complications in colostomy, 87 in ileostomy and 19 in urostomy (Table 4). Skin complications were the most common complications in all stoma types (78% in colostomy, 70% in ileostomy and 89% in urostomy). Studies have reported a prevalence of peristomal skin complications of between 29% and 63% depending on the type of ostomy and skin complication (Arumugam et al, 2003; Persson et al, 2010; Lindholm et al, 2013; Salvadalena, 2013).
Table 4. Peristomal and skin complications (n=429)
| Complications | Colostomy n (%) | Ileostomy n (%) | Urostomy n (%) |
|---|---|---|---|
| Peristomal separation (23%) | 71 (22%) | 26 (30%) | 2 (11%) |
| Skin complications (77%) | 252 (78%) | 61 (70%) | 17 (89%) |
Limitations
Limitations of this study include that pre-existing pathologies and differences in surgical technique were not considered.
In addition, because the study is retrospective in nature, the data may have inherent flaws unknown to researchers. The formation of stomas by different surgeons and with different surgical techniques may have affected the rates of complications (Koc et al, 2017).
Finally, the types of skin complication were not recorded.
Conclusion
In a study of 1263 reports, 63% of patients were found to develop one or more complications during the period examined, which is in line with other studies. The most frequent stomal complication was oedema (23%), whereas the most frequent complication in general was that affecting the skin (26%).
In colostomy, the most frequent complication was retraction (36%), in ileostomy, oedema (36%) and, in urostomy, retraction (50%). Haemorrhage was reported as a complication in 2% of cases; the authors did not find figures on its incidence in the literature. Late complications were detected (11%) as well as early ones.
Risk factors were not identified in this study. However, in the literature, a high body mass index, diabetes, having the surgery as an emergency and a short spout height have been indicated as possible risk factors for complications after stoma creation (Carmel et al, 2016).
In this study, a high number of retractions (22%) was found in all ostomy types, and could be a factor that led to further complications.
Complication rates were high, in line with data in the literature, and many factors could influence their onset.
Finally, given the ETN role is fundamental to preventing complications, additional exploratory or randomised controlled trials are needed to identify the optimal nursing strategies and follow-up, performed by the ETN, to prevent complications.
KEY POINTS
- The incidence of early complications is difficult to determine, especially in Italy, where the care provided to stoma patients varies
- Complications are common within a month of stoma formation, with around two-thirds of patients developing one or more complication
- Retraction may lead to other types of complication
- Skin problems are the most common problem
- Complications that normally occur a month or longer after surgery can also develop at an early stage
CPD reflective questions
- How would you recognise early stomal, peristomal and skin complications?
- Why do complications depend on ostomy type?
- The data in this study is compared with that in the literature. How do these figures compare with the incidence rates of complications in your place of work?


