Manual infection surveillance is a labour-intensive process that can involve the infection prevention and control (IPC) team accessing multiple data sources and copying and pasting data into spreadsheets, attracting the risk of error. Automated infection detection using algorithms within the electronic medical record or via specialised add-on data-mining software has been shown to improve the quality of data and the use of staff resources (National Information Board and Department of Health, 2014; Barnes, 2017). Hospitals that adopt this technology are more likely to implement best practices to prevent healthcare-associated infections (Association for Professionals in Infection Control, 2010). The emergence of COVID-19 in early 2020 highlighted the need for efficient digital solutions in health care to support infection control.
Even before COVID-19, Public Health England (PHE) (now the UK Health Security Agency (UKHSA)) recommended the exploitation of technological change in its infectious disease strategy, stating as one of its top priorities:
‘Ongoing opportunities to harness and embed new technologies, to link and integrate our data, and improve our surveillance.’
PHE, 2019: 3
The strategy also highlights that:
‘Infectious disease surveillance generates information that shapes public health decisions, determines appropriate actions, and informs how we commission research. This includes passive surveillance to monitor for changes in the epidemiology of infectious diseases, and active surveillance to collect in-depth information to assess new and emerging problems, including through syndromic surveillance.’
PHE, 2019: 10
Digital health technologies have been actively promoted as key to the effective implementation of containment and mitigation strategies (Whitelaw et al, 2020; National Audit Office, 2020; Maguire et al, 2021).
In 2013, Dorset County Hospital NHS Foundation Trust (DCHFT) implemented use of the ICNET clinical surveillance system (CSS) (Baxter Healthcare). The IPC team asked the Trust board to support the CSS and the board recognised that the benefits would outweigh the costs. This CSS draws patient data from various electronic sources to provide meaningful information to IPC staff and alert them to critical infection risks among hospital inpatients. During the pandemic, the IPC team, which consisted of three nurses, used the CSS to optimise the identification of patients infected or potentially infected with COVID-19. This enabled quick isolation of such patients, reducing the likelihood of hospital-acquired COVID-19 for others. Access to the CSS via tablet computers enabled mobile access to the required data at the point of care during ward rounds. Ward rounds are part of normal service provision, and this practice was in place before and during the pandemic. If the IPC team were required to work remotely, they were able to refer to the CSS and contact colleagues onsite directly to provide support. Despite the intense focus on COVID-19 surveillance and reporting, the automated nature of the CSS ensured that the team did not lose focus on other priority pathogens.
Reporting capabilities in the CSS allowed timely analysis of data, ensuring the hospital had accurate, up-to-date information to make informed decisions quickly. Senior leaders were able to provide the public with clear and accurate reports on the status of COVID-19. This reinforced hospital board support for the continued use of the CSS.
Benefits of the clinical surveillance system
DCHFT provides a full range of district general hospital services, including an emergency department and links with satellite renal-care units across the county for dialysis care. It is the main provider of acute hospital services to a population of over a quarter of a million people in the western part of Dorset.
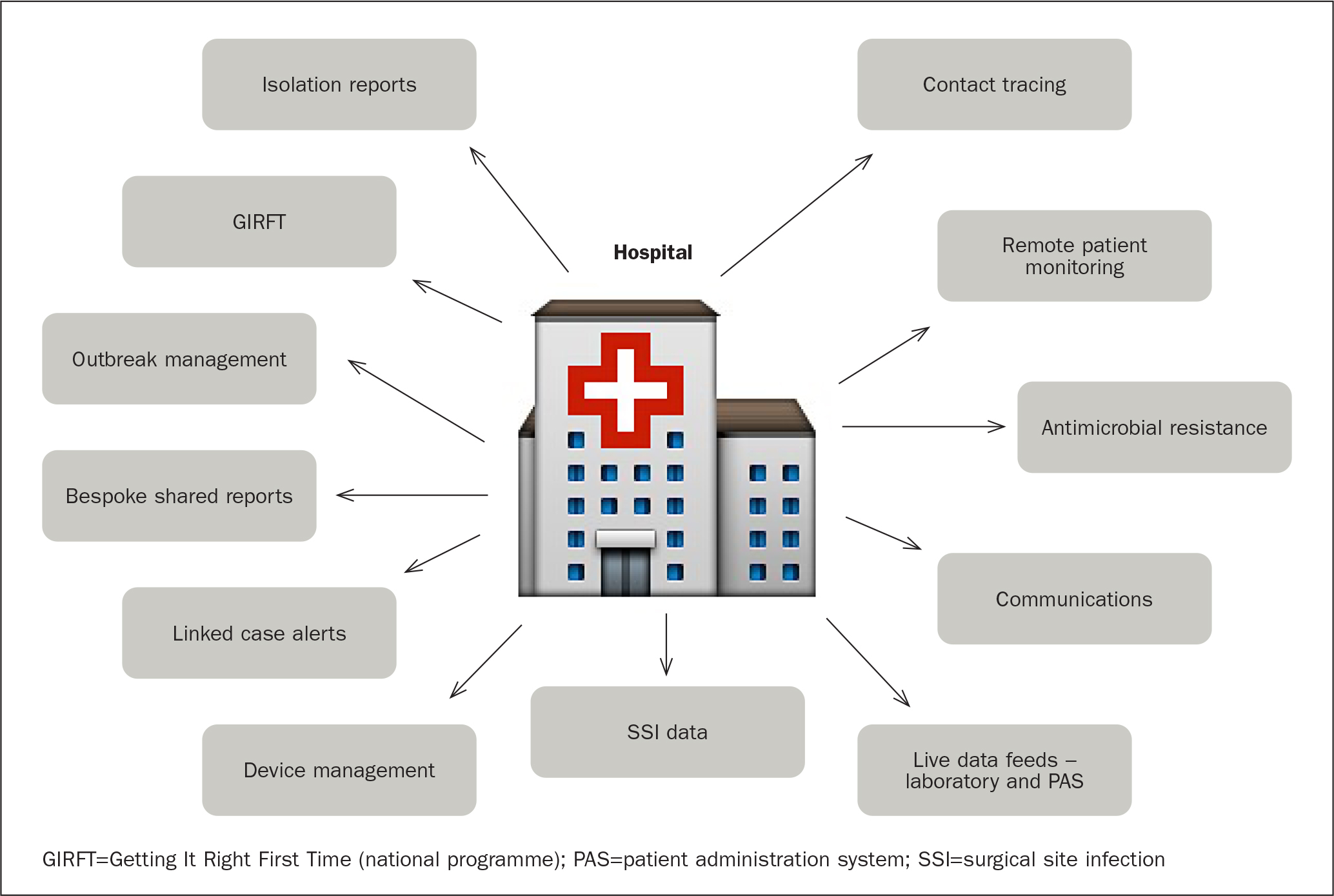
The CSS uses real-time data from various clinical information systems across a facility, such as patient administration systems (PAS) and laboratory information management systems (LIMS) and applies advanced analytics to provide meaningful information to the users for clinical decision-making. The algorithms also look for event clusters to track sources of infection. User-defined alerts bring immediate attention to lab results, patient exposures and infection clusters, allowing for early intervention to prevent outbreaks. A function within the CSS enables swift data collection to collate reports relating to specific organisms, antimicrobials and locations, which enables immediate trend analysis and subsequent action (Figure 1).
The CSS is web-based and of particular importance for DCHFT has been its ability to provide up-to-the-minute data and alerts via mobile devices. This frees the IPC team to visit wards and clinical departments regularly with immediate access to required data and to work remotely when team members’ physical presence was not possible. This close working relationship with the clinical teams enabled a positive relationship with the IPC team and the team were seen as supportive to ensure safe patient care.
The ‘alert’ functionality highlights any patient previously identified with an infection for the IPC team to monitor from admission. In addition, as soon as an infection is identified in the microbiology laboratory, the IPC team is alerted via the CSS, ensuring that they can review the affected patients immediately, so they are placed in an environment suitable for their needs and one that avoids an unnecessary cross-infection risk. Up-to-the-minute data enables maintenance of an isolation list within the CSS so the clinical site team can manage patient flow safely and effectively throughout the hospital.
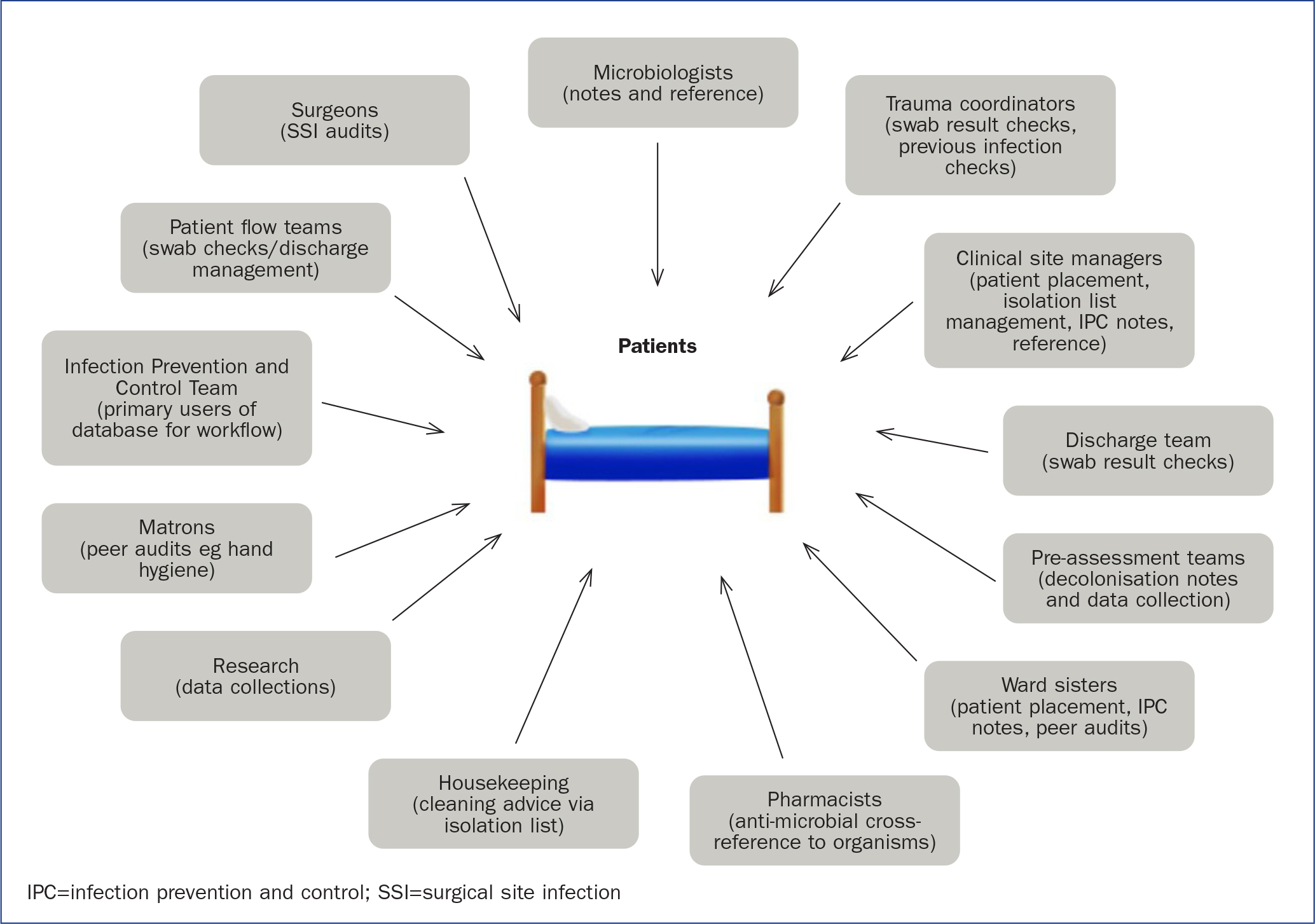
The CSS also includes multidisciplinary notes for each patient, so clinical staff such as microbiologists, the antimicrobial pharmacist, the pre-assessment team, and the IPC team can keep up to date with the CSS's chronological narrative format and access data even outside of normal working hours. Other healthcare staff can also use the CSS to support their patients and it provides a central area for all digital information relating to infection control (Figure 2). The CSS is particularly effective for reporting; users can easily generate isolation lists, contact tracing lists and reports on organism data and antibiotic resistance patterns, among others.
The CSS device module provides a link with digital feeds from other systems monitoring indwelling devices such as urinary catheters and peripheral and central venous catheters. This information enables device documentation to be accessed and audited.
Shaping clinical surveillance software development
DCHFT has worked with ICNET to help shape the functionality of the CSS to meet its needs and test new functionalities that are now part of the platform used by other hospitals in the UK and elsewhere. This is a key element of the best practice effectiveness standards defined by the National Institute for Health and Care Excellence (2019) for tier 1 digital health technologies, as it highlights both ‘credibility with UK health professionals’ and ‘acceptability with users’.
In particular, the IPC team worked with ICNET to develop and use a surgical site surveillance tool within the CSS. Surgical site infections (SSIs) have been targeted as an area in which reporting of data and trend analysis can have a significant impact on reducing adverse events. The adoption of the SSI module enabled the IPC team to collaborate closely with the surgeons to manage the data produced. The data were readily available for analysis and subsequent actions were taken to reduce the risk of infection. Implementation of this module was linked to the SSI rates dropping by almost 62% over 2 years (DCHFT, 2018; 2020).
The surgical site infection surveillance tool pulls data from multiple IT platforms to create a log relating to each surgery. This is manually checked, and infection data are confirmed before it is sent from the CSS directly to the UKHSA Surveillance of Surgical Site Infection database, as part of a mandatory national audit. Without the facility of the CSS to assist with this process, the hospital would require additional staffjust to perform these audits. Before the implementation of the CSS function, the audit required at least 2 to 3 days a week of trained staff time and this is now reduced to a few hours within the audit period.
IPC team response to COVID-19
When the pandemic was declared in the UK, the NHS actioned its incident command mechanisms. Locally, at DCHFT, an incident management team of senior staff, including the IPC team, was created. The team met twice daily to review the status of patients, new treatment protocols, and critical supplies. Overnight data on the number and severity of cases were immediately available via the CSS, which meant the IPC team were always prepared for the important hospital-wide daily update meeting. The CSS played a vital role in the hospital's response to COVID-19. The tool includes exposure tracking, contact tracing and a cross-infection matrix.
DCHFT had its first confirmed COVID-19 case on 12 March 2020. By mid-April there were around 30 COVID-19 inpatients. One of the three IPC team members dealt with routine work, and the remaining team members focused their time on COVID-19. Being a smaller hospital, it was manageable but exhausting. By late summer and early autumn of 2020, the COVID-19 rate had settled to near zero, to the point where elective procedures could begin again. In November 2020, when there was a small national peak that so many UK hospitals confronted, it did not have a major impact at DCHFT as the systems were in place to support safe IPC.
In late December 2020 the second wave of COVID-19 was experienced at DCHFT, with a dramatic increase in cases. The critical care unit and surge capacity were tested to the limit and additional critical care beds were designated and staffed. In comparison with April 2020, when there was a single COVID-19 ward, five wards were assigned and fully used as COVID-19 areas.
Having these peaks and troughs in cases enabled the IPC team time to adjust the processes in place to support patients and staff. There was understandable anxiety about cross-infection risk among staff, particularly in the first wave, so having the IPC team present and able to support and advise was beneficial in the second wave, and helped to reduce this anxiety.
The hospital did not experience any issues with the supply of personal protective equipment (PPE). It had procured surgical-grade masks early on in the pandemic and was able to work with providers to keep other supplies in stock. The IPC team conducted PPE audits while on the wards, ensuring staff were wearing the right equipment and donning and doffing it correctly. The team was especially vigilant about handwashing — providing continued auditing and staff support where required. These efforts resulted in minimal cases of staff infections during the first year of the pandemic. The CSS was adapted to enable digital audit surveillance for PPE as well as a hand-hygiene audit.
Another positive result of the COVID-19 response by the IPC team has been a broader range of leadership involvement in infection control. The Trust's board has supported ICNET since it voted to secure the technology. Board engagement has been consistent, reinforced by new member orientations and other presentations by the IPC team. Before the pandemic, the IPC team reported through the director for infection prevention and control. During the pandemic, the team had involvement with a wider range of senior managers, including the director of operations, the medical director and the chief executive officer, who chairs infection prevention group meetings as well as root cause analysis panels.
Over the course of the pandemic, data produced by the CSS was the subject of intense daily scrutiny. Having clear precise information was crucial to map the infection both in the healthcare setting and community. Having such up-to-date data and belief in the accuracy was appreciated by the leadership, who were able to make it the basis of information and data shared with the national databases and, subsequently, the media.
Consolidation and building on success
Following its introduction, the CSS further developed and enhanced the way the IPC team worked. Being fully mobile, it freed the team from their desks. Using tablet computers, the team can be present for ward rounds and clinical visits in any area of the hospital. Among the tasks for each round are:
- Ensuring patients are in the most appropriate location for IPC measures (isolation/cohort)
- Maintaining a live isolation list for the patient flow team
- Giving cleaning advice for all patient cubicles to housekeeping staff
- Reviewing any admissions who have a known infection risk
- Supporting staff and patients at the bedside.
Implementing digital ways of working has changed the clinical practice of the IPC team members at DCHFT. They have worked their way from being viewed as outside auditors to being accepted as team players within the clinical setting. Team members have maintained their clinical skills and demonstrated this in practice, providing direct care where and when required.
Through regular ward rounds, the IPC team can engage with clinical staff and are able to spot trends and act quickly to relocate patients to reduce potential exposure time while samples are being processed and critical cleaning is commenced.
The team uses the clinical notes section on the isolation report to provide an assessment of each patient's cross-contamination risk to others. This guides the decision on whether a patient can be transferred to a lower infection risk area if a more infectious case comes in with a higher chance of transmission.
The availability of the CSS to many teams enables the devolution of accountability. Clinical site teams are not reliant on being told about issues by the IPC team, and this promotes an approach in which good infection control is everyone's responsibility. For example, out of hours, the clinical site teams can refer to the CSS to gain information on a patient's current infection status and risk assessment.
All this work on the units, including screening for certain high-risk patient groups, decolonisation of high-risk patients prior to procedures, and close monitoring of indwelling devices, have coincided with gradual and steady reductions in healthcare-associated infections (HCAIs) at DCHFT. Despite use of a more expansive definition of healthcare-associated Clostridium difficile infections by UKHSA (NHS Improvement, 2018), there were just six reportable cases detected within 48 hours after admission at DCHFT from April 2019 to March 2020, continuing a significant downward trend (DCHFT, 2020). Bed closures due to gastroenteritis and other diarrhoea-related viruses have been significantly reduced. The last case of reportable meticillin-resistant Staphylococcus aureus (MRSA) bacteraemia was in 2013.
Automated syndromic surveillance allowed the Trust to keep its focus on these other bacteria and viruses, which continued to be present despite the reduction in elective procedures during the pandemic. HCAI rates have stayed low.
COVID-19 certainly tested the CSS, and its constant capabilities enabled the IPC team to maintain credibility in demonstrating quick and precise information to the Trust board.
The vision across Dorset is for ICNET to be accessible by all IPC teams as a shared system. A whole health economy approach is essential, especially as the integrated care system (ICS) develops and progresses. It was agreed by all the leads for IPC in Dorset that a combined CSS solution would be the way forward and all three NHS healthcare trusts (acute, community and mental health) are now ‘live’ with a single instance of the CSS.
Conclusion
DCHFT has had long-term success using a robust, specialised CSS tool. Having accurate, timely data instantly retrieved from all key sources and sent via task messages to mobile devices has made the IPC team far more productive and effective in identifying infectious diseases, isolating sources of infection, and auditing compliance with protocols. With several years’ experience, it was established practice for the IPC team, freed from manual data collection and reporting, to perform much of their work on the wards, teaching staff about infection control protocols and quickly identifying patients for isolation. This ability took on added significance because of COVID-19. Giving medical staff access to the CSS sped up the process of identifying patients with COVID-19 no matter when or where in the hospital they reported. Senior leaders gained a renewed awareness of the CSS as an essential tool as data were available instantly to facilitate decision-making, enabling timely communication with the media and public on the progress of the pandemic.
As we move ahead into a post-pandemic healthcare system it is evident that novel bacteria and viruses will emerge and having a robust CSS in place to support healthcare staff is crucial.
Key points
- This article explores how a clinical surveillance system supported a healthcare setting before the COVID-19 pandemic and how it was able to adjust to support clinical practice during the pandemic
- Digital solutions to support patient safety should be actively promoted and implemented
- Patient-centred care is an important feature of the design of any healthcare digital tool
- It is important to consider the wider integrated care system when developing digital solutions
CPD reflective questions
- Consider what digital solutions are in place in your clinical setting. How useful and effective are they?
- Reflect on the nurse's role in the provision of clinical care alongside digital technology
- Based on the model of a single instance digital tool, how could a similar model influence your practice?


