Digital health or e-health tools are becoming more common in healthcare generally and in the care of patients with inflammatory bowel disease (IBD) (Avery, 2020). Evidence for the potential positive impact from supported self-management using these tools emerged from a literature review carried out in preparation for a service improvement project (SIP) (Avery, 2019) as part of the work for the author's Master of Science in advanced clinical practice. It was concluded in this review that this integrated approach could provide an alternative management plan for patients who could be offered follow up and support remotely.
In 2015 a patient management system was implemented in the IBD department at the district general hospital (DGH) where the author practises. This particular e-health tool is linked with a national data-collection initiative called the IBD Registry (https://ibdregistry.org.uk/) and was implemented with a view to making data collection easier (Munro, 2014). At the DGH in question, the primary workload for collating information with this tool lies with nursing (medical colleagues citing time restrictions on the use of the patient management system in clinical practice).
A usual IBD consultation is predominantly clinician-led (IBD specialist nurse or consultant) following a medical model (Bickley and Szilagyi, 2013), with elements of motivational interviewing in order to assist agenda setting (Martins and McNeil, 2009; Mocciaro et al, 2014; Neighbour, 2015). The author's practice has mirrored this approach with added disease-specific clinician-completed measures of disease activity providing a clinically led review overall. Disease-specific measures of disease activity commonly include the Harvey Bradshaw Index (HBI) (Best, 2006; Vermeire et al, 2010) in Crohn's disease and the IBD Registry dataset favours the Simple Clinical Colitis Activity Index (SCCAI) in ulcerative colitis (Munro, 2014), whereas the DGH uses a modified Mayo Clinic Score for ulcerative colitis activity. Also recorded are results of faecal calprotectin testing, which is a chemical measure of inflammation used in the management of patients with IBD (Dhaliwal et al, 2015; Parr et al, 2016; Asser et al, 2017). All of these approaches are well-established and used in IBD care internationally. Standard care in the Trust where the project took place includes the use of telephone clinics and advice lines as well as face-to-face care.
A further outcome of the review (Avery, 2019) was evidence that a PROM with validation across IBD sub-types was already available for use: the IBD-Control questionnaire. This internationally recognised tool has potential for use with existing or new e-health systems that also have quality of life (QoL) measures incorporated (Bodger et al, 2014; Gledhill et al, 2014; Bojic et al, 2017; International Consortium for Health Outcomes Measurement, 2018; Kim et al, 2018). In conjunction with existing faecal testing at home using the IBDoc (Bühlmann Laboratories) calprotectin home testing kit, this could function as a remote disease-management strategy (Parr et al, 2016; Avery and Wilson, 2018; Avery et al, 2020a) The PROM, which had been designed with patients and incorporates QoL impacts as well as disease activity (Bodger et al, 2014), was tested by Gledhill et al (2014) and was found to add value to the consultation process and be well-tolerated by patients. Patients recommended that the PROM should be made available a digital platform, and Bojic et al (2017) also recommended its integration in e-health systems. Using the IBD-Control questionnaire for this pilot study was a prudent choice as it has been integrated into the data set for the IBD Registry (Bodger et al, 2014; Gledhill et al, 2014; Avery et al, 2017; Bojic et al, 2017). The IBD Registry is another key driver for clinical engagement because of the benefits it brings in terms of understanding care for people with IBD and the improvements that have been seen since its inception (Bodger, 2019; Shawihdi et al, 2019). Seeking to understand what is important to patients is key to implementing successful change—PROMs begin to do this on an individual level and when used correctly can help to enhance the consultation process (Avery et al, 2020b). With this in mind the author took steps to assess the acceptance of using PROMs via e-health in the DGH where they worked.
Aims
In order to test the concept of using PROMs to support practice and follow up a small-scale service improvement pilot project was designed. The aim of the study was to understand whether empowering patients to undertake supported self-management could in turn lead to improved flow through outpatient services.
The objective of this service improvement was to answer the following questions:
- Do patients feel this is a positive suggestion—are they accepting of self-management using e-health tools at home with support from clinicians remotely?
- Is there acceptability of the concept of using PROMs together with disease assessment and conventional tools (calprotectin, blood tests and clinician's assessment of disease activity) to prescribe care to patients at home, reducing the number of visits needed to outpatients?
Reducing the number of visits to outpatients would in turn have potential to improve the flow through outpatient services.
Methods
The above aims were to be achieved by evaluating an audit of PROMs looking at QoL as well as disease activity, completed using an electronic platform in real time at the point of patient contact. The disease activity indices used were the HBI and the modified Mayo Score, due to the author's familiarity with interpreting these tools as well as the validity and acceptability already shown (Best, 2006; Bennebroek Evertsz' et al, 2013).
An iPad was used to facilitate the collection of PROMs and a patient opinion questionnaire (Box 1), which was added for an additional layer of information to understand the level of acceptance of remote and supported self-management for patients. All patients were shown how to complete the tools before commencement and their understanding was checked. The score for the PROM was then combined with the usual consultation process and the IBD nurses carried out the usual care as documented above.
Box 1.Patient opinion questionnairePatient reported outcome measures (PROM) and self-management with remote monitoring to replace outpatient appointment
- What is your first reaction to the idea of supported self-management with remote monitoring? ☐ Very positive ☐ Somewhat positive ☐ Neutral ☐ Somewhat negative ☐ Very negative Coded for analysis 1–5
- How easy was the patient-reported outcome measure to complete? ☐ Extremely easy ☐ Very easy ☐ Somewhat easy ☐ Not so easy ☐ Not at all easy Coded for analysis 1–5
- Thinking about supported self-management with remote monitoring, is it something you feel you need or don't need? ☐ Yes ☐ No Coded for analysis 1–2 If no please explain why you feel you do not need it
- If supported self-management with remote monitoring were available today, how likely would you be to use supported self-management with remote monitoring? ☐ Extremely likely ☐ Very likely ☐ Somewhat likely ☐ Not so likely ☐ Not at all likely Coded for analysis 1–5
- If you could fill in the PROM and check your general health with blood tests and faecal calprotectin with access to advice either by email or phone would you be happy to not attend outpatients for this routine appointment next year ☐ Yes ☐ No Coded for analysis 1–2
- What is your gender? ☐ Female ☐ Male ☐ Transgender ☐ Prefer not to say
- What is your age? ☐ 18 to 24 ☐ 25 to 34 ☐ 35 to 44 ☐ 45 to 54 ☐ 55 to 64 ☐ 65 to 74
Ethical considerations
A discussion with the DGH audit department and research team concluded that the nature of the project meant local research ethical approval was not required in this case. Although service improvement is not research it should still meet the expectations of ethical principles of care (Beauchamp and Childress, 2013), to this end patient consent was sought verbally before beginning the PROM and discussed at the beginning of the electronic questionnaire. The patients were given the opportunity to complete the PROM in a private clinic room and this was filled in electronically by the patients themselves. As this formed part of work for an MSc the university ethics committee was also asked to consider the project, and gave clearance that there was no need for a full ethics application.
Sample
All patients that attended one of the IBD clinics over 2 consecutive weeks in November 2018 were selected, giving a total convenience sample of 20 participants.
Analysis
The data analysis was conducted using descriptive analysis and three-stage approach was used, as discussed by Whittaker (2012). The data analysis was conducted twice due to two separate questions being asked in the PROM and the opinion questionnaire. The questionnaire was coded using a simple numerical approach (see Box 1) then the questionnaire results were imported into an Excel spreadsheet and descriptive statistical analysis was used. The questionnaire produced nominal and ordinal data that is well suited to simple analysis, according to Whittaker (2012).
Results
Of the potential sample of 20 patients, 3 were excluded as they did not have a histological diagnosis of IBD, leaving 17 potential patients. Two patients declined to take part for reasons relating to IT literacy leaving a final study population of 15 (ulcerative colitis n=11, Crohn's disease n=4). Although this is a small sample it was deemed suitable for this preliminary study.
Results from the collection of the PROM are split into three categories:
- Well patient (W)—in remission,
- Well with questions (WWQ)—remission, but needs advice
- Needs continual review (NCR)—active disease requiring face-to-face revie.w
This was decided by comparing the scores from the PROM with the patient's usual disease measures—HBI for Crohn's disease and a modified Mayo Score for ulcerative colitis. Using this simple analysis 6 patients' combined scores led to a description of being ‘well’. These patients could all be offered review remotely using the proposed developed supported self-management approach.
When looking more closely at the individual responses the ‘well with questions’ patients reported active symptoms or had questions that would require management. These patients had issues relating to QoL or adjunctive medical issues such as fatigue, anxiety or depression and irritable bowel syndrome (IBS).
Figure 1 and Figure 2 show the proportions of patients who were assigned into the three categories.
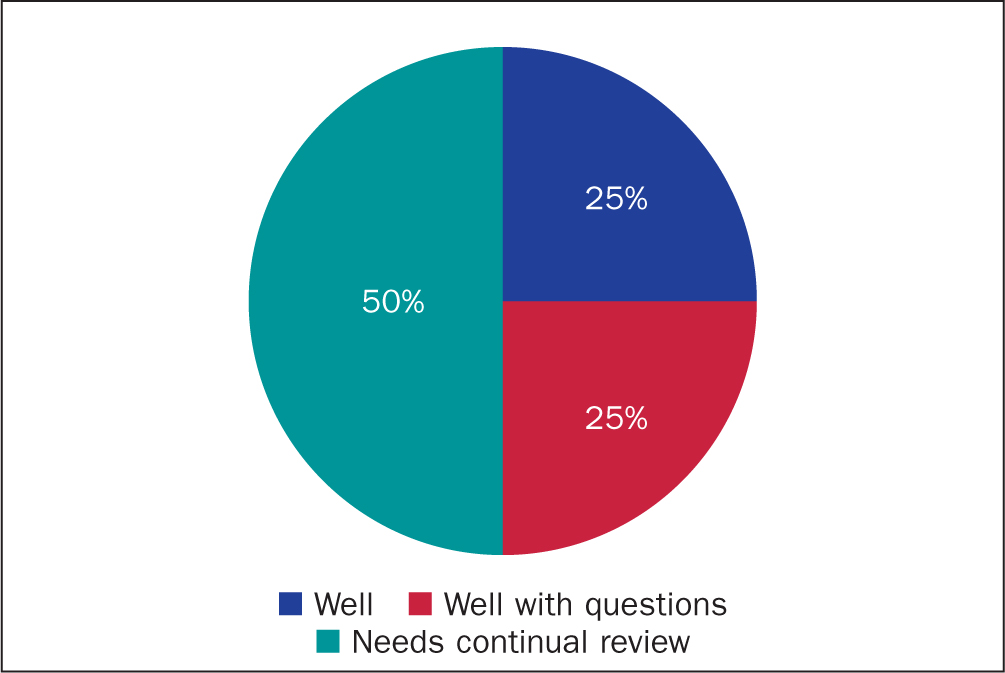 Figure 1. Findings for patients with Crohn's disease (n=4)
Figure 1. Findings for patients with Crohn's disease (n=4) 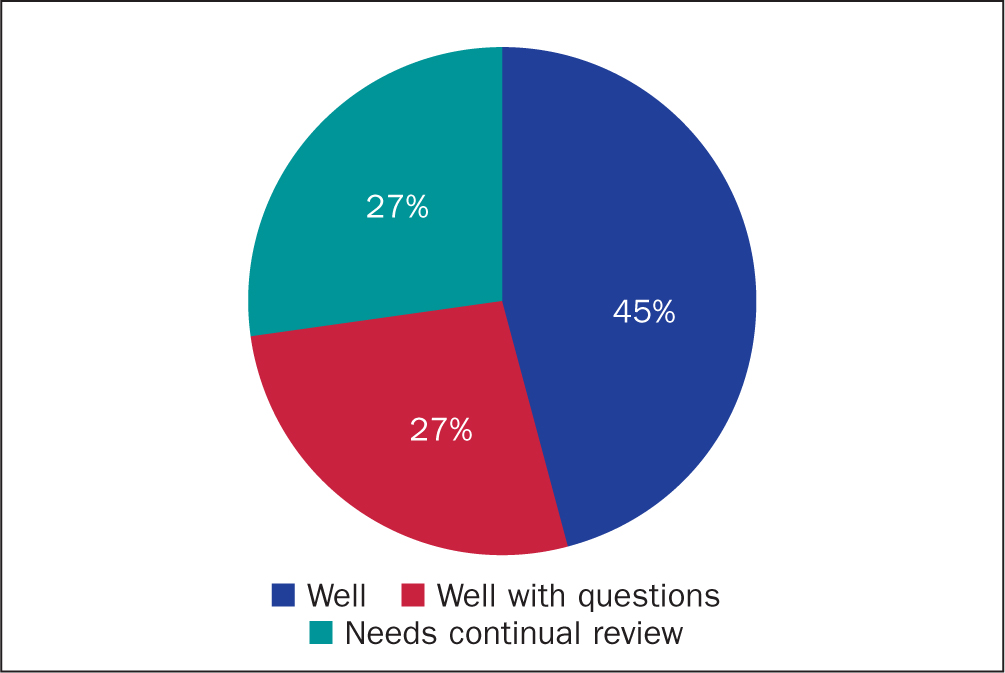 Figure 2. Findings for patients with ulcerative colitis (n=11)
Figure 2. Findings for patients with ulcerative colitis (n=11)
The disease activity measures and PROMs appeared to be in line to the same extent in both the patients with Crohn's disease and those with ulcerative colitis (Table 1), which suggests that this project could be equitable for all patients at the DGH with IBD.
Table 1. PROMs and disease activity
| Diagnosis | PROM score* | General wellbeing | HBI score† | Calprotectin level | Outcome of consultation | Status§ | |
|---|---|---|---|---|---|---|---|
| P1 | CD | 6 | 85 | 1 | 113 | perianal disease, on biologics | NCR |
| P2 | CD | 0 | 60 | 4 | 1000 | recent surgery on perianal disease | NCR |
| P3 | CD | 0 | 50 | 2 | 20 | constipation | WWQ |
| P4 | CD | 12 | 100 | 0 | 45 | well | W |
| Diagnosis | PROM score* | General wellbeing | Mayo Score† | Calprotectin level | Outcome of consultation | Status§ | |
| P5 | UC | 8 | 60 | 0 | 20 | some fatigue but fairly well | WWQ |
| P6 | UC | 4 | 80 | 0 | 400 | having a colonoscopy | NCR |
| P7 | UC | 6 | 70 | 4 | 360 | questions about medication some disease activity | NCR |
| P8 | UC | 12 | 100 | 0 | 20 | well | W |
| P9 | UC | 12 | 90 | 0 | 24 | well | W |
| P10 | UC | 12 | 95 | 0 | 20 | well but constipated | WWQ |
| P11 | UC | 12 | 95 | 0 | 20 | some activity few weeks earlier but all settled | WWQ |
| P12 | UC | 2 | 50 | 5 | 426 | flaring, needs to change treatment | NCR |
| P13 | UC | 10 | 95 | 0 | 28 | well | W |
| P14 | UC | 12 | 80 | 0 | 32 | well | W |
| P15 | UC | 12 | 100 | 0 | 20 | well | W |
CD=Crohn's disease; HBI=Harvey Bradshaw Index, UC=ulcerative colitis
* Patient-reported outcome measure (IBD-Control questionnaire) scored 0–16, the higher the score, the better the patient feels †Patient disease activity scores (HBI or modified Mayo Score): the higher the score, the less well the patient is
§Well (W), well with questions (WWQ) or needs continual review (NCR)
There was a 100% response to the patient opinion questionnaire (Table 2). The results show a positive response regarding the acceptability of supported self-management and the use of PROMS.
Table 2. Responses to the patient opinion questionnaire
| Q1 | Q2 | Q3 | Comments | Q4 | Comments | Q5 | Q6 | |
|---|---|---|---|---|---|---|---|---|
| P1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| P2 | 2 | 2 | 1 | 2 | 1 | 2 | ||
| P3 | 1 | 1 | 1 | 1 | 1 | 2 | ||
| P4 | 2 | 2 | 1 | 2 | 1 | 1 | ||
| P5 | 2 | 1 | 1 | 1 | 1 | 1 | ||
| P6 | 1 | 1 | 1 | 1 | 1 | 2 | ||
| P7 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| P8 | 2 | 1 | 1 | 2 | 1 | 1 | ||
| P9 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| P10 | 2 | 1 | 1 | 1 | 1 | 2 | ||
| P11 | 2 | 2 | 1 | 1 | 2 | 1 | ||
| P12 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| P13 | 2 | 2 | 2 | Not IT minded | 5 | Prefers face to face | 2 | 1 |
| P14 | 2 | 2 | 1 | 1 | 1 | 2 | ||
| P15 | 1 | 1 | 1 | 1 | 1 | 2 |
Note: Q7 is excluded from the table as there was no difference seen in range of responses in any one age range
In all, 13 patients responded ‘yes’ on being asked whether, if they could fill in the PROM and check general health with blood tests and faecal calprotectin with access to advice either by email or phone, they would be happy to not attend an outpatient clinic for this routine appointment next year.
Acceptability was consistent across age ranges (from 18 to 75+), all could see the benefit of the idea of supported self-management (Figure 3) and all the respondents found the PROM ‘easy’ or ‘very’ easy to fill in (Figure 4).
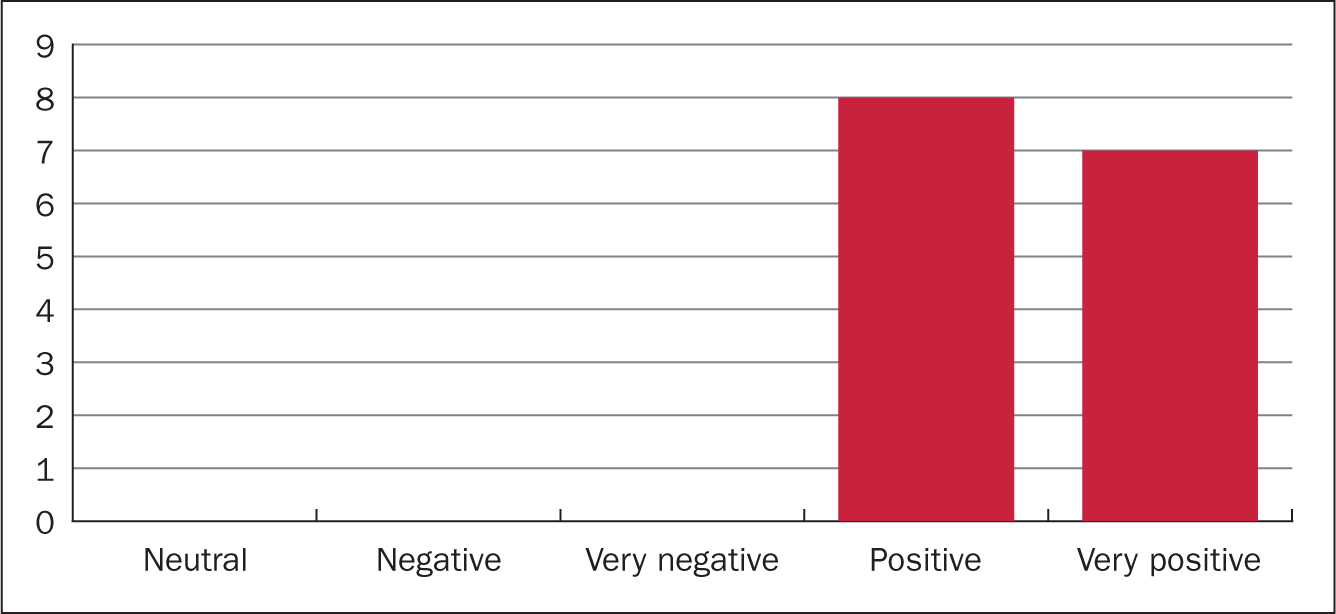 Figure 3. Q1: What is your first reaction to supported self management?
Figure 3. Q1: What is your first reaction to supported self management? 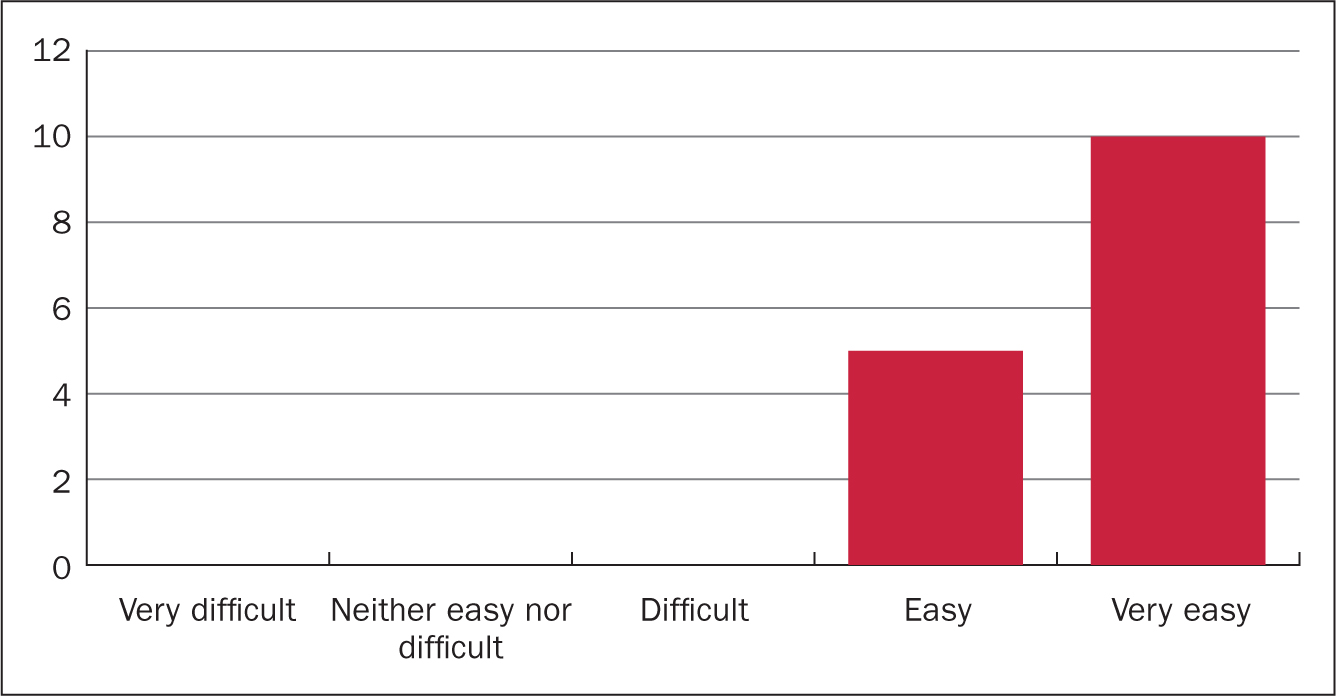 Figure 4. Q2: How easy was the PROM to fill in?
Figure 4. Q2: How easy was the PROM to fill in?
Discussion
In this service improvement project participants were invited to complete a digital questionnaire in addition to the PROM using their own personal smartphone, or an iPad provided. Inviting participants to complete the questionnaire during the clinic visit aimed to avoid failure to complete—which can lead to a phenomenon of failure bias in questionnaires (Whittaker, 2012)—and resulted in 100* return rate. To avoid coercion all patients were given the option to decline participation and withdraw consent at a later date as per general data protection regulations (Crowhurst et al, 2019). All questionnaire responses were confidential, but results could be shown on an individual anonymised basis in order to look at trends in gender and age, which can be important when looking at service development design (Boaz, 2016).
The evaluation of this service improvement was considered for its reliability and validity with the author reflecting on whether the measures would answer the question, Whittaker (2012) described this process as operationalisation and it helped to inform the decision to use a questionnaire as well as the PROM and the development of the questions. The author's aim was to use a range of questions looking for different responses, some closed questions and some using a scale; if the answers were negative on some questions a comment response was requested. The reasons for this were to offer patients the option to explain what barriers they had to acceptance of the idea of using e-health and remote management.
Although the author recognises that the individual skill of each patient with regard to digital skills was not assessed, the positive response to Q5 on the patient opinion questionnaire (Box 1) shows a willingness by people with IBD to take on remote monitoring. The data show a promising acceptance of e-health and remote management and the use of PROMs. The idea of supported self-management was generally accepted by all 15 of the participants and although the numbers here are small this positivity echoes that in previous work in this area (Calvert et al, 2013; Naghibi et al, 2014). PROMs report the patients' view of their wellbeing and disease state (Gledhill et al, 2014). In this study, six patients reported themselves as well and a further four had some issues to discuss but all those issues—fatigue, constipation and medication changes, even anxiety and depression—were amenable for remote management, including discussing either over the phone or via email if this was preferred by the patient. These issues are often managed remotely by phone in chronic disease management (Wicks et al, 2014; Chung and Basch, 2015; Squires et al, 2016; de Jong et al, 2017a). Tests can be requested and completed in primary care or delivered to the pathology specimen reception at the hospital; this is already done when patients are managed via the advice line in place at the DGH for patients with IBD. Ten patients from this study could have been managed remotely, suggesting that these face-to-face appointments could have been used by other patients. This could offer a freeing up of capacity in outpatients with a potential to improve patient flow through waiting lists and the outpatients service for IBD as a whole. The value of this in terms of QoL for the patients managed remotely would be less disruption to their daily lives, reducing unnecessary journeys and time off work to attend face-to-face appointments and the associated stress and anxiety that these things can bring to a patient with IBD (Kemp et al, 2012). Although this was not a cost-saving project, understanding the hard financial impact as well as QoL outcomes can be essential in building a business case for any service improvement project (Healthcare Quality Improvement Partnership, 2020).
This study did not assess the patients' individual capability, knowledge and skills regarding technology nor the patient cohort's access to digital tools at home. It is worth noting that the rapid switch to digital systems across the healthcare system in the context of the COVID-19 pandemic did not factor this in either, yet there have been reports of as high as 90* of all outpatient review or primary care appointments happening virtually (Kennedy et al, 2020; Lees et al, 2020; Smith et al, 2020; Maclean et al, 2020, Stokel-Walker, 2020). However, the ‘digital divide’ poses a potential risk to success. Devices and data use cost money and emerging from this switch to digital systems is another level of health inequality for those already affected by some of the worst health outcomes in the country, (Watts, 2020) and this all needs to be considered as e-health becomes normal practice.
Limitations
The sampling approach of including every patient attending clinic over 2 consecutive weeks was taken to try to bring variability into the sample even though it was small—this convenience sample avoided some selection bias due to the varied population in terms of age and gender of the IBD service at the DGH serving patients 16 and over. Personal investments in the project would provide extra bias if the sample was selected by the researcher (Robson and McCartan, 2015). Bias is always present in any study or project results due to the impact of self on the project (Kotter, 2012). Although a small sample it was deemed suitable for this preliminary study.
Other limitations of this evaluation are validity and reliability of the questionnaire design and the likelihood of the author's own bias in the questions, which are designed to be positive—this is a well-documented pitfall of questionnaires (Whittaker, 2012). The other aspect that could be considered missing is the view of an impartial clinician. However, the use of validated tools such as HBI and SSCAI could provide some comparative data helping with this clinical view. There is much documented in the literature about the need for self-management tools (Squires et al, 2016; Hughes et al, 2018) and the PROM already has validation and because of this evidence the clinician view is well reported, so this should not detract from any results of this evaluation. Any limitations in the study design relate to the purpose of the original project as a service improvement project rather than a research study.
Implications for practice
This response to this evaluation at a local level led to the PROMs being captured on an iPad in the outpatients setting. Allowing patients to use the PROM as a tool in the outpatient setting has led to longitudinal data being added to the patient management system for each individual. This has allowed for tracking of PROMs and disease scores alongside chemical and physical testing to build an individual picture of the QoL and physical impacts of IBD on that patient over time. Gledhill et al (2014) found that PROMs helped to enhance the patient conversation and this was also the author's experience in this limited setting. There is a growing body of literature showing that supported self-management can be a tool to help with sustainability as it can help to free up capacity in outpatients (Calvert et al, 2013; Gledhill et al, 2014; Naghibi et al, 2014; Wicks et al, 2014; de Jong et al, 2017b; Avery, 2019; Aziz et al, 2019). It is the author's opinion that this intervention and evaluation has added support for that growing body of evidence for PROMs and supported self-management using novel e-health tools, and that this must be integrated into clinical systems for maximum benefit. To this end, and on the author's recommendation, the DGH has allowed an upgrade to the existing IBD patient management system. Working with the software developer the author has piloted a dashboard style approach. The system now allows for the routine collection of patients' PROMs and disease activity scores using an iPad. Results from this early experience were presented at the European Crohn's & Colitis Congress in February 2020 (Avery et al, 2020b). Integration with existing structures of any e-health system is vital. It means that the data input from patients will be available to clinicians in real time, as in some proven applications (whch were also in the IDB context) (Calvert et al, 2013; Naghibi et al, 2014; Squires et al, 2016; Squires et al, 2017; Walsh et al, 2018).
COVID-19 update
Since the beginning of the COVID-19 pandemic the way outpatient care has been provided in the NHS has been changed rapidly and forever. Nearly all outpatient care ceased overnight (Willan et al, 2020) with much of the care provided virtually and with clinical commissioning groups leaving outpatient care, for many trusts remote and virtual e-health is here to stay (Davey, 2020). Patients with IBD experienced the same phenomenon (Kennedy et al, 2020) with face-to-face review cancelled for all but the most unwell patients. Some immediate evaluation of these changes in care management reveals that although acceptability is high, clinical teams worldwide would like to have a variety of options to support care for patients (Berg et al, 2020; Hernández Benabe and Langshaw, 2020; Lees et al, 2020; Verstraete et al, 2020). Patients using the services also report a high level of acceptability, but choice in what form of follow up they have is key, with 58* of people asked by the leading IBD patient organisation in the UK stating they would wish for a choice of face-to-face or virtual (Crohn's & Colitis UK, 2020).
Conclusion
This evaluation from a small sample of IBD patients shows that an intervention to provide an e-health application or internet link that could assist with remote management is something that patients can ‘buy into’—accept and engage with. Although the individual's capability and skill with digital tools at home was not assessed, patients did report that they found the concept of employing remote monitoring in place of outpatient appointments acceptable. This suggestion of acceptability could offer improvements in the patient flow in the IBD service. Although this is undoubtedly positive, it was a small study intended for service improvement and further research and evaluation of remote management of patients using e-health is needed. Since the COVID-19 pandemic healthcare systems have rushed forwards with the virtual and remote monitoring of patients in general. The caution expressed regarding changes to outpatient review that have occurred because of the pandemic confirm the need to better understand patient's perceptions and wishes and the impact the rapid alteration to outpatient care may have made to these perceptions and wishes.
KEY POINTS
- Integrated e-health tools can support clinical teams with real-time information
- This service improvement project collected data from a patient reported outcomes measure together with disease activity scores using a tablet in an outpatient setting
- The patients in this small study were positive about e-health and self management
- Since the COVID-19 pandemic healthcare system have rushed forwards with virtual and remote monitoring of patients in general, concerns and caution expressed regarding changes to outpatient review that have occurred because of the pandemic stress the need to better understand patient's perceptions and wishes
CPD reflective questions
- What changes have you seen in the e-health tools you have used to manage your patients during the pandemic and how has this impacted on care?
- How do you think patient-reported outcome measures can affect decision making in your specialism?
- On reflection, are there patients in your caseload who could be managed in a different way? Ask yourself how this might be facilitated in a way that supports patient safety.


