Urinary tract infections (UTIs) present a major burden for individuals with neurogenic lower urinary tract dysfunction (NLUTD), which is defined by abnormal or difficult function of the bladder and urethra in mature individuals (and/or prostate in men) with clinically diagnosed neurologic disorder (Dinh et al, 2019). To empty the bladder and avoid urological complications, intermittent catheterisation (IC) is used as the gold standard of care for voiding disorders in individuals with and without NLUTD (Kennelly et al, 2019). However, individuals who are dependent on IC also experience UTIs to a higher degree compared with the general population (Welk et al, 2022). NLUTD complexity typically makes these individuals more prone to infections and they also experience significantly longer hospital stays (Welk et al, 2022).
Different UTI risk factors in individuals using IC have previously been established. However, as catheter-associated UTIs can involve a broad range of symptoms and heterogeneity in the underlying disease, this makes the detection of UTIs challenging and underlines the increased risk of infection and potential failure of antibiotic treatment (Kennelly et al, 2019; Li, 2022).
UTIs can have a dramatic effect on quality of life (QoL) physically, mentally and socially, and the economic burden of UTI hospitalisation can impact society and healthcare systems globally (Hearn et al, 2018; Welk, 2020; Buchter et al, 2022). Therefore, addressing UTIs and QoL by involving patient perspectives in research is important in order to develop treatment and improve IC management in individuals depending on the procedure (Welk et al, 2022).
Given the lack of evidence using patient-reported data, the aim of this study was to investigate potential associations between UTI risk factors, such as IC technique, haematuria, perceived residual urine, recurrent UTIs, bowel issues and sex, in relation to patient-reported UTIs and QoL through self-reported data from individuals with and without NLUTD performing IC.
Methods
Study design and population
Data were obtained between March and April 2022 through an online survey distributed to a large voluntary IC user panel and through local country databases created by Coloplast. The respondents were individuals with lower urinary tract dysfunction (LUTD), both neurogenic and non-neurogenic, who were performing daily self-catheterisation using single-use IC devices of any brand. Respondents originated from 13 countries and were male and female adults aged at least 18 years. The online survey was conducted via Confirmit software and consisted of 60 questions in total: 30 questions on demographic factors, medical history, bladder emptying, and bowel issues; and 30 questions of the Qualiveen-30 questionnaire (Bonniaud et al, 2006), which is a validated instrument to assess health-related QoL. No personal data were obtained, thus, informed consent from the respondents was not needed.
Exposures: UTI risk factors
The investigated exposures defined as UTI risk factors in this study were included based on evidence from previous research (Kennelly et al, 2019) and an exploratory statistical approach further described below. UTI risk factors were defined as:
- Additional IC technique defined as applying additional strategies to assist bladder emptying when using IC (yes/no to: withdraw the catheter very slowly, withdraw the catheter in small steps, turn/rotate the catheter, change body position, put constant pressure on the stomach (abdominal pressure), tapping (small taps on the stomach), other)
- Apparent blood in the urine defined as haematuria (yes/no to: daily, weekly, monthly, less than monthly)
- Perceived residual urine left in the bladder after removing catheter (yes/no)
- Having recurrent UTIs, defined as a minimum of two UTIs during the past year requiring antibiotic treatment (Fisher et al, 2018) (yes/no)
- Having bowel issues (yes/no to: constipation, faecal incontinence, both constipation and faecal incontinence)
- Sex (female, male, other).
Other demographic factors and medical conditions included in the analyses were age (19-29 years, 30-39 years, 40-49 years, 50-59 years, 60-69 years, 70-79 years, 80+ years), country (Australia, Austria, Denmark, Finland, France, Germany, Italy, the Netherlands, Norway, Sweden, Switzerland, UK, USA), and having LUTD based on the cause of urinary issues (NLUTD due to spinal cord injury, multiple sclerosis, spina bifida, stroke, Parkinson's, diabetes, other neurogenic conditions; non-NLUTD due to unspecified prostate problems, bladder reconstruction, bladder cancer, unspecified post-surgery, other non-neurogenic conditions; other unspecified causes).
Outcomes: Patient-reported UTIs and QoL
The two main outcomes were defined as having any patient-reported UTIs requiring antibiotic treatment (yes/no to: antibiotics prescribed by doctors, antibiotics from own stock at home, other treatment), and QoL measured by the Qualiveen-30 questionnaire (Bonniaud et al, 2006) with questions scoring from 0 (no impact of urinary issues on health-related QoL) to 4 (high adverse impact of urinary issues on health-related QoL). Scoring was based on four domains (Bonniaud et al, 2008):
- Bothered by limitations defined as inconvenience (eg, time spent passing urine or thinking that the bladder problems complicate one's life; 9 items)
- Frequency of limitations defined as restrictions (eg going out without planning anything in advance or thinking one's life is regulated by bladder problems; 8 items)
- Fears (eg fearing smelling of urine or that one's bladder problems are worsening; 8 items)
- Feelings (eg feeling embarrassed or worried because of one's bladder problems; 5 items).
The overall QoL score was calculated from the mean score of the four domains ranging from 0 to 4 points, where scoring higher means that one's QoL is impacted to a higher degree and scoring lower on this scale shows less impact of urinary issues on QoL.
Statistical analysis
Descriptive analyses were used to describe the study population based on whether individuals had NLUTD or not, as it has previously been shown that individuals performing IC may differ in terms of UTI risk, depending on whether or not the cause of their LUTD is neurogenic (Welk et al, 2022).
To investigate the potential associations between UTI risk factors, patient-reported UTIs and QoL, two separate multivariate linear mixed models were used to estimate relative risk (RR) of UTIs and mean differences in QoL score, including 95% confidence intervals (95% CI). Using an exploratory approach, different effects and interactions were investigated, leading to two final models. The initial models included: haematuria, perceived residual urine, bowel issues, sex, country, additional IC technique, age, NLUTD/non-NLUTD, and recurrent UTIs (only included for the QoL outcome). Following model reduction, only significant (alpha=0.05) effects and covariates remained in the final models. The final model for UTI included haematuria, perceived residual urine, bowel issues, sex and country. The final model for QoL included haematuria, perceived residual urine, bowel issues, sex, country, additional IC technique, age and recurrent UTIs. Data were analysed using SAS Enterprise Guide v7.1 and a 5% significance level was applied in all statistical analyses.
Ethics statement
The project (Study Protocol No.: CPUSCC002) has received IRB D2-Exemption under 45 CFR § 46.104(d)(2) from the institutional review board WCG IRB. The participants all consented to receive survey questionnaires from Coloplast A/S, which conducted the survey, and to the use of data for analyses. The participants' data were treated with confidentiality in compliance with the EU General Data Protection Regulation, and the analyses were performed with aggregated anonymous data.
Results
In total, 3464 (6%) out of the 55 235 invited individuals performing IC responded to the survey with complete data (Figure 1). The majority were aged 50-79 years (53.2%) and had NLUTD (56.7%); the largest group was male (47.8%) (Table 1). Individuals resided in Denmark (19.2%), Italy (14.3%), Germany (13.1%), UK (12.6%), France (10.5%), USA (5.4%), Norway (5.3%), Sweden (4.6%), Australia (4.1%), The Netherlands (3.9%), Finland (3.8%), Switzerland (1.8%), and Austria (1.5%).
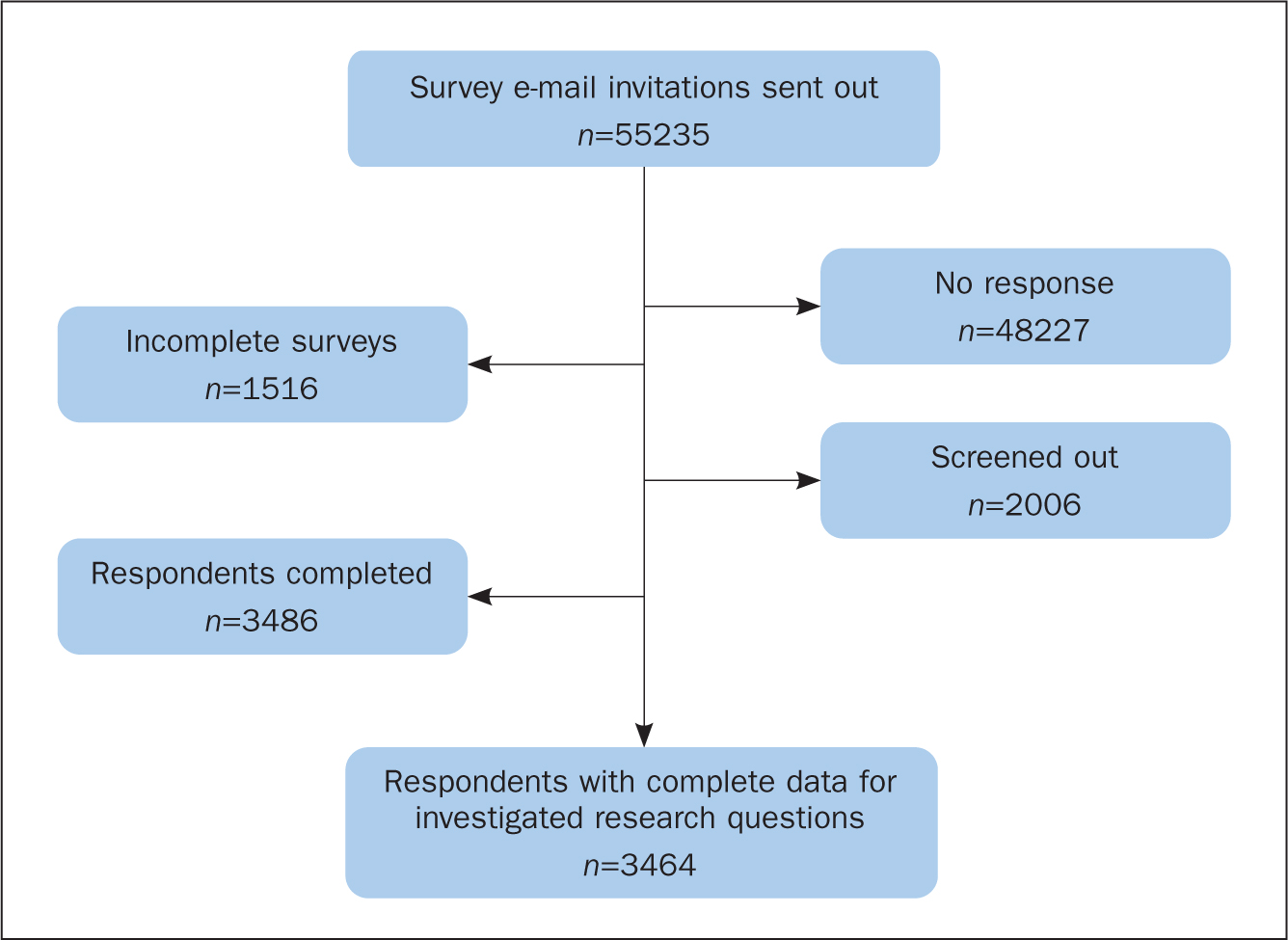
Table 1. Baseline characteristics for the study population divided into neurogenic and non-neurogenic lower urinary tract dysfunction cases (NLUTD/non-NLUTD), unspecified cases and the total population
| Characteristics | NLUTD cases n=1963 (56.7%) | Non-NLUTD cases, n=1063 (30.7%) | Unspecified cases, n=438 (12.6%) | Total population, n=3464 (100%) |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Age | ||||
| 18–29 years | 47 (2.4) | 3 (0.3) | 7 (1.6) | 57 (1.6) |
| 30–39 years | 147 (7.5) | 14 (1.3) | 19 (4.3) | 180 (5.2) |
| 40–49 years | 271 (13.8) | 25 (2.4) | 35 (8.0) | 331 (9.6) |
| 50–59 years | 387 (19.7) | 74 (7.0) | 66 (15.1) | 527 (15.2) |
| 60–69 years | 395 (20.1) | 207 (19.5) | 81 (18.5) | 683 (19.7) |
| 70–79 years | 202 (10.3) | 343 (32.3) | 89 (20.3) | 634 (18.3) |
| 80–89 years | 30 (1.5) | 122 (11.5) | 29 (6.6) | 181 (5.2) |
| 90+ years | 1 (0.1) | 8 (0.8) | 1 (0.2) | 10 (0.3) |
| Missing | 483 (24.6) | 267 (25.1) | 111 (25.3) | 861 (24.9) |
| Sex | ||||
| Female | 617 (31.4) | 199 (18.7) | 145 (33.1) | 961 (27.7) |
| Male | 874 (44.5) | 601 (56.5) | 181 (41.3) | 1656 (47.8) |
| Other | 471 (24.0) | 263 (24.7) | 111 (25.3) | 845 (24.4) |
| Missing | 1 (0.1) | 0 | 1 (0.2) | 2 (0.1) |
| Urinary issues* | ||||
| Retention | 1355 (39.1) | 919 (26.5) | 386 (11.1) | 2660 (76.8) |
| Incontinence | 1074 (31.0) | 218 (6.3) | 91 (2.6) | 1383 (39.9) |
| Missing | 48 (1.4) | 33 (1.0) | 11 (0.3) | 92 (2.7) |
| Bowel issues | ||||
| Fecal incontinence and/or constipation | 966 (49.2) | 120 (11.3) | 59 (13.5) | 1145 (33.1) |
| Number of UTIs within past year† | ||||
| 1 time | 271 (23.2) | 146 (25.5) | 49 (20.7) | 466 (23.6) |
| 2 times | 271 (23.2) | 136 (23.7) | 64 (27.0) | 471 (23.8) |
| 3 times | 209 (17.9) | 96 (16.8) | 33 (13.9) | 338 (17.1) |
| 4 times | 117 (10.0) | 50 (8.7) | 22 (9.3) | 189 (9.6) |
| 5 times | 72 (6.2) | 29 (5.1) | 18 (7.6) | 119 (6.0) |
| 6 times or more | 187 (16.0) | 101 (17.7) | 43 (18.1) | 331 (16.8) |
| Do not know | 39 (3.3) | 15 (2.6) | 8 (3.4) | 62 (3.1) |
| Total | 1166 (100) | 573 (100) | 237 (100) | 1976 (100) |
| Had minimum one UTI requiring treatment since start of IC | ||||
| Yes | 1744 (88.8) | 824 (77.5) | 350 (79.9) | 2918 (84.2) |
| Do not know | 9 (0.5) | 10 (0.9) | 3 (0.7) | 22 (0.6) |
| Worries about getting a UTI when performing IC | ||||
| Yes (daily, weekly, monthly, less than monthly) | 1402 (71.4) | 685 (64.4) | 285 (65.1) | 2372 (68.5) |
| Never | 464 (23.6) | 337 (31.7) | 134 (30.6) | 935 (27.0) |
| Do not know | 97 (4.9) | 41 (3.9) | 19 (4.3) | 157 (4.5) |
| Worries about not emptying bladder completely when performing IC | ||||
| Yes (daily, weekly, monthly, less than monthly) | 946 (48.2) | 487 (45.8) | 204 (46.6) | 1637 (47.3) |
| Never | 892 (45.4) | 538 (50.6) | 208 (47.5) | 1638 (47.3) |
| Do not know | 125 (6.4) | 38 (3.6) | 26 (5.9) | 189 (5.5) |
| Number of years performing IC | ||||
| Less than 6 months | 19 (1.0) | 28 (2.6) | 11 (2.5) | 58 (1.7) |
| 6–12 months | 40 (2.0) | 57 (5.4) | 19 (4.3) | 116 (3.3) |
| 1–2 years | 134 (6.8) | 132 (12.4) | 50 (11.4) | 316 (9.1) |
| 3–4 years | 235 (12.0) | 276 (26.0) | 93 (21.2) | 604 (17.4) |
| 5–10 years | 466 (23.7) | 324 (30.5) | 165 (37.7) | 955 (27.6) |
| 10+ years | 1065 (54.3) | 245 (23.0) | 99 (22.6) | 1409 (40.7) |
| Do not know | 4 (0.2) | 1 (0.1) | 1 (0.2) | 6 (0.2) |
| Number of catheterisations per day | ||||
| 1 time | 25 (1.3) | 49 (4.6) | 11 (2.5) | 85 (2.5) |
| 2 times | 94 (4.8) | 104 (9.8) | 39 (8.9) | 237 (6.8) |
| 3 times | 138 (7.0) | 131 (12.3) | 57 (13.0) | 326 (9.4) |
| 4 times | 348 (17.7) | 217 (20.4) | 92 (21.0) | 657 (19.0) |
| 5 times | 542 (27.6) | 210 (19.8) | 98 (22.4) | 850 (24.5) |
| 6 times | 470 (23.9) | 180 (16.9) | 84 (19.2) | 734 (21.2) |
| 7 times or more | 344 (17.5) | 170 (16.0) | 56 (12.8) | 570 (16.5) |
| Do not know | 2 (0.1) | 2 (0.2) | 1 (0.2) | 5 (0.1) |
| Haematuria | ||||
| Yes | 669 (34.1) | 388 (36.5) | 132 (30.1) | 1189 (34.3 |
| No | 1221 (62.2) | 635 (59.7) | 287 (65.5) | 2143 (61.9) |
| Do not know | 73 (3.7) | 40 (3.8) | 19 (4.3) | 132 (3.8) |
Among individuals who had UTIs, 1976 out of 3464 reported their number of UTIs within the last year
IC=intermittent catheterisation, UTI=urinary tract infections
Compared with non-NLUTD cases, cases with NLUTD were slightly younger, were female, experienced retention and incontinence, suffered from bowel issues, were experienced IC users, and performed IC every day. Overall, 89.3% used additional IC technique to assist bladder emptying when using IC, 84.2% of the study population had a UTI since starting IC, 64.5% reported 1-3 UTIs within the last year, and the overall UTI level was 1.88 UTIs per year (95% CI: 1.71-2.07). UTIs also affected QoL, in that 68.4% worried about acquiring a UTI and 47.3% worried about not emptying their bladder completely during IC.
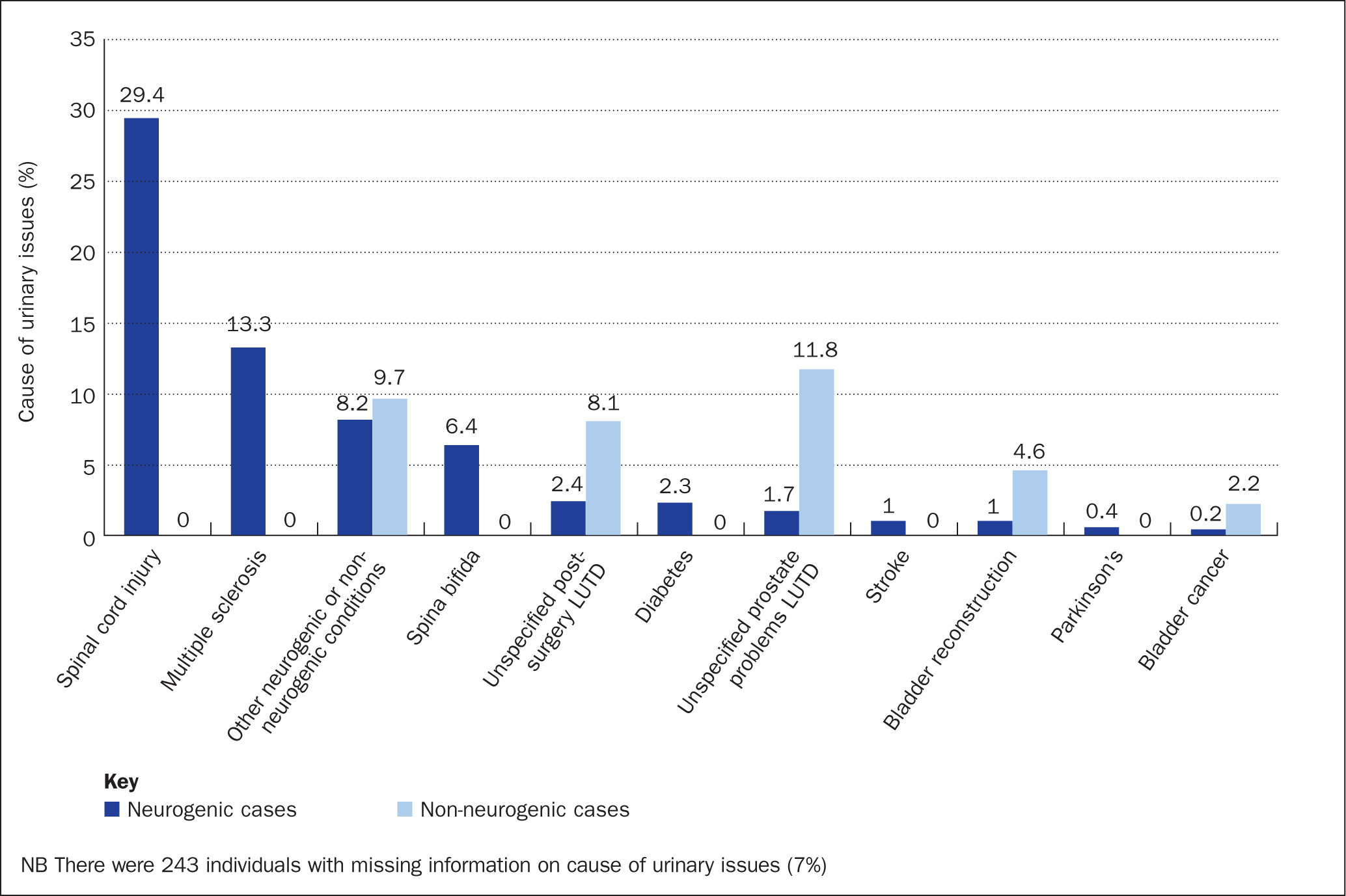
Among individuals with NLUTD, spinal cord injuries were the primary cause of urinary issues (29.4%), followed by multiple sclerosis (13.3%), other neurogenic conditions (8.2%), spina bifida (6.4%), diabetes (2.3%), stroke (1.0%), and Parkinson's (0.4%) (Figure 2). Individuals with non-NLUTD mainly reported unspecified prostate problems of LUTD (11.8%) as the cause of urinary issues, followed by other non-neurogenic conditions (9.7%), unspecified post-surgery LUTD (8.1%), bladder reconstruction (4.6%), and bladder cancer (2.2%).
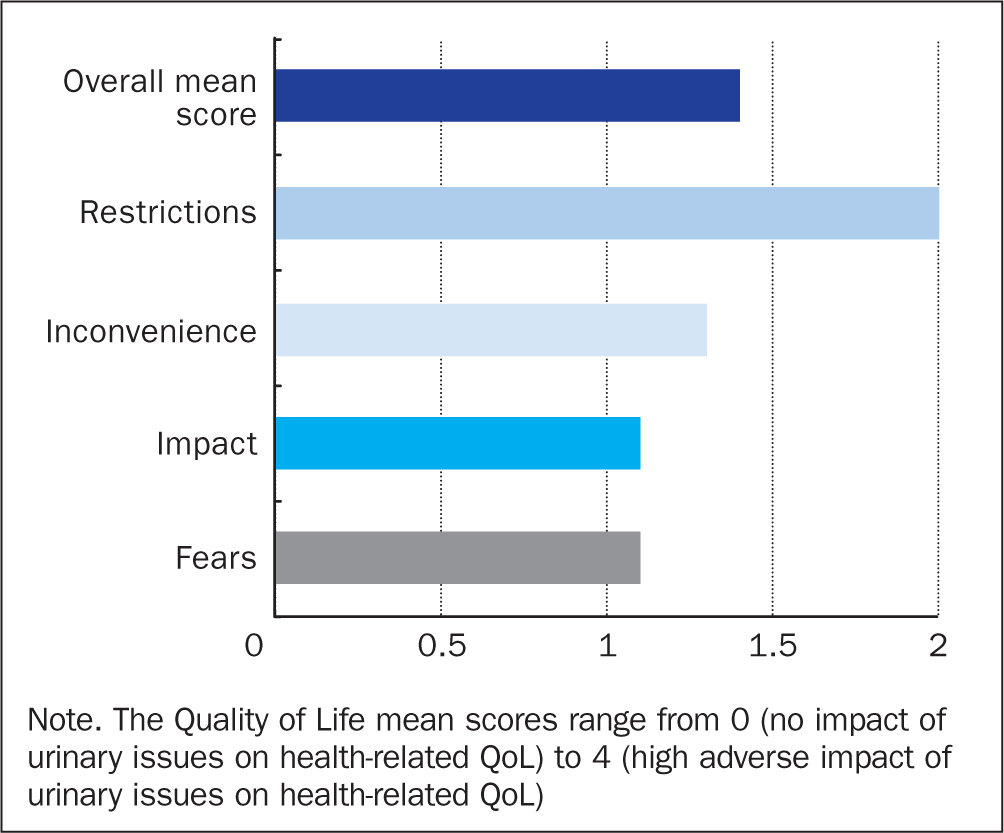
Based on the QoL mean scores, being bothered by restrictions, defined as the frequency of limitations due to urinary issues, had a higher impact on all individuals' QoL compared with the other domains (Figure 3).
There was a 37% lower risk for UTIs in individuals without haematuria (RR: 0.63; 95% CI: 0.55-0.71), a 17% lower risk for UTIs when the bladder was perceived empty (RR: 0.83; 95% CI: 0.72-0.96), a 14% lower risk for UTIs in the absence of bowel dysfunctions (RR: 0.86; 95% CI: 0.76-0.98), and a 30% lower risk of UTIs in males (RR: 0.70; 95% CI: 0.62-0.79) (Table 2).
Table 2. Relative risks (RR) and 95% confidence intervals (95% CI) of urinary tract infections (UTIs) in patient-reported risk factors for UTIs (n=2100)
| Risk factors for urinary tract infections | Adjusted RR | P value |
|---|---|---|
| Not having haematuria versus having haematuria | 0.63 (0.55–0.71) | <0.001 |
| Not having perceived residual urine versus having perceived residual urine | 0.83 (0.72–0.96) | 0.012 |
| Not having bowel issues versus having bowel issues | 0.86 (0.76–0.98) | 0.027 |
| Male versus female | 0.70 (0.62–0.79) | <0.001 |
NB Relative risk (RR) estimates obtained in a combined model were adjusted for haematuria, perceived residual urine, bowel issues, sex, and country
Overall, individuals who reported risk factors for UTI had a significantly lower QoL. Lower QoL were observed when individuals experienced haematuria (mean difference: 0.19; 95% CI: 0.13-0.25), perceived residual urine (mean difference: 0.29; 95% CI: 0.22-0.36), experienced bowel issues (mean difference: 0.21; 95% CI: 0.15-0.27), were female (mean difference: 0.11; 95% CI: 0.05-0.17), applied additional IC technique to empty their bladder (mean difference: 0.18; 95% CI: 0.09-0.28), and had recurrent UTIs (mean difference: 0.22; 95% CI: 0.16-0.28) (Table 3).
Table 3. Mean difference and 95% confidence intervals (95% CI) of quality of life (QoL) score in patient-reported risk factors for urinary tract infections (n=2062)
| Risk factors for urinary tract infections (UTIs) | Adjusted mean difference | P value |
|---|---|---|
| Not having haematuria versus having haematuria | 0.19 (0.13–0.25) | <0.001 |
| Not having perceived residual urine versus having perceived residual urine | 0.29 (0.22–0.36) | <0.001 |
| Not having bowel issues versus having bowel issues | 0.21 (0.15–0.27) | <0.001 |
| Male versus female | 0.11 (0.05–0.17) | <0.001 |
| Not using additional IC technique versus using additional IC technique | 0.18 (0.09–0.28) | <0.001 |
| Not having recurrent UTIs versus having recurrent UTIs | 0.22 (0.16–0.27) | <0.001 |
NB Mean difference estimates obtained in a combined model were adjusted for haematuria, perceived residual urine, bowel issues, sex, country, additional IC technique, age, and recurrent UTIs
Discussion
In this cross-sectional population-based study among individuals using IC, there was a lower risk of UTIs when haematuria and bowel issues were absent, when the bladder was perceived empty, or if individuals were male. QoL was lower for individuals who had haematuria, perceived residual urine, bowel issues, were female, applied additional IC techniques, and had recurrent UTIs.
Haematuria can be a sign of UTIs, but can also be caused by performing IC (Kennelly et al, 2019; Engberg et al, 2020), because urethral trauma may occur due to the IC procedure (Engberg et al, 2020). However, as data were collected at one time point and were also patient reported, it cannot be determined whether haematuria was caused by UTIs or IC. Indeed, catheter coating can also play an important role in individuals' use of IC and using an optimal coating is associated with a reduction in urethral microtrauma, strictures, adverse events and UTIs, as well as improved preference, satisfaction and QoL (Barken and Vaabengaard, 2022; Liao et al, 2022). In line with previous research, the findings of this study suggest that absent haematuria is linked to a lower risk of UTIs (Kennelly et al, 2019; Engberg et al, 2020; Liao et al, 2022), emphasising the importance of preventing haematuria.
Despite lack of consensus on a clinically relevant residual urine threshold, residual urine has been recognised as a possible UTI risk factor by individuals using IC (Kennelly et al, 2019). Emptying one's bladder with IC can be challenging due to anatomical bladder abnormalities, choice of inadequate product design for the specific individual, incorrect handling of catheter, removing the catheter prematurely, and insufficient IC education (Kennelly et al, 2019). Regardless of underlying cause, inefficient bladder emptying may increase the UTI risk, especially in predisposed individuals (Vasudeva and Madersbacher, 2014). The current study shows a lower UTI risk in individuals perceiving their bladder as empty, supporting perceived residual urine as a possible risk factor and suggesting that the bladder should be emptied as much as possible. This is further supported by clinical guidelines recommending thorough emptying with IC (Vahr et al, 2013).
Experiencing urinary tract symptoms, bowel dysfunction and UTIs have been shown to significantly impact QoL due to the restrictions experienced from physical, mental and social aspects (Patel et al, 2016; Hearn et al, 2018; Emmanuel, 2019; Welk, 2020; Truzzi et al, 2022). A lower risk of UTIs was observed when bowel issues were absent in the current study, which is in line with the evidence on bowel dysfunction as a potential UTI risk factor (Kennelly et al, 2019).
In the current study, individuals were significantly influenced by restrictions due to urinary issues, which were defined by frequency of limitations, such as, for example, going out without planning anything in advance or thinking one's life is regulated by bladder problems. A minimal important difference in QoL of 0.5 (range: 0.36-0.72) has previously been suggested (Bonniaud et al, 2008). However, the QoL scores observed in this study did not correspond to this minimal important difference. Still, individuals seemed to feel significantly restricted by urinary issues and their QoL was also affected, thus, emphasising that urinary issues can be burdensome in individuals using IC despite not reaching the minimal important difference (Patel et al, 2016; Crescenze et al, 2019).
Even though the associations between patient-reported UTI risk factors in relation to UTI and QoL were significant, it is important to keep in mind that the collected data are cross-sectional. A direct causality of the observed associations therefore cannot be established, nor can temporal associations between exposures, potential confounders and outcomes be determined. Neurological patients can have reduced sensitivity and the perception of having an empty bladder may therefore depend on the preserved sensation in LUTD, which can vary between different patient groups (Musco et al, 2022). Thus, self-reported data on residual urine may depend on individual sensitivity and there may be a risk of misclassification.
In general, different UTI definitions exist and are applied differently in practice and research in individuals with neurourological conditions. This has highlighted the need for a generally accepted UTI definition, as individuals may be categorised differently across studies, making comparisons more challenging (Berger et al, 2022; Sartori et al, 2022). In addition, there is a general risk of selection bias, because individuals who have voluntarily registered to participate in the online survey may have a healthier status and this would therefore be likely to cover more competent IC users. This is supported by the descriptive data showing that half of the study population had performed IC for more than 10 years and more than 4 times per day. Because the study does not include data on IC difficulty before catheter insertion into the bladder, but rather after insertion, it does not capture those with IC difficulties, which could otherwise show more about the IC users' competencies with IC.
Another important observation when using an exploratory statistical approach was that, when adjusting for NLUTD, this was not associated with UTI risk, as opposed to findings from another recent study (Welk et al, 2022). Therefore, the researchers were not able to assess potential differences among distinct patient profiles, such as in NLUTD versus non-NLUTD. Thus, the current study population may represent a selected and more competent patient group, who are generally at lower risk of UTIs, which may lead to underestimation of the actual impact of patient-reported UTI risk factors and QoL. In addition, as the sources from where individuals were recruited include anyone using IC and who had originally signed up for surveys and news, this led to a broad reach-out. Not surprisingly, the majority of individuals contacted with an invitation to take part (n=48 277) did not start the survey and because the survey was active for a short period only (March to April 2022), the response rate of 6% was consequently low.
Strengths of this study include the large number of individuals who perform IC regularly, representing individuals with both NLUTD and non-NLUTD across 13 countries, which provides adequate and varied data to investigate several well-established patient-reported UTI risk factors. Furthermore, the study was based on self-reported data obtained through a comprehensive list of questions related to several urinary issues, medical history, bladder emptying, bowel issues, worries, and QoL-related questions based on the validated Qualiveen-30 questionnaire (Bonniaud et al, 2006). The subjective data are valuable in terms of gaining insights into patients' lived experience and reflections on IC use and related challenges.
Conclusion
Significant associations between previously identified UTI risk factors such as haematuria, perceived residual urine, bowel issues, and additional emptying techniques were associated with a higher UTI risk and lower QoL. This study provides real-life, patient-reported insights on identification of symptoms, which can bring guidance for health professionals in terms of re-evaluating IC procedures, as individuals may change behaviour or adherence throughout time, leading to more UTIs and lower QoL. Further longitudinal research, including a large heterogenous study population of both experienced and inexperienced IC users, is needed to expand findings from the present study and to identify manageable risk factors to improve QoL for individuals using IC.
KEY POINTS
- This patient survey looked at urinary tract infections and quality of life in individuals carrying out intermittent catheterisation
- Poor quality of life was associated with experiencing blood in the urine, residual urine, bowel dysfunction, recurrent urinary tract infections, being female, and when applying specific withdrawal techniques
- Having no symptoms was associated with a lower risk of urinary tract infections
- Patient-reported data can provide valuable real-life insights and help health professionals in identifying and treating symptoms of urinary tract infections
- Intermittent catheterisation procedures should be re-evaluated over time, because individuals may change their level of adherence to treatment
CPD reflective questions
- Can a measurement of quality of life be used as indication of whether individuals with lower urinary tract dysfunction need help with their bladder-emptying routine?
- How can individuals with lower urinary tract dysfunction be assisted in identifying urinary tract infection symptoms?
- Should individuals with lower urinary tract dysfunction have their intermittent catheterisation procedures re-evaluated through time?


