Compression therapy is essential for lymphoedema management (Badger et al, 2020; Executive Committee of the International Society of Lymphology (ISL), 2020). Compression therapy using elastic stockings or multilayer bandaging requires continuous self-care, so it is essential that health professionals educate patients on this. However, in practice, compression therapy self-care can be difficult. Reasons for this include physical limitations, psychosocial issues and a lack of knowledge (Chitambira, 2019). In particular, a lack of knowledge may be a barrier to patients starting or continuing with compression therapy.
Self-care is a routine health behaviour that patients need to follow. Health professionals' first intentions in self-care education are to improve patients' awareness of their illness and address their lack of knowledge to help them understand their condition. This approach is suggested in the middle-range theory of self-care support in chronic disease (Blok, 2017; Riegel et al, 2018; Khademian et al, 2020). Under this theory, symptoms are viewed as being important to monitor and as giving direction to self-care management behaviour; in other words, when symptoms worsen, patients can use different management strategies, such as changing medication or diet or consulting a clinician.
The authors focused on this theory for supporting self-care for patients with lymphoedema, especially those using compression therapy. Implementing compression therapy as self-care in lymphoedema requires patients to be aware they have the condition, decide to purchase compression therapy products and engage in the health behaviour of wearing them daily.
Self-care education for patients with lymphoedema is provided by physicians, nurses and certified lymphoedema therapists. These practitioners provide general knowledge about lymphoedema, using information leaflets and demonstrating basic self-care techniques. While this is generally done for all patients, it can still be difficult for individuals to fully recognise that lymphoedema is their problem. Therefore, the authors attempted to apply middle-range theory to lymphoedema self-care education and use real-time image sharing to assist patients in understanding lymphoedema and recognising how the disease is affecting them.
Real-time image sharing education is a method of showing and explaining images to the patient in real time using two techniques: indocyanine green lymphography (ICG) and ultrasonography. It is expected to improve awareness and understanding of the disease and lead to better health behaviour.
ICG is one of the standard methods of diagnosing lymphoedema (Mihara et al, 2013, 2014; Narushima et al, 2016). ICG, which involves a fluorescence spectrum of 800–830 nm, expresses molecular fluorescence by binding to plasma proteins in lymphatic vessels, and a camera captures images of stagnant lymphatic areas. Being able to observe the stagnation of lymphatic circulation in their own affected limb allows patients to recognise that they have lymphoedema.
Ultrasound images can be used to assess lymphoedematous status (Dai et al, 2013; Suehiro et al, 2014; 2016; 2017; Tashiro et al, 2017) and its relationship to cellulitis (Dai et al, 2016; 2021), and are useful in providing an understanding of the condition of lymphoedema. These images allow fluid retention and fat accumulation in the skin and subcutaneous tissue to be observed. The ability to observe the lymphoedema-specific condition of skin and subcutaneous tissue in their own affected limb gives patients a clear understanding of their condition. This may lead to patient decision-making and behaviour change regarding compression therapy.
In this study, the authors report a case in which real-time image sharing education promoted decision-making and behaviour change in a patient with lower extremity lymphoedema who could not manage elastic stockings.
Case study
The study protocol was approved by the medical ethics committee of the University of Tokyo (#2020287NI) and the authors gained written consent from the patient.
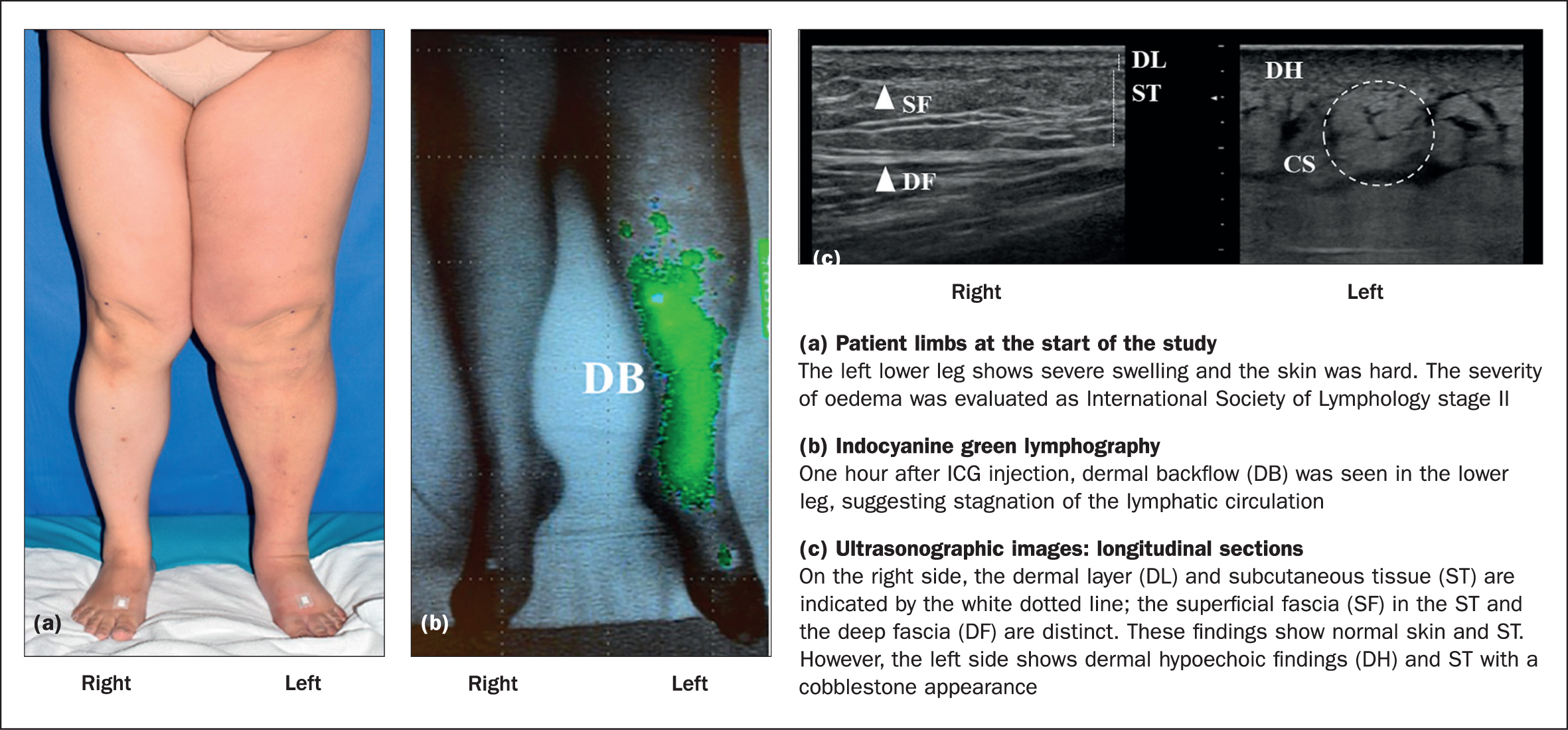
The patient, a 51-year-old woman with a BMI of 31.7 kg/m2 and a history of hypertension and diabetes, had had secondary left lower extremity lymphoedema for 5 years after she had undergone a hysterectomy, pelvic lymph node dissection and radiation therapy for cervical cancer. She had developed cellulitis twice within a year. and had stage II lymphoedema according to the ISL (2020)(Figure 1a).
The treatment plan was that she would learn conservative therapy to control the oedema. This involved the use of compression stockings and continued self-care behaviour after which lymphovenous anastomosis would be considered.
Although the patient agreed to the treatment plan through regular self-care education, she had been unable to practise self-care for 5 years and her condition worsened. Self-care instructions were given; however, the patient did not purchase elastic stockings and only occasionally wore commercially available weak-pressure elastic stockings. Regarding compression therapy, she said:
‘I do not understand the significance of wearing elastic stockings. I cannot make the effort to wear them or to continue to do so.’
This was thought to be because the patient did not recognise that she had lymphoedema in her lower limb, so did not know of the risks and that she needed to wear elastic stockings. Furthermore, she did not understand the condition, so was unable to make a decision on compression therapy, which prevented her from engaging in self-care behaviour.
In this patient, the periapical diameter of the lymphoedema was likely to increase along with the risk of cellulitis, which would make it more difficult to carry out the treatment plan.
Therefore, the authors decided to educate the patient using real-time image sharing. This was intended to promote recognition of illness and an understanding of lymphoedema, in the hope that it would lead to behavioural changes.
First, plastic surgeons performed ICG (PDE NEO, Hamamatsu Phonics, Japan) imaging. A physician injected 0.2 ml of ICG (0.5 mg) into the dorsum of the foot (saphenous lymphatics) and the proximal side of the lateral condyle (lateral calf lymphatics) and, 1 hour later, the lymph flow was shown on the monitor. Dermal backflow (DB) was seen in the lower leg (Figure 1b), suggesting stagnation of lymphatic circulation. The image confirm the diagnosis and provided a better understanding of the patient's condition. The image was shared with the patient to explain stagnation of lymphatic circulation in real time. ICG revealed dermal backflow in the patient's left leg.
Next, a researcher with a certified lymphoedema therapist carried out ultrasound imaging (Noblus, Hitachi Aloka, Japan) to show the dermis and subcutaneous conditions in real time. To do this, a linear probe was coated with gel and placed on the skin, and the echo reflection showed the properties of the dermis and subcutaneous tissues. The researchers used a 10–18 MHz linear probe to obtain longitudinal images.
The ultrasound images in Figure 1c show longitudinal sections of the medial site (10 cm below the knee). Ultrasonography showed a cobblestone effect in the left leg and dermal hypoechogenicity. The images were shared with the patient.
Immediately after sharing the ICG and ultrasound images with the patient, the authors assessed her understanding and awareness. They also assessed self-care behaviour and circumferences monthly for a period of 4 months.
Immediately after the ICG and ultrasound images had been viewed and explained to the patient, she said:
‘I noticed that I had moderately severe lymphoedema.’
‘I was well aware that I needed to wear elastic stockings.’
‘I saw skin findings that were associated with cellulitis, and I knew I had to wear them properly in case I got cellulitis again. I don't want cellulitis to recur.’
After the patient understood why compression therapy was necessary, the authors emphasised the goal of continuous use of low-pressure stockings that covered her up to the waist during the daytime.
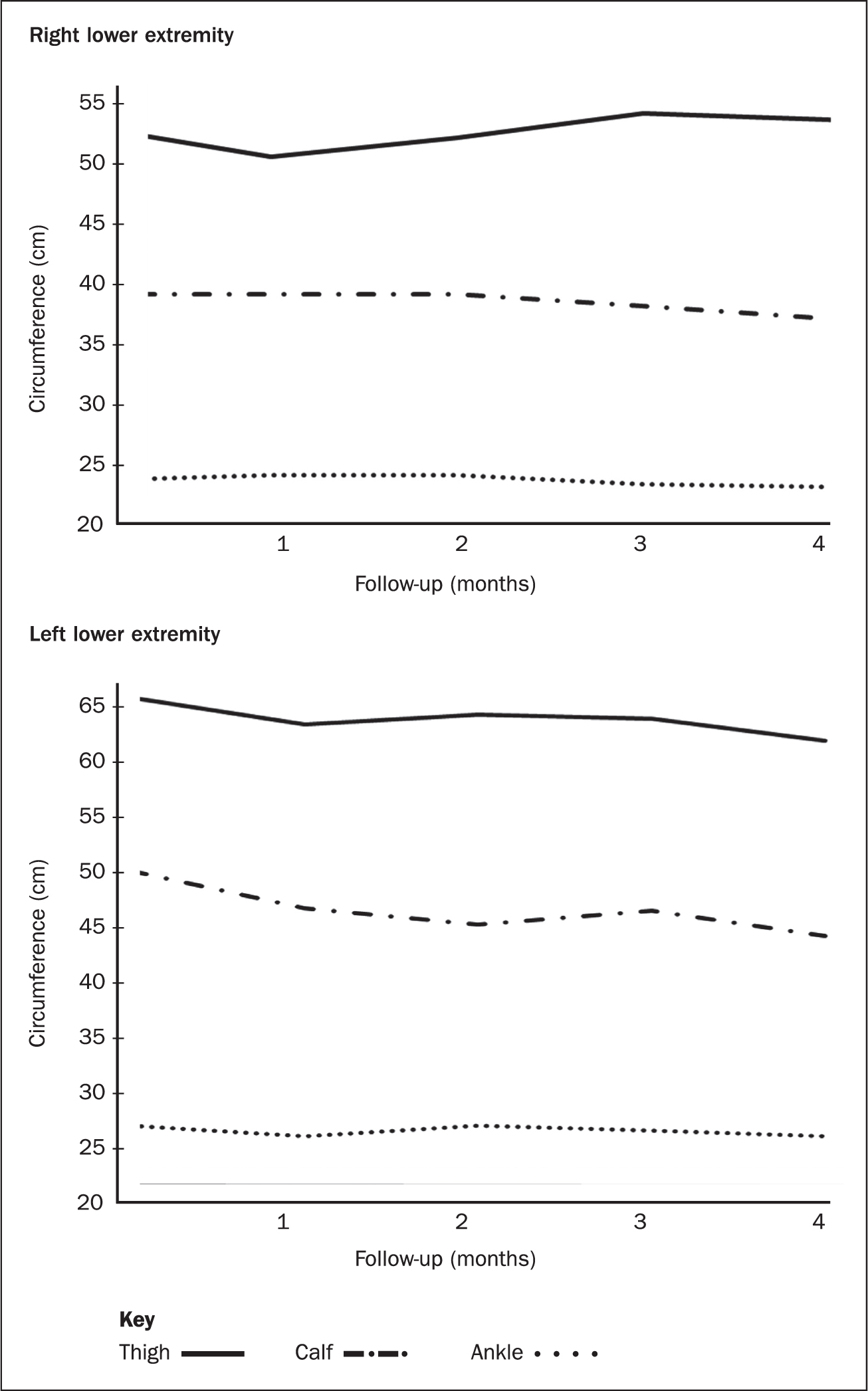
After 1 month, the patient was able to wear weak pressure stockings daily. The circumferences of the oedematous limb had decreased.
At month 3, she decided to purchase elastic stockings (Airbo Wave, Three Gentleness Medical, Japan) for her left leg to wear at night and at home. These are flat-knit elastic stockings composed of 82% cotton, 10% polyurethane and 8% polyester. The compression value at the time of application was 25 mmHg measured by Pico Press (Microlab, Italy).
A month 4, the patient was able to continue wearing elastic stockings daily, and her thigh, lower leg and ankle circumferences decreased.
Her progress was monitored monthly for 4 months and, over this time, limb circumference decreased progressively (Figure 2). The patient did not develop cellulitis during this follow-up period.
Discussion
This case demonstrates the effectiveness of real-time image-sharing education using ICG and ultrasonography to promote self-care in patients with lymphoedema of the lower extremities who cannot start compression therapy. It could result in behavioural changes so patients start and continue to wear elastic stockings.
The patient, whose oedema was at ISL stage II, was able to continue wearing elastic stockings daily for 4 months, and the circumference of her limb decreased. Furthermore, she did not develop cellulitis during this period.
Although this patient had previously received general self-care education, she was not willing to wear stockings and was unable to continue the treatment plan. This, according to self-care theory (Choi et al, 2014; Riegel et al, 2021) relates to the middle-range theory of self-care of chronic illness (Blok, 2017; Riegel et al, 2018; Khademian et al, 2020). Non-adherence with self-care may have been a result of inadequate awareness of the disease.
ICG and ultrasound images are characterised by their ability to show images in real time that are easy to understand. ICG and ultrasound imaging have been found to be useful for selecting treatment and care based on diagnosis (Mihara et al, 2013; 2014; Narushima et al, 2016) and assessment of oedema status (Dai et al, 2013; Suehiro et al, 2014; 2016; 2017; Tashiro et al 2017). In this case, the patient had dermal backflow in the lower leg, which indicated stagnant lymphatic circulation.
Showing the dermal backflow (Mihara et al, 2013; 2014; Narushima et al, 2016) clearly in green may have helped the patient to understand the differences between her left and right legs.
Ultrasound imaging showed hypoechoic findings in the dermis (Dai et al, 2016), obscuring the layered structure of the subcutaneous tissue, and giving it a cobblestone appearance (Suehiro et al, 2014; 2016; 2017; Tashiro et al 2017). The hypoechoic findings in the dermis are suggestive of interstitial fluid accumulation, which is suspected to be related to a history of cellulitis. In addition, the cobblestone appearance of the subcutaneous tissue shows it contains fat, fibrous tissue and excessive interstitial fluid (Tashiro et al, 2017). The ultrasound images may have provided a better understanding of the oedema condition, as the changes specific to the patient could be seen clearly.
Regarding clinical application, real-time sharing of such images could increase patients' awareness of their disease. Real-time image-sharing education, where ICG and ultrasound are used initially, followed by periodic assessment with ultrasound, could be implemented in clinical practice in lymphoedema outpatient clinics, after cancer treatment and in rehabilitation and home-care settings.
However, these devices need to be installed and health professionals need the knowledge and technical skills to use them, which incur costs. Deployment in all hospitals is likely to be difficult in the immediate future but, where these are available, it may be possible to share these images with patients and explain them.
Limitations
While this case was ISL stage II and lymphoedema-specific findings could be observed on the images, the images may appear different when used for early diagnosis and assessment, or for those with a milder stage of the disease.
This is a one case study. Future research is needed to verify whether real-time image sharing using ICG and ultrasound imaging devices can lead to the development of methods to support the self-care of patients with lymphoedema.
Conclusion
Real-time image-sharing education using ICG and ultrasonography as self-care support for a patients with lymphoedema who cannot start compression therapy could result in behavioural changes, resulting in patients starting and continuing to wear compression stockings.
KEY POINTS
- Compression therapy is important in oedema control in patients with lymphoedema but usual self-care education on this is inadequate
- Self-care is necessary for successful treatment of lymphoedema patients, and nursing practice based on the self-care theory of disease awareness and understanding is important in supporting this
- Real-time image-sharing education by indocyanine green lymphography (ICG) and ultrasonographic images can provide an alternative education in self-care for patients with low adherence to this
- ICG shows stagnation in the lymphatic circulation, while ultrasound imaging depicts specific findings of lymphoedema in the dermis and subcutaneous tissues
- Research is needed to confirm whether the use of ICG and ultrasonography images in educating patients about their lymphoedema would be feasible in future nursing practice
CPD reflective questions
- Do you know of patients with lymphoedema who have difficulty in starting or maintaining self-care?
- How could you implement the real-time image-sharing education for self-care among lymphoedema patients?
- How do you think training for healthcare professionals in promoting self-care education should be implemented?


