The cardiovascular system, as the name indicates, consists of the heart (cardio) and blood vessels (vascular). The heart acts as a pump responsible for the consistent and uninterrupted flow of blood, whereas the blood vessels provide the vast network through which blood is transported throughout the body (Waugh and Grant, 2018). The main functions of the cardiovascular system are the circulation of blood to and from the tissues, organs and systems of the body and the removal of waste products of metabolism (McCance, 2019; Dutton and Elliott, 2021). The blood is responsible for the transportation of nutrients, oxygen, carbon dioxide, waste products of metabolism, water, electrolytes, hormones and other blood products to the target organs (Dutton and Elliott, 2021). It is important to note that the lymphatic system is closely linked to the cardiovascular system and enhances its functionality (Waugh and Grant, 2018; McCance, 2019). Blood flow through the extensive vascular network is achievable only with the aid of sufficient pressure exerted on the blood vessels by the pumping action of the heart (Banasik, 2019)
Location of the heart
The heart is located near the midline of the thoracic cavity, commonly known as the mediastinum, and rests on the diaphragm (Cook et al, 2021). The mediastinum is the space in the centre of the thorax located between the right and the left lungs. The heart lies towards the left-hand side of the thoracic cavity, with the apex pointing towards the left hip and resting at the level of the fifth intercostal spaces (Marieb and Keller, 2018). It has been estimated that the size of the heart is about the size of the owner's clenched fist, measuring about 12 cm long and 9 cm wide (Nair, 2018). In men, the heart weighs approximately 250–390 g, whereas in women, it weighs 200–275 g) (Marieb and Hoehn, 2018).
Structure of the heart
The wall of the heart is made up of three layers: the pericardium, the myocardium and the endocardium (Peate and Nair, 2015; Waugh and Grant, 2018). The pericardium is the double-walled outer fibrous membrane enclosing the heart whose role includes anchoring the heart to the surrounding structures, protecting the heart and preventing it from overstretching or overfilling with blood during systole (Marieb and Hoehn, 2018). The outer layer of the pericardium is a fibrous sac, referred to as the parietal pericardium, whereas the inner layer, a serous membrane, is referred to as the visceral pericardium or epicardium (Peate and Nair, 2015). A thin film of serous fluid separates the two layers and is referred to as the pericardial cavity, containing between 10 ml and 30 ml of pericardial fluid. This fluid allows the heart to move freely without friction (McCance, 2019).
The myocardium is the middle layer of the heart wall and the thickest layer. It is also referred to as the cardiac muscle because its muscular contractions facilitate the ejection of blood from the heart chambers (Dutton and Elliott, 2021). The endocardium forms the innermost layer of the heart. It consists of thin, smooth endothelium and connective tissue that allows smooth flow of blood (Waugh and Grant, 2018). The endothelial layer releases antithrombotic factors, which inhibit blood from adhering to the endocardium (Dutton and Elliott, 2021).
The chambers of the heart
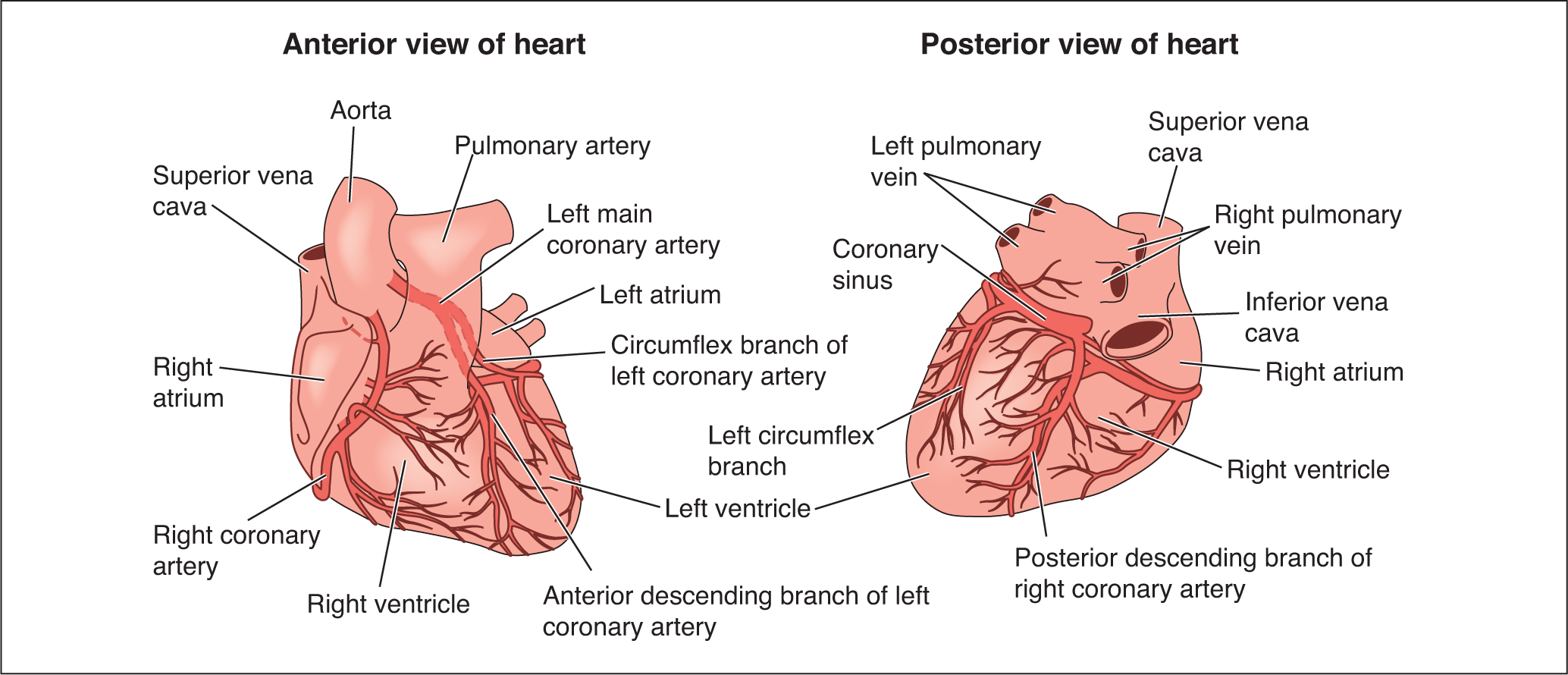
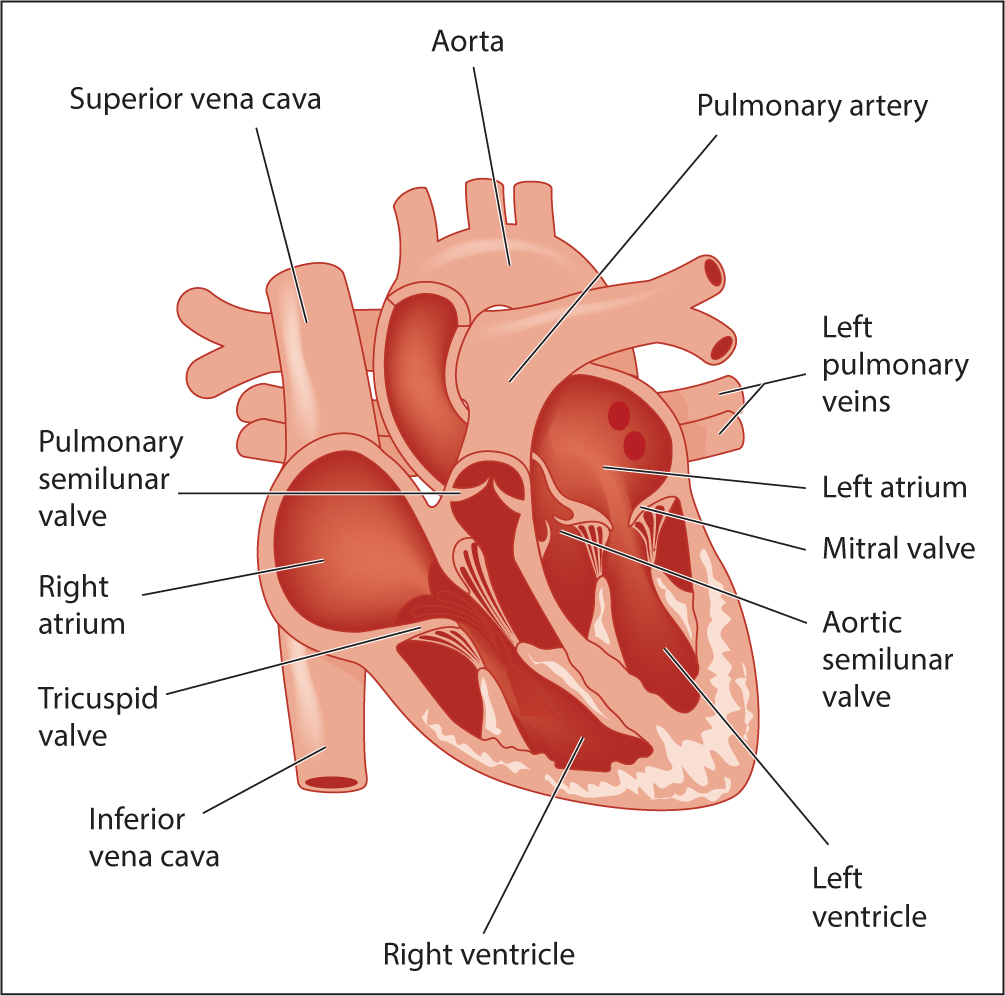
The heart is divided into right and left side and is composed of four chambers: the right atrium, the left atrium, the right ventricle and the left ventricle (Nair, 2018) (Figure 1 and Figure 2). The left and right side of the heart are separated by a wall referred to as the septum. This septum prevents the oxygen-rich blood of the left-hand side of the heart from mixing with the oxygen-poor blood of the right-hand side of the heart (Tortora and Derrickson, 2017). The two upper chambers are referred to as the right atrium and left atrium (plural: atria) and the two lower chambers are referred to as right and left ventricles (Banasik, 2019). It is important to note that the atria are thinner and smaller than the ventricles. The ventricles form much of the bulk of the heart and have a thicker myocardial layer. The thickness of each chamber is directly proportional to the resistance that needs to be overcome before ejection of blood from the chambers (Hubert and VanMeter, 2018). Hence the ventricular walls are thicker because of the enormous resistance that must be overcome before ejecting blood into the pulmonary and the systemic vessels.
Fibrous skeleton of the heart
There are four dense fibrous rings known as annuli fibrosi cordis that form anchorage for the firm attachments of the atria and the ventricles tissues as well as the valvular tissues (McCance, 2019).
Valves of the heart
The valves of the heart ensure one-way flow of blood through the chambers of the heart (Peate and Nair, 2015). The valves preventing back-flow of blood from the ventricle to the atria are known as atrio-ventricular valves. The valve on the right side of the heart is called the tricuspid valve because of its three cusps and the valve on the left hand side is called the bicuspid or mitral valve because of its two cusps (Cook et al, 2021). In the aorta and in the pulmonary artery there are also valves, which serve similar purposes to the atrioventricular valves. These are known as semilunar valves (Marieb and Hoehn, 2018).
Blood flow through the heart
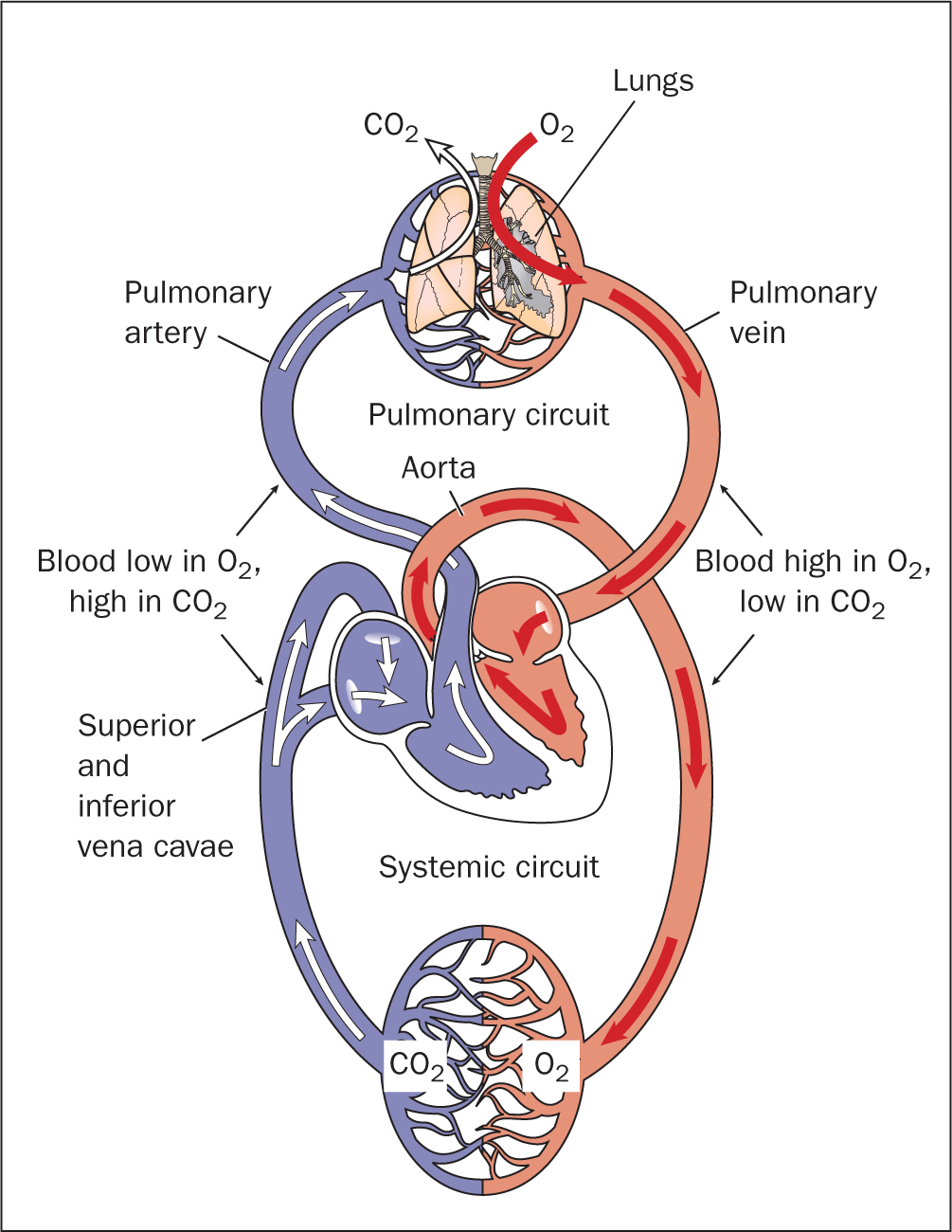
There are three main types of vessels that transport blood to and from the heart. These are the arteries, the veins and the capillaries. The arteries carry blood away from the heart and the veins carry blood to the heart. Blood vessels have been described as a closed delivery system originating from the heart and terminating at the heart (Martini et al, 2014). Blood flows into and out of the heart via several large vessels. Deoxygenated blood from the systemic circulation is transported back to the heart through the superior and inferior venae cavae into the right atrium and is emptied into the right ventricle via the tricuspid valve (Nair, 2018; Banasik, 2019). The blood is then pumped from the right ventricle into the pulmonary arteries, and on to the right and left lungs for oxygenation. Exchange of gas occurs at the capillary–alveolus interphase in the lungs leading to oxygen being absorbed and carbon dioxide exhaled (Waugh and Grant, 2018). The oxygenated blood from the lungs is transported to the left atrium via the four sets of pulmonary veins and from the left atrium, the blood is pumped into the left ventricle via the biscupid (mitral) valve. Oxygenated blood from the left ventricle is ejected into the aorta via the semilunar valves and from the aorta travels to the systemic vessels that supply the body (Tortora and Derrickson, 2017). It is this transportation of blood from the right ventricle to the lungs and from the lungs to the left atrium that is commonly referred to as the pulmonary circulation (Marieb and Keller, 2018). The systemic circulation, on the other hand, refers to the transportation of blood from the left ventricle through the aorta to the systemic vessels of the body and its subsequent return to the right atrium via the superior and inferior venae cavae (Marieb and Hoehn, 2018) (Figure 3). It is important to note that the coronary arteries supply the heart tissues with oxygenated blood while the coronary veins return the deoxygenated blood from the heart tissues to the right atrium (Peate and Nair, 2015).
The contraction and relaxation of the myocardial layer of the heart is what constitutes the pumping action of the heart. Each contraction and then relaxation of the myocardial layer of the ventricle is what is referred to as the cardiac cycle (McCance, 2019). When the ventricles relax (diastole) they fill up with blood from the atria, and when the ventricles contract (systole), blood is ejected into circulation.
The conduction system of the heart
The consistency of the cardiac cycle is facilitated by the transmission of electrical impulses through the myocardium of the four chambers of the heart. This is known as the cardiac action potential, which activates the electrical impulses. The conducting system of the heart is composed of the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, the right and left bundle branches and the Purkinje fibres (Tortora and Derrickson, 2017) (Figure 4).
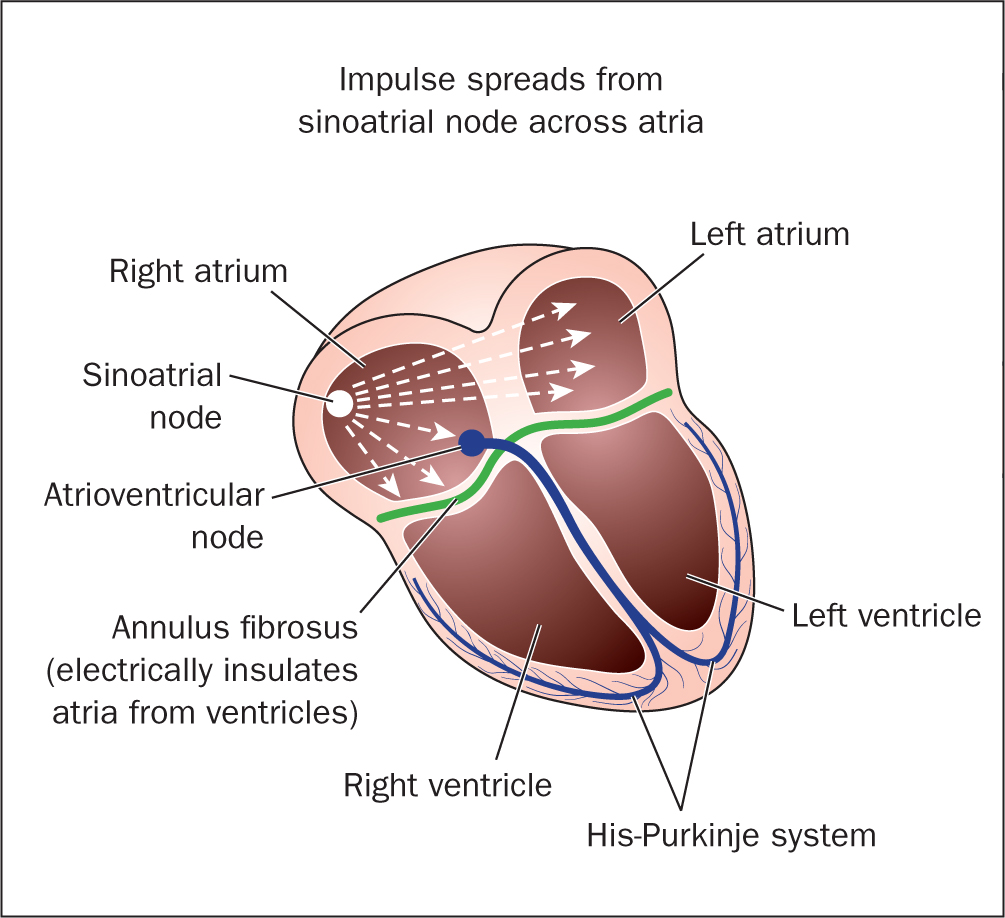
The electrical impulses initiate from the SA node, which is situated in the right atrium near the opening of the superior vena cava. It is often referred to as the natural pacemaker of the heart because its impulses are initiated much faster than the other neuromuscular cells (Peate and Nair, 2015). The impulses of the SA node are responsible for triggering atrial contraction. Electrical impulses pass on from the SA node to the AV node via the posterior internodal pathway, which connects both left and right atria as well as the SA node and the AV node (Edwards, 2014).
The AV node is located at the lower end of the right atrium, which allows it to mediate conduction between the atria and the ventricles. Its unique positioning in the atria means that it is the last area of the atria to be stimulated, allowing enough time for blood emptying into the ventricle before ventricular contraction to ensure there is no back-flow (Peate and Nair, 2015).
On the posterior border of the interventricular septum, the conducting fibres of the AV node merge to form what is known as the bundle of His (AV bundle). The bundle of His divides into two parts forming the left bundle branch and the right bundle branch. The left bundle branch (LBB) travels to the left ventricular apex and the right bundle branch (RBB) travels to the right ventricular apex (McCance, 2019). The terminal branches of the left bundle branch and the right bundle branch are known as the Purkinje fibres. They extend to the ventricular apexes and promote fast distribution of impulses throughout the apices.
The pumping action of the heart is rhythmic in nature and can automatically contract and relax independent of the nerve supply, however, the rate of contraction is influenced by the heart's nerve supply originating from the medulla oblongata (Waugh and Grant, 2018).
Common heart disorders
The cardiovascular system consists of the heart and its blood vessels. The numerous disorders of the cardiovascular system would involve the vessels, the heart structure and the conduction system abnormalities. They include atherosclerosis, myocardial infarction, endocarditis, rheumatic heart disease, cardiomyopathy, heart failure/congestive heart failure, angina and cardiogenic shock. Coronary heart disease (CHD) has been viewed as the most important heart disorder due to the high prevalence in men and women as well as the economic impact (Banasik, 2019). It is also referred to as ischaemic heart disease (IHD) or coronary artery disease (CAD). CAD is one of the main cardiovascular diseases that has affected human populations globally and has been the leading cause of mortality in both the developing and developed world (Malakar et al, 2019). In the USA, CAD causes one in six deaths and the American Heart Association groups heart failure, dysrhythmia, sudden cardiac arrest, myocardial infarction, angina pectoris under the umbrella of CAD (Banasik, 2019). CAD originating from atherosclerosis has been flagged as the primary cause of heart disease (Brashers, 2019). Atherosclerosis results from build-up of plaques in the endothelium of the cardiac arteries supplying the myocardium causing partial or full obstruction of the vessels. Partial obstruction can potentially lead to transient ischaemic events often manifesting during exercise or stress. If left untreated, increasing obstruction results in poor perfusion of the affected tissues and could potentially lead to myocardial infarction (Brashers, 2019). A related disorder of the cardiovascular system is peripheral arterial disease (PAD), which is an atherosclerotic disease of the arteries perfusing the limbs that may progress to claudication.
Myocardial infarction
Myocardial infarction (MI) is a term used for an adverse cardiovascular event caused by formation of plaques or blood clots in the intima of the coronary arteries impeding blood flow to the heart and injuring the myocardium due to lack of oxygen supply (Lu et al, 2015).
Acute MI has been identified as a leading cause of morbidity and mortality worldwide despite improvements made through research and improved lifestyle (Reed et al, 2017). MI is considered to be a medical emergency requiring prompt intervention from medical practitioners in order to achieve a positive outcome for patients (Anderson and Morrow, 2017). Certain factors predispose someone to MI and they include people with past medical history of atherosclerosis, transient ischaemic attack (TIA), smokers, excessive alcohol intake (which contributes to increased level of low-density lipoprotein cholesterol), use of recreational drugs such as cocaine, diabetes, and obesity (Banasik, 2019; Malakar et al, 2019).
Pathophysiology
MI occurs as a result of a blockage in the intima of the coronary artery due to a blood clot or atheromatous plaque. This reduces or impedes blood flow to the heart muscle tissues distal to the affected artery and subsequently cell death (necrosis) due to oxygen deprivation (Edwards, 2014). This damage from lack of oxygen is called an infarct. The extent of the blockage depends on its location, the size of the area of the affected tissue, and the duration of occlusion (Peate and Nair, 2015). Sometimes, the pericardium and endocardium are affected as well (Brashers, 2019).
When the infarct has occurred in the myocardial tissue, a collagen scar forms in the heart tissue, impairing the affected area of the myocardium from contracting efficiently (Hubert and VanMeter, 2018). It also affects the cardiac conductivity, further impairing the effective functioning of the heart, and subsequently leads to impaired tissue perfusion.
Investigations
MI can be diagnosed by carrying out medical investigations such as an electrocardiogram (ECG), angiogram, echocardiogram, chest X-ray and blood chemistry: cardiac enzymes, urea and electrolytes, full blood count, and serum biomarkers, for example, troponin (Banasik, 2019). MIs are categorised into two types depending on the changes indicated on the ECG: ST-segment elevation myocardial infarction (STEMI), usually caused by complete and persisting occlusion of the artery and non-ST segment elevation myocardial infarction (NSTEMI), mostly caused by partial or intermittent occlusion of the artery (Anderson and Morrow, 2017).
Symptoms of MI
The symptoms of MI include chest pain, radiating from left arm to neck, which most patients often describe as an excruciating pain or tightness in the chest, anxiety, shortness of breath (dyspnea), cyanosis, excessive sweating (diaphoresis), nausea, hypotension, vomiting, irregular pulse, fatigue, weakness, stress, depression, signs of shock, loss of consciousness and death (Lu et al, 2015). Evidence seems to suggest that women often present with symptoms that differ from symptoms in men (Mehta et al, 2016). For instance, men will likely manifest with central chest pain whereas women often manifest with pain in the jaw, upper back, neck and arm.
Nursing management of MI
It is pertinent that nurses have sound knowledge of MI to enable them to manage patients safely and effectively (McCance, 2019). Hence, immediate recognition and diagnosis of the condition is of the essence. Prolonged deprivation of oxygen to the heart tissue could lead to cell death. Therefore, nurses must escalate care as soon as a suspected MI is observed. Some of the immediate management procedures will include administering prescribed oxygen, analgesia, vital signs monitoring, reassuring the patient, connecting the patient to a monitor and carrying out airway, breathing, circulation, disability and exposure (ABCDE) assessment (Royal College of Physicians, 2017). Nurses should monitor for signs of shock – for example cyanosis, bradycardia, diaphoresis, tachycardia – and must endeavour to keep accurate records of care given in accordance with the Nursing and Midwifery Council (NMC)(2018) guidance on record keeping.
Treatment of MI
The immediate treatment of MI is taking a resting ECG and initiation of antithrombotic therapy (Anderson and Morrow, 2017). Treatment may differ depending on whether it is NSTEMI or STEMI. For STEMI, the National Institute for Health and Care Excellence (NICE) (2020) advises initiation of a 300 mg loading dose of aspirin immediately and to continue unless contraindicated. Oxygen supplementation should be considered as a priority for patients with hypoxaemia (oxygen saturation of less than 90%), cyanosis or dyspnea (Anderson and Morrow, 2017). Reperfusion therapy (percutaneous coronary intervention (PCI) or fibrinolysis) is also highly recommended depending on eligibility otherwise medical management will be offered (NICE, 2020).
Treatment for NSTEMI also involves an initial antiplatelet therapy of continuous 300 mg loading dose (unless contraindicated) or immediate angiography (NICE, 2020). Unfractionated heparin with dose adjusted to clotting function if creatinine above 265 micromoles/litre could also be considered.
Pain must be managed using glyceryl trinitrate (nitroglycerin) to treat chest pain. Opioid analgesics such as morphine or pethidine can also be administered to relieve pain. Antihypertensive drugs such as beta-blockers, angiotensin-converting enzyme (ACE) inhibitors or calcium channel blockers may also be used to lower blood pressure and to improve the oxygen demand of the heart; however, NICE (2020) guidance advises that calcium channel blockers should no longer be routinely offered as secondary prevention after MI.
Case study
Eunice Watkins (not her real name), a 67-year-old lady presents to the emergency department with chest pain. She reports that the pain started about an hour into her evening light exercises. She describes an ‘agonising pain’ in her mid-sternal region radiating down to her left arm. On a scale of 1–10, with 10 being the most painful, she rates the pain at 5/10. On assessment, the findings were:
- Airway: patent
- Breathing: respiration rate – 36 breaths per minute, oxygen saturation 94%, dyspnea
- Circulation: blood pressure 98/60 mmHg, pulse 102 beats per minute, capillary refill time 3 seconds
- Disability: patient was alert and orientated
- Exposure: temperature 36.5 C, diaphoresis, nausea.
Management would consist of the following:
- Escalation of care depending on the National Early Warning Score 2 (NEWS2)
- Pain management
- Oxygen therapy
- Bed rest
- ECG, echocardiogram, chest X-ray, blood test to check for troponin level and cardiac enzymes – patients presenting with chest pain of suspected cardiac origin should have a resting 12-lead ECG taken as soon as possible (NICE, 2016)
- Medications: aspirin, glyceryl trinitrate, reteplase or alteplase to dissolve clots, anticoagulant such as heparin could be administered to minimise risk of thrombus formation; the NICE (2020) guideline advises that antithrombin drug should be given alongside thrombolysis and antiplatelet therapy.
- Coronary angioplasty might be required to dilate the artery and improve blood flow.
- A urinary catheter might be inserted to monitor fluid balance.
- Record keeping, reassuring patient and good communication.
Summary
This article has described the structure and function of the heart and discussed the common disorders of the heart and the nursing management of a common heart disorder, myocardial infarction. A good knowledge of the normal anatomy and physiology of the cardiovascular system will enable the nurse to apply the nursing process effectively – assessment, diagnosis, planning, implementation and evaluation. Early recognition of deteriorating patients and early intervention facilitates a better outcome for patients (Dutton and Elliot, 2021). There are many cardiovascular disorders and it is beyond the scope of this article to address all the cardiac dysfunctions. Nurses need to recognise the signs and symptoms indicating cardiac disorders so they can act quickly and confidently while delivering high-quality, effective and patient-centred care.
Key Points
- The cardiovascular system consists of the heart, which functions as the ‘pump’, and the vascular networks of vessels that transport blood throughout the body
- Any disease affecting the heart or the vast networks of the vessels would impair the normal physiology of the cardiovascular system
- Plaques can build up in the endothelium layer of the heart potentially causing a disruption in the blood flow
- If left untreated, an infarct can occur in the distal area of any affected vessel and is potentially a life-threatening condition
- Identification of common symptoms associated with cardiac infarction would foster the culture of early intervention among nurses and therefore save lives
CPD reflective questions
- What constitutes the cardiovascular system?
- What is the function of the cardiovascular system?
- What symptoms are associated with myocardial infarction?


