Myeloproliferative neoplasms (MPNs) are clonal stem cell disorders (Hofmann, 2015; Harrison et al, 2017), characterised, in the chronic phase, by an abnormal production of differentiated haematopoietic cells, predominantly of the bone marrow (National Cancer Registry Ireland, 2015; Rumi and Cazzola, 2017; Swerdlow et al, 2017). It results in increased numbers of normal granulocytes, erythrocytes and platelets in peripheral blood (National Cancer Registry Ireland, 2015). Typically a disorder of the older adult, MPNs are classified as rare, with an incidence rate less than 6 per 100 000 persons per year (Rumi and Cazzola, 2017). Typically, 153 new cases of MPN are reported in Ireland each year (National Cancer Registry Ireland, 2015).
There are three main subtypes of MPNs: polycythaemia vera (PV), essential thrombocythaemia (ET) and primary myelofibrosis (PMF) (Harrison et al, 2017). Clinical manifestations vary by subtype but typical symptoms include fatigue, pruritus, night sweats, splenomegaly, abdominal pain and early satiety (Passamonti and Maffioli, 2016). Importantly, PV and ET both convey a high risk of thrombosis and an increased risk of progression to acute myeloid leukaemia (AML) or secondary MF (Mesa and Passamonti, 2016). MPN patients have reduced life expectancy compared with the general population (Paranagama et al, 2018). Data from the US and Global MPN Landmark surveys showed that symptom burden among MPN patients is substantial and negatively affects quality of life (QoL), daily living and productivity (Mesa et al, 2016; Harrison et al, 2017;). The impact on the Irish patient population has not previously been evaluated.
Genomic studies in MPN have identified multiple recurrent somatic mutations, including Janus Kinase-2 (JAK2), calreticulin (CALR) and thrombopoietin receptor (also known as myeloproliferative leukaemia virus (MPL)) (Vainchenker and Kralovics, 2017). Such mutations constitutively activate downstream cell-signalling pathways and have provided new targets for drug development (Viny and Levine, 2014). Despite such advancements, most treatments remain non-curative. Therefore, reduction of symptom burden and improvement of QoL should be considered major treatment goals (Petruk and Mathias, 2020).
Patients with MPNs often require assistance from a caregiver (Paranagama et al, 2018). The physical and psychological impact of caregiving is well established (Schulz et al, 1995). However, limited data are available regarding the burden on caregivers attending to patients with MPNs and this has not previously been assessed in an Irish population. In this article, ‘caregiver’ refers to the person who assists/supports the person with an MPN with daily activities such as shopping, cleaning, cooking, giving medications, toileting assistance and personal care etc.
The authors present the results from the first Irish MPN questionnaire, exploring the impact of the disease and symptom burden on patients and caregivers in the Republic of Ireland.
Method
The methodology used was a cross-sectional questionnaire distributed using convenience sampling to MPN patients and caregivers. The questionnaires were adapted from the Global MPN Landmark Survey (Harrison et al, 2017) and developed by a collaborative working group of advanced nurse practitioners and clinical nurse specialists, supported by Novartis Ireland Limited and endorsed by MPN Voice (https://www.mpnvoice.org.uk/), a UK-based patient group. Patient and caregiver questionnaires were not linked. The patient questionnaire included 29 questions (1 open, 22 closed and 6 Likert scale) and evaluated the experience of living with an MPN. The caregiver questionnaire included 19 questions (1 open, 14 closed and 4 Likert scale) and explored the impact of providing support for the MPN patient.
Patients (18 years and over) with a diagnosis of ET, PV or MF were eligible for participation. Caregivers (18 years and over) who provide care or support to a person with MPN, were eligible for participation. The questionnaires were distributed to attendees at the MPN Voice Patients' Forum held in Cork, Ireland, on 18 May 2019. Two members of the working group distributed the questionnaires (in hard copy). Completed forms (including informed consent) were subsequently collected for analysis. Individual responses were kept confidential and protected by data consolidation. Analyses used descriptive statistics and formal hypotheses were not tested. Research ethics committee approval was not required as this was an audit using a questionnaire that collected descriptive data only.
Results
Patients
A total of 51 MPN patients and 44 caregivers completed the questionnaires. The majority of patients and caregivers were female (67% and 55%, respectively) with a mean age of 57 and 49 years, respectively. The mean age of MPN patients at diagnosis was 52 years (18-78). Most patients had been living with MPN for more than 2 years (68%), with 47% living with the disease for more than 4 years (since diagnosis). Most caregivers reported providing care for more than 2 years (56%), with 36% providing care for more than 4 years. Seventy per cent of patients described their current health state as ‘excellent’ to ‘good’, while 29% described their current health state as ‘fair’ to ‘poor’. Respondent characteristics are presented in Table 1.
Table 1. Respondent characteristics
| Characteristic | Patient | Caregiver |
|---|---|---|
| Age, mean (range), years | ||
| At time of questionnaire completion | 57 (38–80) | 49 (19–77) |
| At time of diagnosis | 52 (18–78) | NA |
| Disease duration (years since diagnosis), n (%) | ||
| >4 | 24 (47) | NA |
| 2 to 4 | 11 (21) | NA |
| 1 to 2 | 6 (12) | NA |
| <1 | 10 (20) | NA |
| Gender n (%) | ||
| Male | 17 (33) | 20 (45) |
| Female | 34 (67) | 24 (55) |
| Current health state, n (%) | ||
| Excellent | 4 (8) | NA |
| Very good | 14 (27) | NA |
| Good | 18 (35) | NA |
| Fair | 13 (25) | NA |
| Poor | 2 (4) | NA |
| Very poor | 0 | NA |
NA=Question was included in the patient questionnaire only.
Symptoms
The most common symptoms experienced by patients at diagnosis were fatigue (71%), pruritus (37%) and dizziness (35%). Symptoms experienced by at least 20% of patients are presented in Figure 1. Other symptoms reported in less than 20% of patients included sexual problems (18%), abdominal pain (14%), blood clots (14%), early satiety (10%) and unintentional weight loss (10%). Four per cent of patients did not experience any symptoms at diagnosis. Half of the patients had experienced symptoms for more than 2 years prior to diagnosis.
Figure 1. Symptoms experienced by ≥20% of patients at diagnosis or questionnaire completion
The most common symptoms experienced by patients at the time of questionnaire completion were fatigue (86%), bone pain (43%) and pruritus (37%). Symptoms experienced by at least 20% of patients are presented in Figure 1. Other symptoms reported in less than 20% of patients included cough (18%), abdominal pain (16%), burning in the hands and feet (16%), early satiety (14%) and sexual problems (10%). Four per cent of patients did not experience any symptoms at the time of questionnaire completion.
When asked which symptoms they would most like to resolve, 65% named fatigue. Pruritus (20%), bone pain (18%), problems concentrating, difficulty sleeping and facial flushing (all 12%) were also named.
Emotional impact of MPN
The majority of patients (81%) described feeling fear/distress at the time of diagnosis, 12% reported feeling depressed, while 30% experienced a sense of calm or relief and 31% were not sure how they felt or could not remember. The most common emotions experienced by caregivers at the time of diagnosis were concern/worry (both 59%), scared feelings (43%) and anxiety (30%) (Figures 2a and 2b).
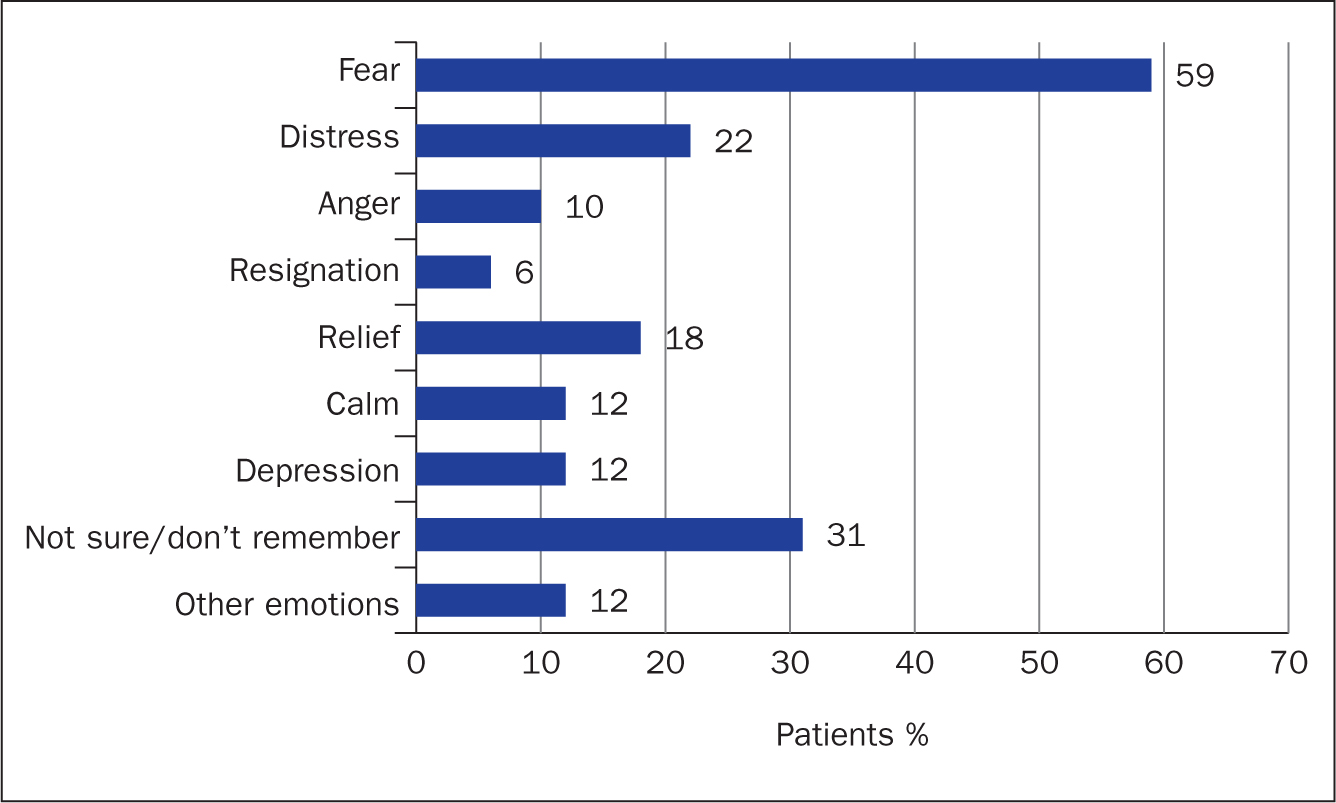 Figure 2a. Primary emotions experienced by patients at diagnosis
Figure 2a. Primary emotions experienced by patients at diagnosis 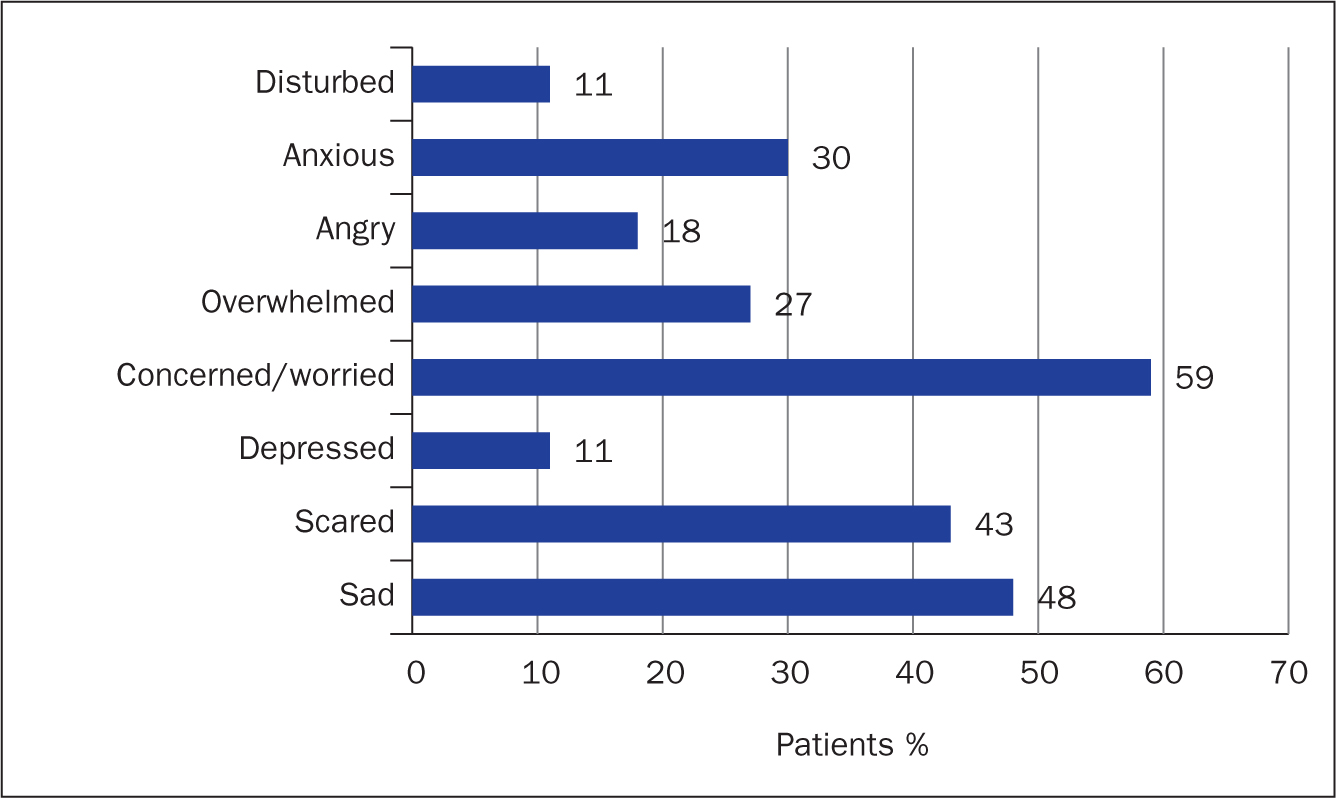 Figure 2b. Primary emotions experienced by caregivers at diagnosis
Figure 2b. Primary emotions experienced by caregivers at diagnosis
Most patients (67%) felt that MPN had a ‘minor’ to ‘no impact’ on their emotional wellbeing (defined as stress and anxiety levels and mood), whereas 32% reported a ‘great deal’ or a ‘significant’ impact. Similarly, although 61% of caregivers reported that caring for a person with MPN made ‘minor’ to ‘no difference’ to their emotional wellbeing, 35% reported a ‘significant’ or a great deal of impact (Table 2). When caregivers were asked how they felt about the future of the person with an MPN, ‘concerned’, ‘hopeful’ and ‘worried’ were the most common answers, reported by 48%, 43% and 39% respectively. Most patients (68%) reported that the disease was not controlling their lives, 69% felt that they had a normal life, with 39% forgetting that they have a disease ‘often’ or ‘all the time’. Although 74% ‘never’ or ‘rarely’ felt depressed about their disease, almost half (46%) reported feeling anxious or worried about their condition ‘often’ or ‘all the time’.
Table 2. Impact of MPNs on patient and caregiver emotional wellbeing
| Impact on emotional wellbeing | Patients n (%) | Caregivers n (%) |
|---|---|---|
| Not at all | 4 (8) | 3 (7) |
| Very little | 8 (16) | 9 (20) |
| Minor impact | 22 (43) | 15 (34) |
| Significant | 11 (22) | 13 (30) |
| A great deal | 5 (10) | 2 (5) |
Daily activities
MPN impacted on energy levels and sleep ‘all the time’ or ‘often’ in 69% and 37% of respondents respectively, with ability to exercise impacted in 53%. Sexual, social and professional lives and ability to care for family were also affected (Figure 3). At the time of questionnaire completion, 98% of patients were actively receiving treatment. Of these, 51% reported that the treatment had a positive impact on their lives, while 36% felt that it either had ‘no impact’ or a ‘negative impact’.
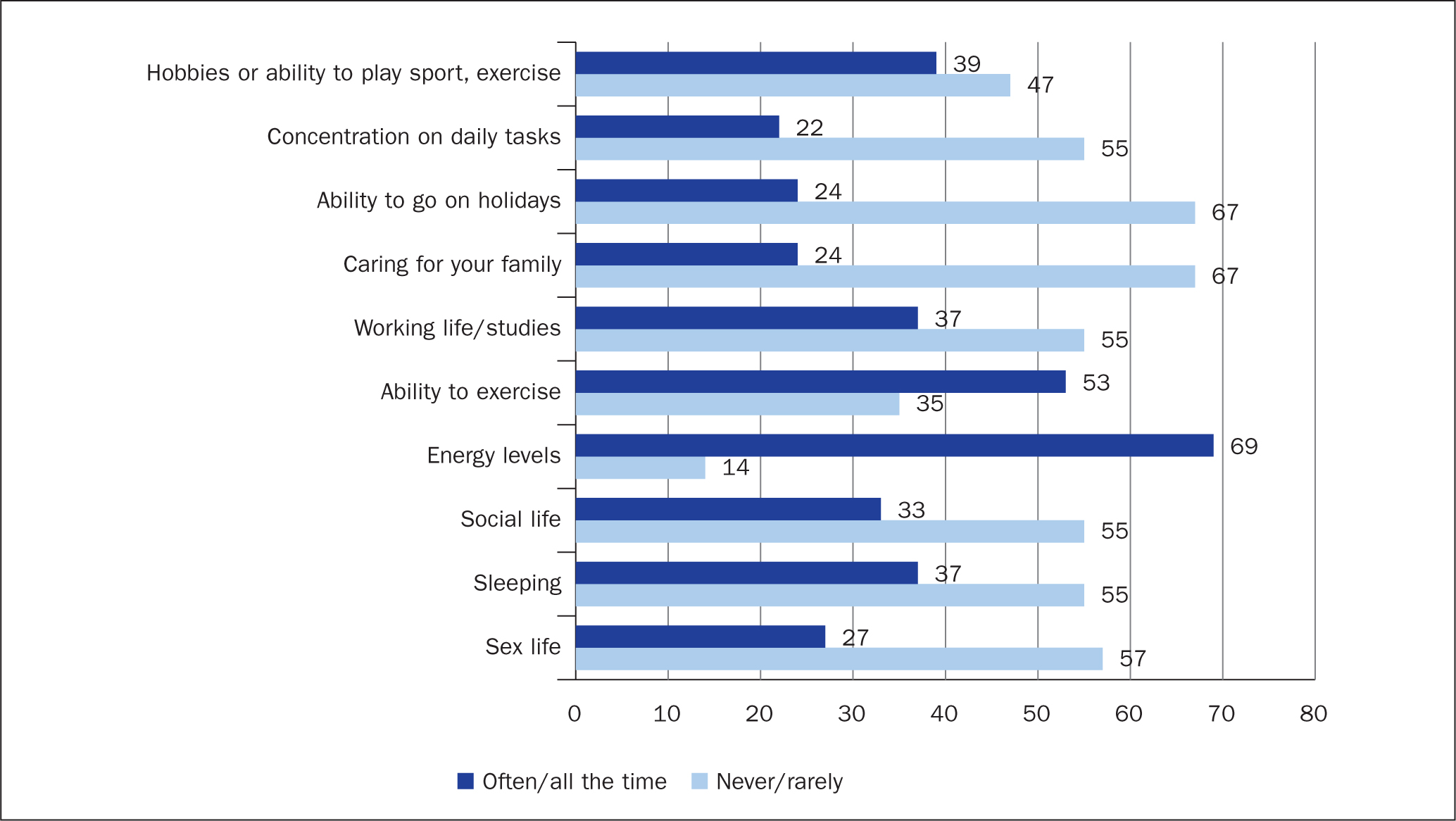 Figure 3. Disease impact ratings on patients' daily lives. Patients were asked how often their MPN impacts each activity
Figure 3. Disease impact ratings on patients' daily lives. Patients were asked how often their MPN impacts each activity
Diagnosis
Following diagnosis, the majority of patients received support from family (75%) and health professionals (67%), with 10% stating that they had no support (Figure 4). Most (71%) felt that additional support at the time of diagnosis could have helped them better deal with their condition; more educational, emotional and peer group support were named by 50%, 37% and 35% of patients, respectively. Health professionals (doctor/nurse) (65%), patient support groups (33%), family (22%), other patients (10%) and friends (6%) were cited as the desired source of this additional support.
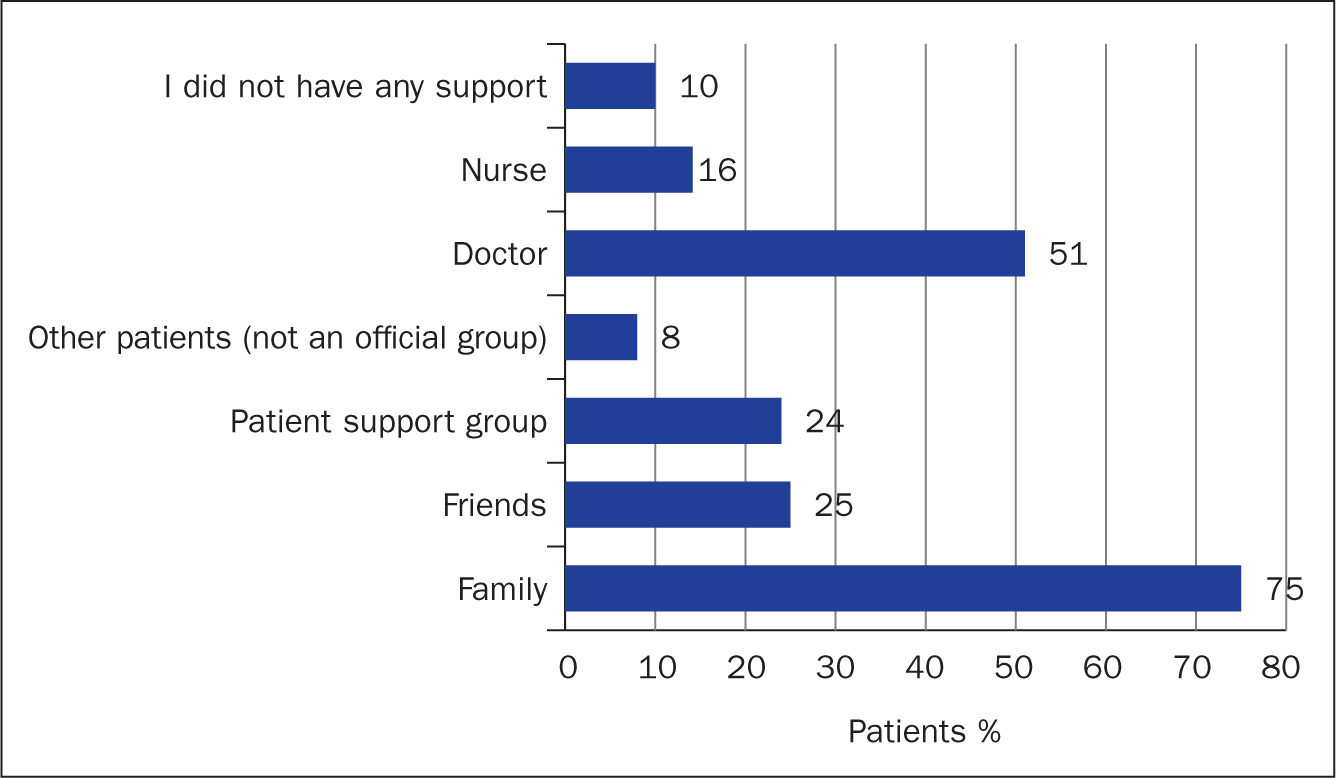 Figure 4. Sources of patient support following diagnosis
Figure 4. Sources of patient support following diagnosis
At the time of diagnosis, 69% of patients were given information (leaflets, links to websites etc) to explain their condition and the potential symptoms. Although 47% stated that their health professional provided them with a leaflet and explained the contents, 12% were provided with a leaflet with no explanation. In 46% of cases health professionals directed patients to a website or brought up a website during the consultation. Roughly a quarter of patients said that their health professional told them about patient support groups. Information on MPNs was provided to 54% of caregivers at the time of diagnosis. Awareness of the disease was low prior to diagnosis; with 96% of patients and 100% of caregivers having never heard of MPNs.
Ongoing support
Ongoing support was received from spouses/partners (71%), siblings, children, parents and others. Caregiving was not required by 14% of patients and 6% said that no caregivers were available (Figure 5a). Caregivers provided support primarily to their spouses (61%) and parents (27%), with others supported their children, siblings and other relatives (Figure 5b). Emotional support and companionship were the most needed support types. Other forms of support included transportation, financial, home making etc (Table 3). While 68% of caregivers felt that they spend less than an hour a day providing care, 9% spend at least 4 hours.
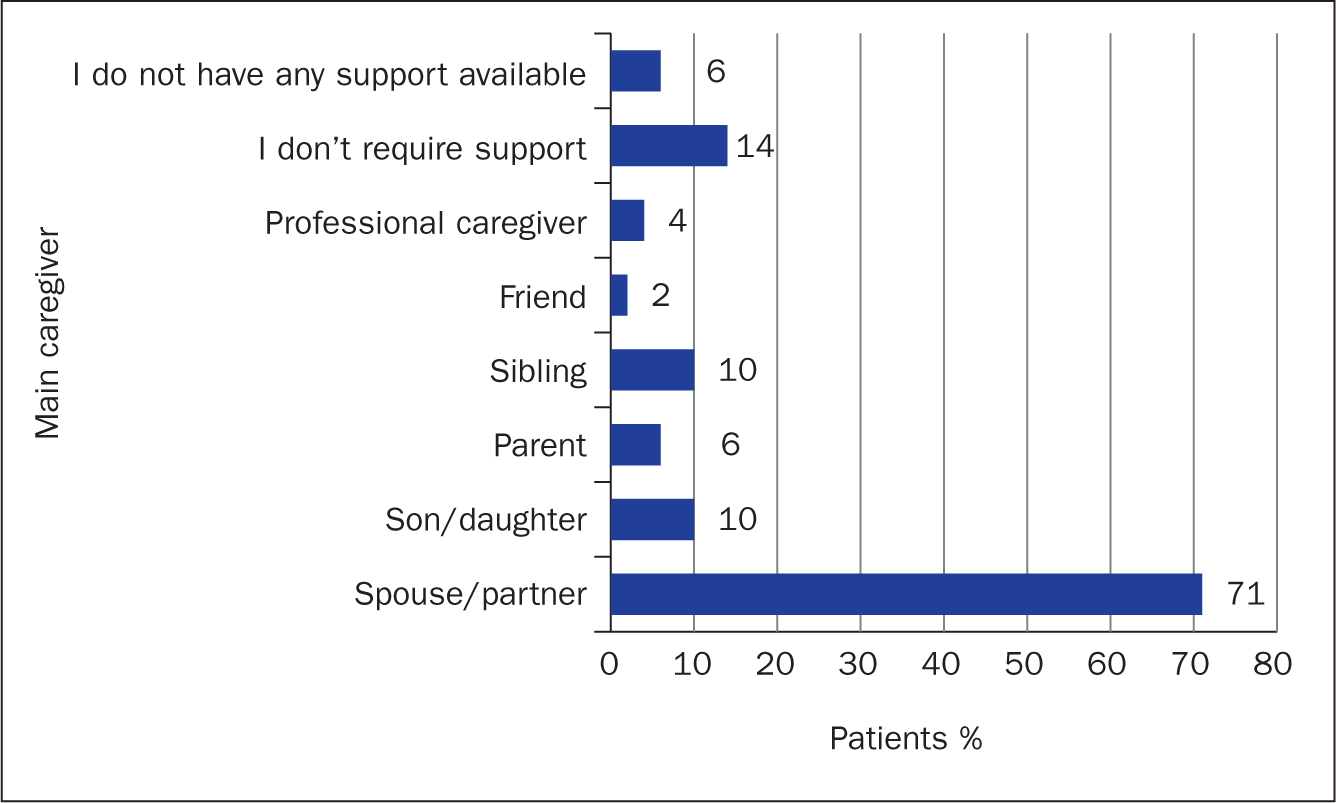 Figure 5a. Main caregiver supporting patients at time of questionnaire completion
Figure 5a. Main caregiver supporting patients at time of questionnaire completion 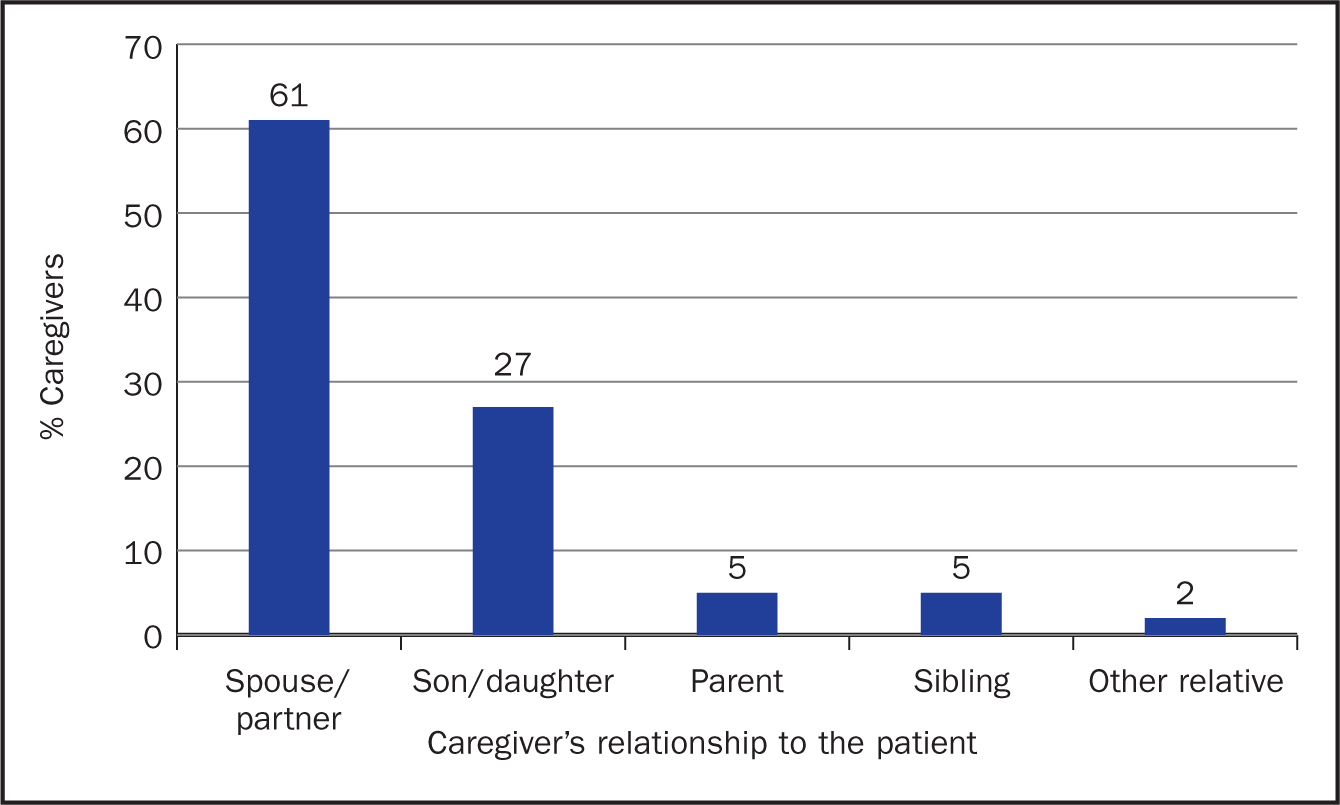 Figure 5b. Caregiver's relationship to the patient. Caregivers were asked to complete the statement ‘I am the … to the patient’
Figure 5b. Caregiver's relationship to the patient. Caregivers were asked to complete the statement ‘I am the … to the patient’
Table 3. Type of help required/provided by MPN patients/caregivers
| Support type | Patients n (%) | Caregivers n (%) |
|---|---|---|
| Companionship | 32 (63) | 36 (86) |
| Emotional support | 35 (69) | 41 (93) |
| Transportation | 11 (22) | 14 (32) |
| Homemaking | 15 (29) | 10 (23) |
| Healthcare assistance | 4 (8) | 3 (7) |
| Managing finances | 9 (18) | 7 (16) |
| Organising daily activities | 5 (10) | 7 (16) |
| No help/support required | 12 (24) | NA |
| No help/support available | 2 (4) | NA |
| Other | NA | 1 (2) |
The majority of patients felt well informed about their disease (82%), supported by their doctor/nurse (74%) and felt that their doctor understands their situation (65%) (Table 4). Similarly, most caregivers agreed (somewhat or strongly) that they were well informed about the disease (66%) and supported as caregivers (57%). However, 45% of caregivers did not feel included/taken into consideration by the doctors/nurses.
Table 4. Patient statements about information and support
| Patient statements | Strongly agree (% patients) | Somewhat agree (% patients) | Somewhat disagree (% patients) | Strongly disagree (% patients) |
|---|---|---|---|---|
| I am well informed about my disease | 35 | 47 | 4 | 4 |
| I feel supported by my doctor/nurse | 49 | 25 | 16 | 8 |
| My doctor understands my situation | 45 | 20 | 20 | 6 |
The majority of patients (94%) did not have local patient support groups available to them; similarly, 82% of caregivers were not in contact with a caregiver MPN support group. Both patients and carers stated that there is a need for local MPN support groups to be established (98% and 84% respectively). Additionally, 93% of caregivers believed that more public education on MPNs is needed.
Discussion
The impact of MPNs on patients and caregivers within the Republic of Ireland, has not previously been assessed, to the best of our knowledge. In agreement with other reports (Mesa et al, 2016; Harrison et al, 2017; 2019), the present study's findings suggest that Irish MPN patients experience a broad symptom burden that impacts on emotional wellbeing and daily functioning. The present study also suggests that the impact of MPNs extends beyond the patient and that there is a need for more support for both patients and caregivers at the time of diagnosis and beyond.
Most respondents (almost 80%) had symptoms at diagnosis. Fatigue was the most common symptom and was reported in 70% of patients, which is in keeping with previously reported studies (Scherber et al, 2016; Harrison et al, 2017; 2019). At the time of questionnaire completion, rates of fatigue had risen to 86%, with ability to exercise and energy levels impacted ‘all the time’ or ‘often’ in 53% and 69% of patients (respectively). Fatigue is widely recognised as a significant burden for MPN patients (Scherber et al, 2016) and is a major contributor to reduced QoL (Mesa et al, 2007). Although the aetiology of MPN-related fatigue is multifactorial, studies have shown that underlying psychological comorbidities may contribute (Scherber et al, 2016). In fact, some authors suggest the magnitude of the association to be the highest among all the correlates of fatigue (Hotopf, 2014). Results of an international survey of MPN patients (n=1788), showed that patients with underlying depression, higher body mass index and current alcohol or tobacco use demonstrated significantly higher fatigue scores. The authors suggest that these represent under-recognised modifiable therapeutic targets to reduce fatigue (Scherber et al, 2016).
Depression was reported in 12% of the present study's respondents at diagnosis and had increased to 20% at the time of questionnaire completion, despite high treatment levels of 98%. A further third reported a great or significant impact on their emotional wellbeing, and almost half felt anxious or worried about their condition ‘often’ or ‘all the time’. High emotional burden was also noted among caregivers, with a third stating that caring for a person with MPN had a ‘great deal’ or ‘significant’ impact on their emotional wellbeing. Half of the patients reported that they could have benefited from more educational support at diagnosis, 65% would have liked to receive this from their health professionals. Taken together, these data suggest that there is a need to develop strategies for proactive symptom management, incorporating self-care strategies and modifiable lifestyle changes for reducing physical and psychological symptoms.
In addition to its potential benefit to patients, educational support has been reported to be one of the most impactful interventions in reducing caregiver strain and burden (Honea et al, 2008). The present study's findings reveal that 80% of patients received caregiver support, which is higher than previously reported (Harrison et al, 2017; Paranagama et al, 2018). Data from the Global MPN Landmark survey show that the need for assistance is significantly higher in patients with MF (compared to ET/PV), high or intermediate risk disease and greater symptom burden (Harrison et al, 2017). Other studies have also shown the relationship between disease severity and care dependency (Janssen et al, 2011, 2013; Montgomery et al, 2018), suggesting that symptom-reducing interventions may reduce the need for care and the associated burden on caregivers. Furthermore, the negative impact of MPN on social and sexual functioning and the reported reduction in ability to care for family suggests that the impact of MPN extends beyond the patient and caregiver.
At the time of questionnaire completion, most patients and caregivers felt well informed about MPNs. However, other needs remained; 94% of patients were without local support groups, with 84% of patients and caregivers confirming the need for such support. Almost all patients and caregivers felt that more public education was needed. Most patients and caregivers had not heard about MPN prior to diagnosis (96% and 100% respectively), demonstrating the lack of public awareness of MPN. Half of the patients experienced MPN-related symptoms for over 2 years before diagnosis, which has been previously reported (Mesa et al, 2016). The present study did not explore whether patients discussed symptoms with their GP in the years prior to diagnosis. Therefore, whether the delay to diagnosis could be partially due to a lack of public or GP awareness of MPN is unclear and warrants further investigation.
Limitations
The limitations of the analysis include the descriptive nature of the findings, self-reporting of clinical information, small patient numbers and the recruitment method. The questionnaire was designed to be descriptive, which precluded any statistical comparison of the data. In addition, the recruitment procedure may have introduced bias as only patients attending the MPN patient forum could participate. These patients may have been more engaged or had a lower symptom burden. The patient number is small in this questionnaire, reflecting a limitation of the recruitment method and the low/unknown prevalence of MPN in the Republic of Ireland. Additional limitations are that the questionnaire did not categorise the data based on MPN subtype; the symptom burden is known to be much higher in MF compared with ET and PV and this could have impacted the results. Finally, the positive and negative questionnaire descriptors were not always evenly balanced or interspersed, which may have introduced an element of bias to some questions.
Conclusion
This project was the first of its kind to examine the impact of MPNs on patients and caregivers in the Republic of Ireland. As expected, the findings showed that, despite treatment, symptom burden remains high and impacts the emotional wellbeing of patients and carers alike. The findings suggest the need for support is highest around the time of diagnosis. Further research will determine whether educational programmes that focus on modifiable lifestyle factors, symptom reduction and self-care could be used to reduce patient distress and anxiety around the time of diagnosis and to improve patient and caregiver QoL in the longer term. Additionally, the creation of a wider emotional support network (including the establishment of local support groups) is needed to help patients adjust to their diagnosis and to reduce the burden on caregivers and health professionals. The survey also suggests that work is required to establish the prevalence of MPNs in the Republic of Ireland and to increase public awareness. In the absence of a Republic of Ireland-specific database, participation in registries, such as the Cancer Experience Registry (https://www.cancerexperienceregistry.org/), may be a method whereby symptoms and unmet needs could be captured and communicated to a broader audience, including the public and GPs.
KEY POINTS
- Despite high treatment levels, symptom burden associated with myeloproliferative neoplasms (MPNs) remains high and impacts the emotional wellbeing of patients and carers alike
- There is a need for greater patient and caregiver support at the time of diagnosis
- Educational support and interventions that incorporate self-care and modifiable lifestyle factors may be effective in meeting this need and helping to manage symptom burden
- Awareness of MPNs pre-diagnosis was reported as low, which may reflect the lack of awareness in the Irish general public
- There is a strong need for the establishment of local MPN patient and caregiver support groups
CPD reflective questions
- In this questionnaire, many patients experienced symptoms for more than 2 years before diagnosis. Is this timeframe acceptable and what could be done to lower it?
- The questionnaire revealed that the prevalence of many symptoms differed between diagnosis and questionnaire completion. What factors may have contributed to this?
- Could nurse-led education be used to help patients manage physical and psychological symptoms? How and when would this be delivered for optimal impact?
- Studies have suggested that physical and psychological comorbidities may contribute to symptom burden. What level of pre-screening for medical and psychological conditions do you think is appropriate/feasible in both clinical and research settings?
- The percentage of patients requiring caregiver support was higher in this questionnaire compared with previously reported studies. Why do you think this is?


