The UK is currently experiencing a nationwide shortage of nurses with around 40 000 nursing vacancies across health and social care in England in 2020 (House of Commons, 2020). The number of unfulfilled staff vacancies in adult social care has steadily been rising since 2014 (Care Quality Commission (CQC), 2019). A shortage of registered nurses (RNs) in nursing homes is having far-reaching effects (Mitchell, 2021). Without adequate RN cover, nursing homes are either forced to close or re-register as residential homes. This has a huge knock-on impact on the number of services that can be offered in particular regions, meaning people who cannot access services locally are forced to be separated from their families. Closures and re-registration also increase pressure on NHS services that must make up for the mismatch between service provision and need (CQC, 2019).
The Registered Homes Act 1984 stipulates that nursing homes, registered under part 2, must be under the charge of a medical practitioner or qualified nurse on duty within the home. Currently the wording of this legislation is interpreted by care providers, regulatory bodies and local authorities as meaning that nursing homes must have the physical presence of a registered nurse on duty within the home at all times. This requirement, in the face of today's nursing shortages, has created an unprecedented market for agency staff.
Few studies examining the use of agency staff in nursing homes exist. However, studies conducted in the USA have found agency staffing levels above 25 full-time equivalent (FTE) staff per 100 beds were associated with poor quality of care (Castle and Enberg, 2007). Further evidence suggests that there is a strong association between better quality care and lower use of agency RNs and this influence is likely to be clinically significant (Castle, 2009). This is now the focus of an ongoing programme of work, funded by the National Institute for Health and Care Research (NIHR), which aims to map the relationship between workforce characteristics and care quality outcomes in the UK in order to understand the most effective workforce models of nursing and care support in care homes (Spilsbury et al, 2019).
Use of high numbers of agency staff is also likely to adversely impact infection control. In fact, one of the common factors prevalent in UK care homes experiencing severe COVID-19 outbreaks was the number of staff who worked on multiple sites. The Department of Health and Social Care (DHSC) published a proposal to regulate and stop the movement of staff between care settings to minimise the spread of COVID-19 (DHSC, 2021). However, this issue is pertinent beyond the pandemic; in 2017 Public Health England (PHE) urged care providers to ‘avoid moving staff between homes and floors’ to prevent the spread of flu (PHE, 2017).
High reliance on agency nursing can also impair continuity of care (National Quality Board, 2013). Indeed, agency staff do not have the opportunity to create and sustain relationships with staff, residents or families, consequently being less able to spot when the health of a resident declines. As well as a lack of continuity of care, other staff members may feel vulnerable or are relied upon unfairly when agency staff are leading a shift. This impact on quality of care is compounded by the increased cost (National Quality Board, 2013), which is passed on to both local authority and service users. For Cornwall Care, agency staff rates are increasing exponentially and some shifts cost more than the fees for a resident for a whole week, funds that could arguably be reinvested into care delivery, including better pay and pensions for nursing staff.
CQC inspections continually highlight that homes rely too much on agency staff, and that this is often a characteristic of poorly performing services (CQC, 2019). However, the social care sector, which mainly consists of independent providers, has little influence on the number of nurses being trained or strategies for ensuring there are enough nurses in social care to deliver the required services. Indeed, workforce planning and recruitment typically focus on nursing careers within the NHS and adult social care must compete with the NHS for a limited number of registered nurses (Lloyd, 2001). The integrated care systems (ICS) partnerships, introduced in 2022, which bring together providers and commissioners of NHS services with local authorities to plan health and care services, may help to overcome this issue. However, a lack of workforce was still the leading obstacle to ICS progress in a 2022 report (Pett and Bliss, 2022). In addition, lack of career progression within adult social care may also contribute to poor uptake and retention of staff. A recent survey showed that 37% of social care employees were looking to leave the sector within 5 years, 41% were searching for greater career progression and 40% wanted more training and development opportunities (Ford, 2019).
A 2001 article suggested that the legislation within the Registered Homes Act 1984 is in urgent need of updating to help reduce the impact of inappropriate placements within homes (Lloyd, 2001). However, until now, ‘appropriate access’ to nursing has been ill defined. With the shortage of registered nurses increasing, what defines appropriate access to nursing care within nursing homes and how can we transform service delivery to help combat the current staffing crisis? The aim of this article is to offer the authors' initial ideas for the transformation of nursing home care and open a discussion and debate on nursing provision within nursing homes. The authors believe that the risks inherent with progression and innovation are far outweighed by the catastrophic impact our current ways of working have, not only for social care, but also for wider healthcare systems.
Possible solutions
One option the authors suggest for consideration is that nursing homes do not always require the physical presence of a nurse, but rather, ‘appropriate access to nursing’ could be provided digitally, via remote means, creating an e-nursing model (see Figure 1). Adapting the nursing profession for a digital future is of key importance, including the development of virtual care modalities that draw from experiences with telehealth and remote models of care (Booth et al, 2021). The COVID-19 pandemic has highlighted how many healthcare services previously delivered face to face could just as adequately be delivered remotely (Doraiswamy et al, 2020; Howarth et al, 2021) and there is ongoing work in nurse-led digital health improvement projects, outside of social care, including nurse-led video consultation clinics (Burdett Trust for Nursing, 2021).
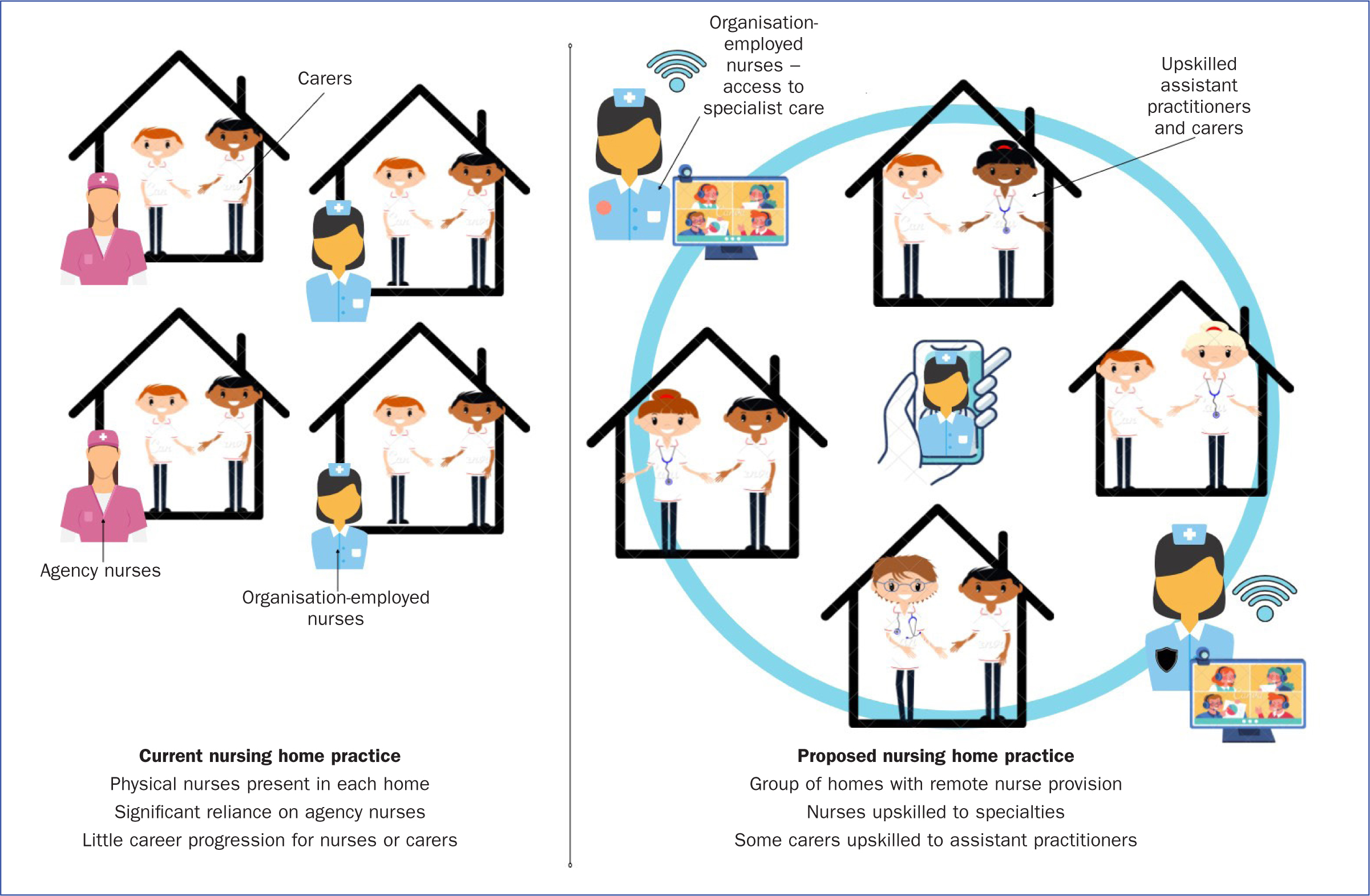
Therefore, perhaps nursing homes could adopt a system where care staff are provided with education and training to increase their skills and competence – ‘upskilled’ – in order to cover nursing home care and nurses are relieved from their required 24/7 presence and enabled to cover a group of nursing homes simultaneously, using a virtual ward methodology. In this way, the organisation Cornwall Care is collaborating with local education providers to deliver training to current care workers to become assistant practitioners, a recognised healthcare profession, via a 2-year, level 5 course resulting in an accredited diploma. The course will provide the level of skills required for care staff to run shifts within nursing homes under the supervision of a registered practitioner, and to assess, plan and deliver care, provide medications and engage with wider health teams. Such tasks are traditionally provided by nurses; however, in community-based care family members are regularly trained in care provision for ill relatives, including tasks such as providing medication, therapies, changing stoma bags and aiding with dialysis machines.
During care at home and end-of-life care, many care needs are met by family members (Caswell et al, 2019), with the care provided being professionally supported, but without those professionals being physically present at all times. In such cases, nurses visit as and when required. The upskilled assistant practitioners could then lead shifts within nursing homes, freeing up nurses to develop specialist skills and provide support across a group of nursing homes, rather than physically being located in one nursing home for the duration of their shift. The nurses may develop specialist skills in areas such as infection control, tissue viability, dementia, prescribing, speech and language or other required services. This would allow nurses to provide their specialist input to the group of homes as required, either remotely or in person when needed. A digital platform could be available for staff in nursing homes, either through local care chains or geographical districts, to show staff which nurses were on duty remotely and which nurses were available with which specialist skills.
One implication could be enhanced care for residents, who often experience complex illnesses and multimorbidities, thus a range of specialist nurses would be advantageous, as continuity of care and an appropriate skill mix are essential in facing the challenges of multimorbidity nursing (O'Connor et al, 2018). This approach would likely also reduce waiting times for such specialist services from local health providers, and reduce the burden placed on resources by nursing homes. Nursing homes frequently access NHS resources, requiring input from a broad range of disciplines (Gordon et al, 2014), which could thus be reduced through provision of directly employed specialty nurses. Reducing strain on the NHS where possible is increasingly important due to the ageing population and growing burden of disability (Guzman-Castillo et al, 2017). The UK government has suggested technology may indeed have a role to play in supporting the needs of the ageing population (Government Office for Science, 2016). Digital nurse provision is one such option.
From the staffing perspective, the proposed move to upskilled assistant practitioners and digital specialist nurse provision could also enhance the appeal and retention of both care workers and nurses in the social care sector (rather than agency or NHS roles), through providing both care staff and nurses with the opportunity for career progression. The reduction in reliance on agency staffing also has significant potential implications for clinical care (Castle, 2009) and social care budgets. Additionally, a reduction in use of agency staff may also help reduce continued viral transmission of COVID-19, or any future such issues, between residential care homes (DHSC, 2021). Finally, considering the high economic cost of agency staffing for nursing homes, reduced reliance on agencies would create large financial savings within social care, which may allow for enhanced pay for permanent staffing or more appropriate use of funds. Ultimately, the proposed innovation in service delivery for nursing homes could have significant implications for resident care, safety and continuity, further to staff retention, intake, satisfaction and more appropriate allocation of budget.
This proposed transformation may also enable those with disabilities to re-enter the workforce and/or work in roles that may better suit their needs. With a limited number of nurses and issues in retention, actively recruiting to roles that better accommodate people with disabilities may go some way to help mitigate these challenges.
Possible barriers to implementation
Implementing the suggested change is not without barriers however (Table 1). Risk is a central component of innovation (Brown, 2010). Generally, risk aversion within health and care can be a barrier to innovation (Brown, 2010). However, the risk of carrying on with current practice should also be considered and weighed against the risks of innovation. When service delivery is ineffective and inefficient, the risk of avoiding innovation is that performance remains problematic (Brown, 2010). As we know, remote health care and video consultations had been of interest in the health sector for some time but progress in adoption had been slow before the COVID-19 pandemic (Shaw, 2020), and yet, during the pandemic the vast majority of healthcare service delivery became remote and video consultations were rapidly implemented (Doraiswamy et al, 2020). One study in UK primary care demonstrated that 90% of GP consultations were remote during April 2020, while face-to-face consultations had been standard practice formerly (Murphy et al, 2021). The authors also noted higher levels of video consultation use among older patients (>85 years) as GPs were being remotely connected to older adults in nursing homes (Murphy et al, 2021). The risks of ‘service as usual’ should be weighed against the risks of innovation in care delivery for social care. Other challenges will include upskilling care staff with the necessary IT skills to competently use the proposed technology.
Table 1. Proposed benefits (regular type) and challenges (bold type) of current practice and proposed transformation
| Current practice | Proposed transformation |
|---|---|
| Registered nurse always in each nursing home | Organisation-employed nurses oversee all nursing homes remotely |
| Constrained by current interpretation of legislation | Remote nurses can also oversee community, which helps people remain at home longer |
| High use of agency nurses | Reduced reliance on agency nurses |
| Lack of continuity of care through agency staffing | Improved continuity of care |
| Significant financial impact of agency staffing | Financial savings |
| Infection risk with agency staff shared across multiple homes | Lessened risk of viral spread between homes |
| Lack of career progression for carers and nurses | Career progression for nurses (to specialise) and carers (to become assistant practitioners) |
| Limited accessibility to nursing for those with disabilities | Enhanced accessibility of the nursing role |
| Poor recruitment and retention of care and nursing staff | Potential to enhance staff retention |
| Reliance on local health care for specialty services | Risks of innovation and challenges with digital provision |
| Nursing homes re-registering as care homes due to nursing shortages | Cultural shifts for social care providers, nurses, residents and family |
Next steps
The authors strongly believe the suggested approach of upskilling care staff and providing digital nursing across nursing homes deserves further consideration, including active debate on a national scale, implementation and trialling for assessment of: impact, safety, care quality and cost-benefit analysis. The financial savings on reduction of agency nurses may even allow for pay increases for contracted staff, again potentially improving retention. At present, the authors have formed a working group of stakeholders, and have met with local council representatives, researchers, nursing standards professionals, the CQC and national care standards professionals and are planning further meetings with families and residents.
The authors would welcome contact and wider input into challenging the interpretation of nursing home regulations that is contributing to an unmeetable demand on nurses in the social care sector, resulting in avoidable costs and, most importantly, impaired care for older adults. To this end, the corresponding author (katie.edwards@plymouth.ac.uk) welcomes contact to discuss the proposal further and engage in constructive conversation responding to the identified challenge facing nursing homes.
KEY POINTS
- Increasing shortages of registered nurses are contributing to a nationwide staffing crisis in adult social care, creating reliance on agency staff, a practice impacting service cost and continuity of care
- Current interpretation of legislation means nursing homes must have the physical presence of a registered nurse on duty at all times but, until now, ‘appropriate access to nursing’ has been ill-defined
- An alternative model of care delivery could be provided where ‘appropriate access to nursing’ is provided digitally, under a clear protocol, where existing care staff are upskilled in order to cover nursing home care and nurses cover a group of nursing homes simultaneously through digital means
- Anticipated benefits include the ability for nurses to develop and deliver specialist care, increased accessibility of the nursing role, opportunity to upskill existing care staff, improve infection control, and improve continuity of care for residents
- Key challenges include the current interpretation of legislation and the cultural shift required by social care providers, nurses, residents and families. However, the risks of service as usual should be weighed against the risks of innovation
CPD reflective questions
- How can we respond to the current staffing crisis without compromising quality of care?
- Is the current interpretation of the legislation related to nursing provision in nursing homes stifling innovation in service provision?
- What will be the key challenges to implementing the suggested solution of digital nursing provision in nursing homes for different stakeholder groups (such as families, residents, staff, care providers and regulatory bodies)?


