More than one in three people aged over 65 years (around 3.4 million people) fall in the UK every year (Age UK, 2010). As a result, hip fracture is associated with a total cost to health and social services of over £1 billion per year. This one injury carries a total cost equivalent to approximately 1% of the whole NHS budget (Royal College of Physicians, 2019). Hospitals are a high-risk environment for falls. Patients may be disorientated, unwell or navigating unfamiliar environments. The conditions in hospitals such as hard flooring can also increase the risk of serious injury (Lamb, 2015).
Due to the general ill health of patients in a hospital setting, falls can often lead to further complications such as fractures, lacerations or significant internal bleeding (Gu et al, 2016). These incidents therefore increase the overall use of resources in the hospital setting, drive up costs and adversely affect patient outcomes (Quigley et al, 2009). It is estimated that the average increase in the length of stay for a patient who has had a fall is around 12.3 days, which can lead to an average cost increase of 61% (Spetz et al, 2007). Due to the rapidly ageing population in most developed countries, this issue is expected to increase in the future.
Preventing falls, therefore, represents an important part of hospital care that needs to be addressed in order deliver high-quality and cost-effective care (Gu et al, 2016). Nurses, due to their close interactions with patients, are one of the key components in preventing patient falls. Often, nursing staff are more attuned to the risk profile of an individual patient than other staff and represent the front line of defence against falls (Melnyk and Fineout-Overholt, 2011).
Background
Within a large hospital trust in the UK, the number of falls within one particular division were studied to determine the number of falls reported while patients were under ‘one-to-one’ (1:1) or ‘cohorting’ supervision, collectively referred to as ‘enhanced supervision’. It is important that falls are reported to ensure learning and transparency (Cotterill et al, 2018). One-to-one supervision is a type of care provided to ensure the safety of patients who may be suffering from cognitive impairment, exhibit challenging behaviour, or who may be at risk of falls or of causing harm to themselves or others (Wood et al, 2018). One-to-one supervision implies that a specific staff member is tasked with monitoring the activity of a specific patient. ‘Cohorting’ or cohort supervision would indicate one staff member is supervising a group of patients, for example, it may involve the staff member watching the activity of a bay of patients who may be at increased risk of falls. Nursing assistants and registered nurses are the staff members most commonly responsible for undertaking this duty (Wood, et al, 2018).
The National Institute for Health and Care Excellence (NICE)(2013) guideline recommends that for patients at risk of falling in hospital staff should consider a multifactorial assessment and multifactorial intervention. These should identify individual risk factors and any intervention should promptly address the patient's individual risk factors and take into account whether these can be treated, improved or managed during the patient's admission. Patients will be reviewed by physiotherapists or occupational therapists to determine their needs while an inpatient and then on discharge.
Studies have shown that enhanced supervision can have a positive impact on the quality of care in relation to patient outcomes. This can include reducing the risk of agitation (Waszynski et al, 2013), and improving the quality of nursing (Burtson and Vento, 2015). It has also been noted to help improve the rate at which staff responded to patient falls (Jeffers et al, 2013). Other studies, such as Spiva et al's (2012), have argued that there was no impact on the quality of care provided. It is also important to balance this care with the psychological impact on staff wellbeing, because it has been noted that staff providing this type of care can be more prone to physical, verbal or sexual assault (Schoenfisch et al, 2015).
Method
Datix is an electronic incident reporting system (EIRS) used in health services worldwide – over 900 organisation in 19 countries (Maxton et al, 2021). When used, incident reporting systems allow data to be collected and aggregated for the determination of patterns that may lead to corrective action. Reported incidents can also be used as learning tools (Hor et al, 2010), to notice trends and to highlight issues on a large or small scale. When incidents occur staff are encouraged to report them not only to keep a record of the incident, and its potential harm, but also to highlight learning opportunities. The author looked at all falls occurring while a patient was under supervision during 2022. Datix was used to determine any trends in these incidents and to look into the circumstances behind each fall. Data from 2019 to 2022 were also used to determine whether these trends were supported over the long term.
Results
During 2022 it was noted that there were 314 falls reported within the division; of these falls 61 occurred while the patient was under enhanced supervision. This equates to nearly one fifth of all falls (19%). Twenty-three of those incidents took place when the patient was due to be under one-to-one supervision, and 38 of these falls involved patients who were under cohort supervision at the time.
Degree of harm
When incidents are reported, reporters must identify a level of harm caused. In Datix these are categorised as (National Learning and Reporting System, 2019):
- No harm: ‘Any patient safety incident that had the potential to cause harm but was prevented, resulting in no harm to people receiving NHS-funded care. This may be locally termed a “near miss”. Or, any patient safety incident that ran to completion but no harm occurred to people receiving NHS funded care.’
- Low: ‘Any unexpected or unintended incident that required extra observation or minor treatment and caused minimal harm to one or more persons receiving NHS-funded care.’
- Moderate: ‘Any unexpected or unintended incident that resulted in a moderate increase in treatment, possible surgical intervention, cancelling of treatment, or transfer to another area, and which caused significant but not permanent harm, to one or more persons.’
- Severe: ‘Any unexpected or unintended incident that appears to have resulted in permanent harm to one or more persons.’
- Catastrophic: ‘Any unexpected or unintended incident that directly resulted in the death of one or more persons.’
In 2022, it was noted that, of the 23 falls under one-to-one supervision, 2 had resulted in catastrophic harm, 4 in low harm, and 17 in no harm.
Of the 38 falls that occurred under cohorting supervision, 1 resulted in catastrophic harm, 2 in severe harm, 10 in low harm, and 25 in no harm.
In contrast, there were 248 falls where enhanced supervision was not in place, and this resulted in 165 ‘no harm’ incidents, 77 low, 5 moderate and 1 severe incident (Table 1).
Table 1. Incident report data for 2022 – number of falls
| Degree of harm | Falls – No supervision | Falls – 1:1 supervision | Falls – Cohort supervision | Total |
|---|---|---|---|---|
| None | 164 | 17 | 25 | 206 |
| Low | 77 | 4 | 10 | 91 |
| Moderate | 5 | 0 | 0 | 5 |
| Severe | 1 | 0 | 2 | 3 |
| Catastrophic | 1 | 2 | 1 | 4 |
From these results it was noted that those patients under enhanced supervision were most likely to suffer severe or catastrophic harm following a fall. Of the falls in patients not requiring supervision, 1% resulted in severe or catastrophic harm. However, in the group of patients needing cohort supervision this rose to 8%. Of those requiring one-to-one care this number was 9%. It is clear that patients deemed at need of enhanced supervision were most likely to come to worse harm if they fell. This stresses the importance of the role of patient supervisors (Table 2).
Table 2. Incident report data for 2022 – resulting harm from fall by type of supervision assigned
| Degree of harm | Falls – No supervision | Falls – 1:1 supervision | Falls – Cohort supervision |
|---|---|---|---|
| None | 66% | 74% | 66% |
| Low | 31% | 17% | 26% |
| Moderate | 2% | 0% | 0% |
| Severe | <1% | 0% | 5% |
| Catastrophic | <1% | 9% | 3% |
Despite this importance, it can be seen that 14 of the patients involved in the falls were not under the correct level of supervision outlined in their care plan at the time of the fall; 47 were under the care plan level of supervision. Data for 2022 showed that 27 (44%) of the falls were witnessed at the time; however, 34 (56%) were not, despite patients being noted as needing enhanced supervision. When looking at the data from 2019 to 2022 combined, 60% of falls were not witnessed and 40% were. This shows that even though patients are known to be at risk there remain instances when situations lead to patients not receiving the standard of care that is needed. Studies have shown that this is common and up to 80% of falls take place when patients are not observed (Staggs et al, 2014). It is important that, when staff are supervising patients, suitable replacements are arranged before they leave patients unattended. Of the patients who fell, 49 were not known to have previously fallen and 12 were known to have had previous falls (in 6 patients the Datix record had no information on this point).
Footwear
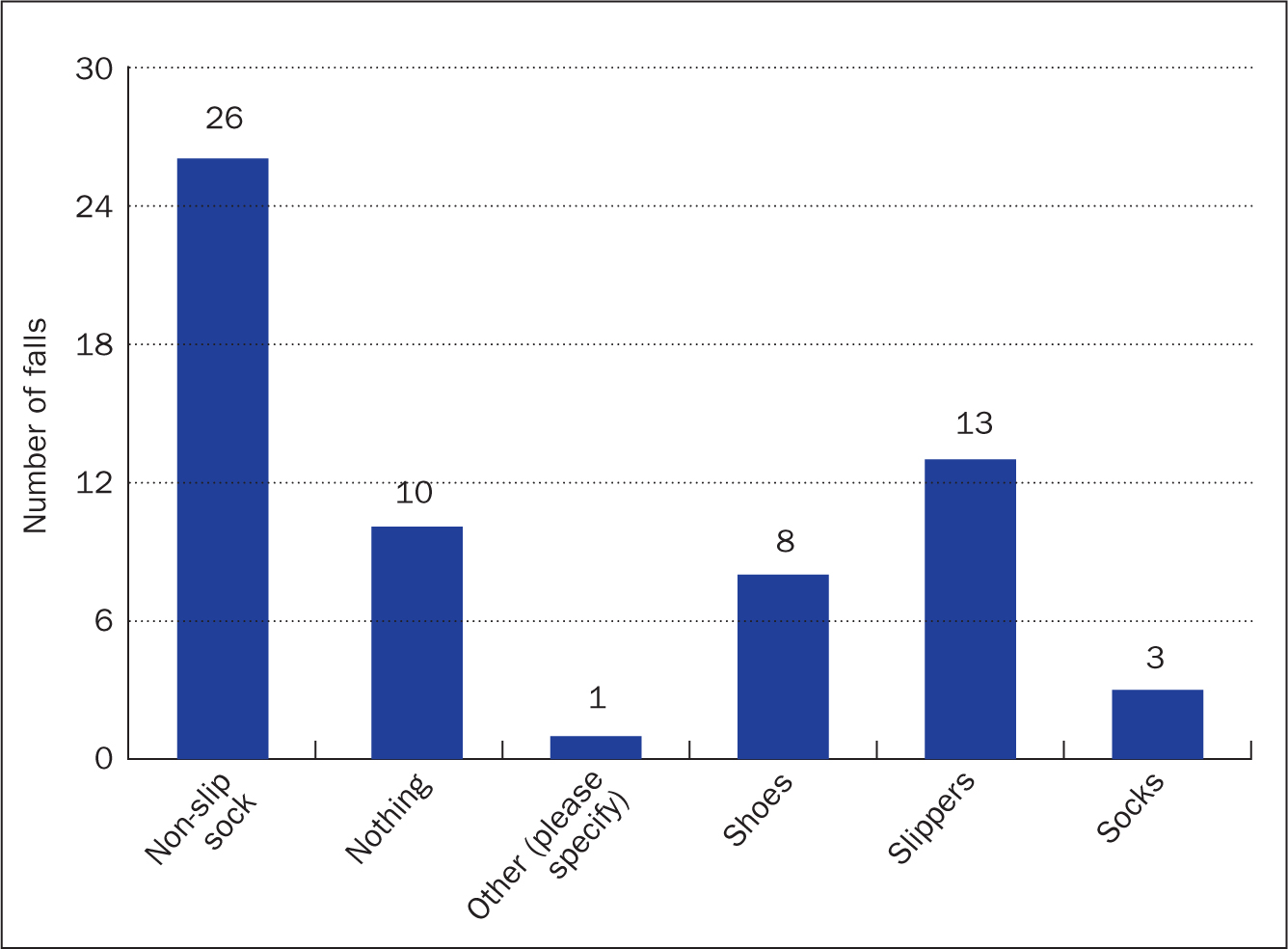
Many patients arrive at hospital without adequate footwear due to the emergency nature of admission. As a result, hospitals use non-slip socks as temporary footwear for older adults. Non-slip socks are regular cotton socks with a rubber tread on the top and bottom to improve the grip strength and slip resistance during ambulation. Although these socks provide some foot protection, they do not possess the properties of adequate footwear to help prevent falls (Hartung and Lalonde, 2017). This is evident in the figures showing that the majority of patients were wearing non-slip socks at the time of their fall (26), while 13 were wearing slippers and 10 of the patients who fell were not wearing any footwear (Figure 1). This figure is similar to the combined 4-year figures from 2019-2022 showing that 48% of patients who fell were wearing non-slip socks and 16% were in slippers.
Location of fall
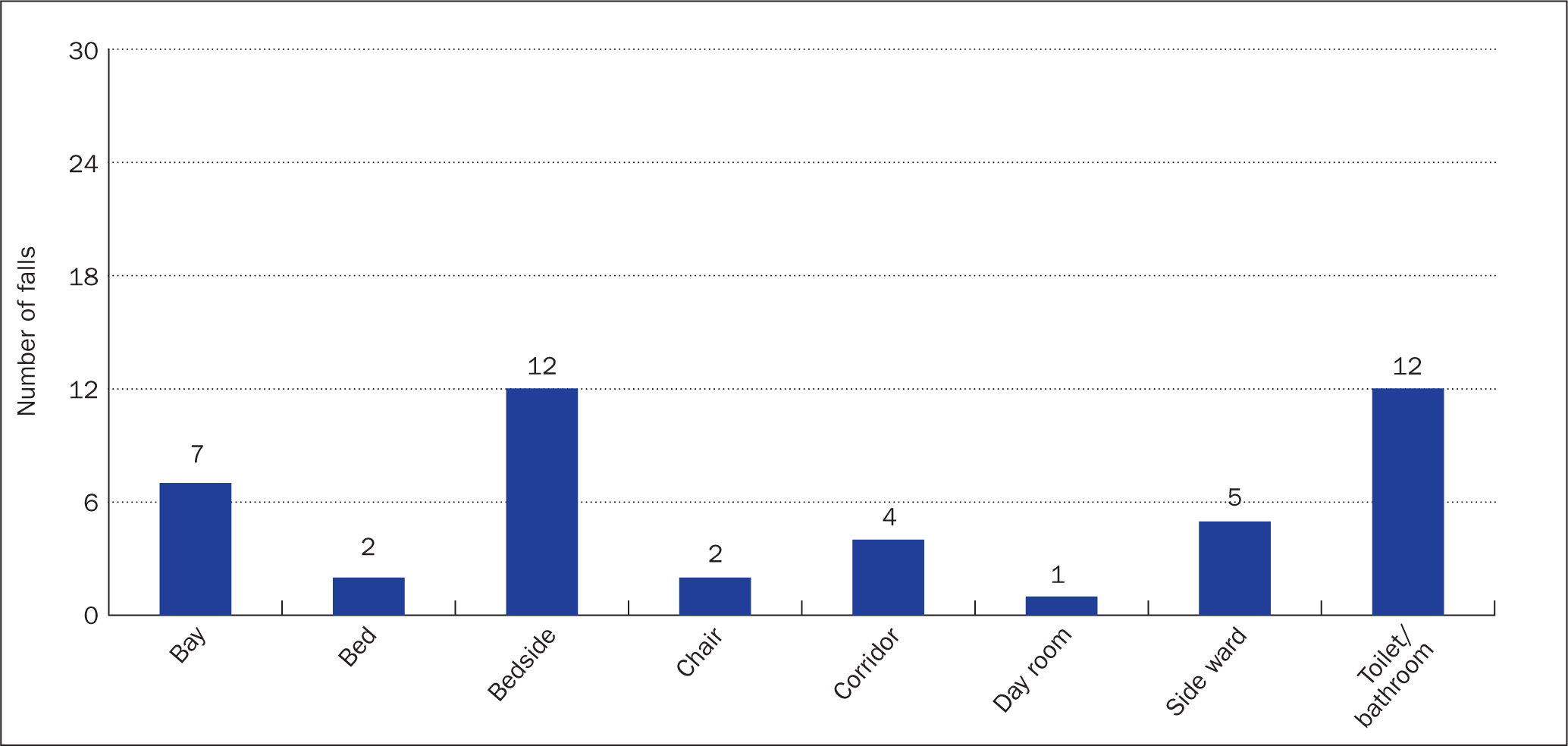
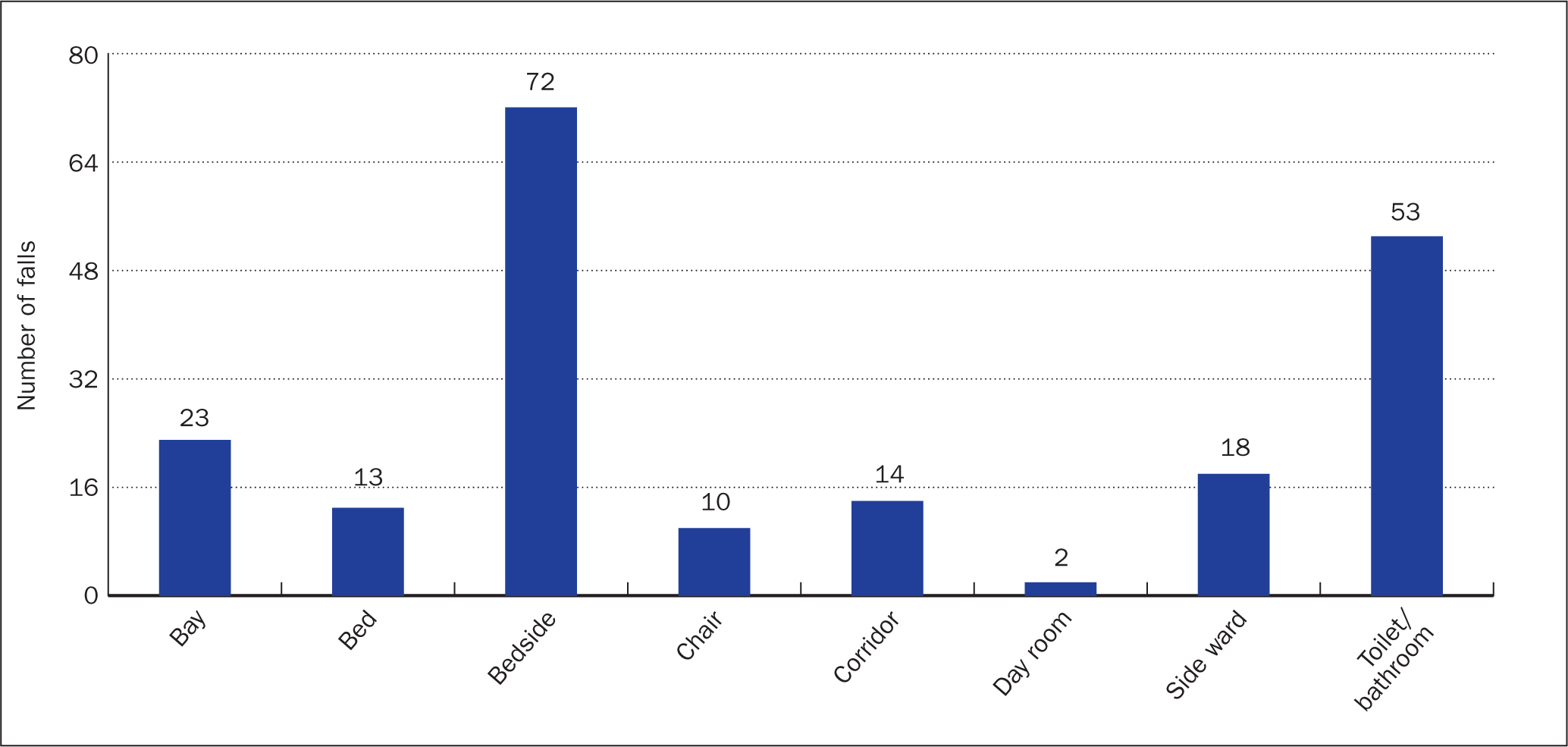
The results of this study showed that during 2022 the most common place for patients to fall was either in the toilet/bathroom or at the patient's bedside. It was noted that the majority of patient activities at the time of falls were reported was ‘toileting’ (Figure 2). Of the falls under cohort supervision 29% of incidents were at the toilet and 33% of falls took place at the bedside. These numbers were similar when patients were under one-to-one supervision, with 40% taking place at the bedside and 21% at the toilet. For the period 2019-2022 these numbers remained similar showing consistency with these findings (Figure 3).
Gender
In 2022, there were 61 falls within the division in patients who were under enhanced supervision: 44 (72%) of those were male and 17 (28%) were female. For the 3 years prior to this the data are very similar: in 2021, there were 32 (68%) male patient falls and 15 (32%) female; in 2020, there were 38 male (78%) and 11 (22%) female patient falls; and, in 2019, there were 33 (67%) male patient falls and 16 (33%) female patient falls. Over the 4-year period this works out at 71% of all patients who fell being male. These results show that within the division men were at significantly greater risk of falling than women. This is supported by a study from James et al (2018); however, other studies have shown that often this is not the case in other areas (Pereira et al, 2013; Greenberg et al, 2016). Further research would be useful to determine why these figures were so uneven.
Age
The average age of patients involved in these falls was 72 years. Interestingly, the average age of those who suffered no harm was 71, those who suffered low harm was 74 and those who suffered catastrophic harm was 77. This would indicate that the older the patient, the more likely they were to sustain worse harm. This is supported by Lamb (2015) who found that around 77% of inpatient falls occurred in patients aged 65 and over. Ghosh et al (2022) noted that the risk of falling with a higher level of injury severity increased by approximately 20% for patients aged 65–74 years, 29% for patients aged 75–83 years and 39% for patients aged over 84 when compared with patients aged 50 years or younger. This should guide staff to consider the patient's age when determining the likelihood of harm that could occur following a fall. In the data for the division presented here, the average age of those patients who suffered severe harm was 61 years, but there were only two patients in this category, making this a less reliable data set.
Time of falls
Throughout 2022, and indeed the 3 years prior to this, the timing of falls across the 24-hour period was fairly evenly spread. The most common times for falls were between 3:00 and 3:59 am (6 falls in 2022, 14 in the period 2019-2022). The majority of falls that took place between 7:00 and 11:59 (morning) took place in the bay, with some in the toilet. The majority of patients were under cohort supervision, but staff were not present at the time or busy with other patients. All of these falls resulted in no harm.
Of the falls that took place between 12:00 and 16:59 (afternoon) patients were more likely to be supervised but falls still took place; most falls in the bathroom occurred when patients were taken to the toilet but left for privacy.
During the evening time (17:00-20:59) there were two catastrophic falls noted. There were also more cases of being taken to the toilet and falling when left alone.
Twenty-two falls were reported during ‘bed time’ (21:00-06:59) nine of which occurred when the patient was left toileting alone. One fall occurred when the patient was outside in an accident. Ten falls occurred at the bedside or bay and one in a side room. It can be seen that, of the patients who fell, some were under cohort supervision but for various reasons staff were not present to help. On other occasions, staff should have been supervising a bay of patients but took one patient to the toilet, where they were left alone and fell. The staff member may have felt the need to ensure that the other patients in the bay were looked after. There were also occasions when patients were due to be put under cohort supervision but staff were busy with other patients. For patients under one-to-one supervision overnight it can be seen that three falls occurred when staff were not close enough to prevent a fall for various reasons and three instances where staff should have been providing one-to-one care but were not present.
Discussion
Falls remain one of the most commonly reported category of patient safety incidents within the division. It is imperative that this number is improved, however over the period 2019-2022 the top three learning outcomes from falls within the division were ‘patient supervision’ and ‘staff education’, followed by ‘no learning’. This shows that staff deemed that no learning had taken place in 23% of all falls under supervision. Educating staff to understand the importance of correct risk assessment is crucial in preventing falls (Gu et al, 2016).
Studies have shown that presence of a risk assessment process was found to be the most significant factor that led to a reduction in the number of falls because it allowed staff to devote additional attention to individuals who were at risk of falling. This alone was found to reduce the rate of falls by approximately 19% (Spoelstra et al, 2012). It is important that staff are given relevant training tools to analyse the effect of specific actions, nurses should also be given the ability to innovate and suggest alternatives that suit their clinical area (Bunn et all, 2014). It was also found that educating patients' family had a positive impact on falls. This involves informing families about a plan of care, the risks involved, and how to prevent falls. It has been shown that falls can occur during visiting periods outside the direct supervision of hospital staff. Training the family regarding the risk of falls allows patients to be continuously monitored by individuals actively engaged in preventing falls (Spoelstra et al, 2012).
The importance of educating patients should also be considered. Well-designed patient education programmes can improve knowledge and self-perception of risk, empowering them to reduce their risk of falling while in hospital (Heng et al, 2022). Unfortunately, it can be seen from studying the data that patients can engage in risk-taking behaviours that increase their likelihood of falling, such as not using the call bells and not waiting for staff before attempting to mobilise (Haines et al, 2012). Patient education should aim to increase patients' awareness of their own risks and provide them with strategies to mitigate these while in hospital. Various methods can be used, such as handouts (Huang et al 2015), posters (Kobayashi et al, 2017) and face-to-face discussion (Forrest et all, 2012). Heng et al (2022) argued that few studies have evaluated the outcomes or designs of educational material based on educational theory. Recent studies have shown that fall mitigation interventions that incorporate evidence-based design are successful at reducing falls (Hill et al, 2015).
It is important that trusts take a proactive approach to patient falls under supervision. Recent studies have shown that portable nursing stations were associated with lower monthly rates for falls (Ali et al, 2018). Two hospitals, Stoke Mandeville and Wycombe General, aimed to reduce inpatient falls by increasing nurse–patient contact time, using an intervention called Stay in the Bay (SITB). They introduced portable nursing stations in bays to allow nurses to do more of their routine work in the ward bays among patients, with the expectation of helping to reduce the inpatient fall rate. The monthly falls rate subsequently declined, it was felt that the nurses' presence and ability to reinforce safety instructions, such as use of walking aids, could play a part in this. It is suggested that this could minimise the level of patient harm as patients are assisted quickly (Ali et al, 2018). However, it is important that there is clear communication between nursing staff, so that, if staff need to leave a bay or an individual patient, other team members are made available to cover. Further research is needed in this area to determine whether learning outcomes are ‘trickling down’ from meetings at trust and divisional level to all members at ward level.
It was noted in this study that a large number of patients fell in the toilet or because of needing the toilet. In the post-fall documentation for many of these incidents it was stated that staff left the patient to maintain their privacy and dignity. It could be argued, however, that if patients are deemed at high risk and need enhanced supervision this should include all areas of the ward. A possible change to practice could involve asking patients on admission if they consent to staff being present, if they are needed, during toileting.
Exploration into further areas of falls management may be of use, studies have shown that the use of patient movement pads, or video monitoring as alternatives to supervision, are methods that could improve patient safety, and decrease sitter usage and cost for trusts. Further research would also be useful in developing the understanding of patient and staff experiences of enhanced supervision. One area to study further is patients' experiences and how these influence their independence and recovery. Jones et al (2019) noted that supervision was not focused on meaningful interaction, and patients were rarely involved in purposeful activities when being supervised. It could be argued that this can lead to the deconditioning of patients. Through understanding both sets of opinions it could lead to the understanding of barriers in the way of best practice
Conclusion
It can be seen that further improvements are needed in increasing the standard of enhanced supervision. Patients under these levels of supervision should, in theory, be better protected from falls; however, this study has shown that patients are still having falls resulting in harm. Themes can be identified through looking at incident rates in particular areas to determine specific patterns in these clinical areas and adaptations can be made to combat the problems highlighted. For example, if patients are more at risk of falls in the bathroom, can staff gain consent to assist them in this area to help with their needs? Further exploration on a larger scale would offer interesting insight into this area and could help improve the quality of nursing care provided.
KEY POINTS
- Incident reporting helps determine trends in patient safety, and themes identified can help shape how clinical areas improve their response to patient safety incidents
- Patients at high risk of falls should receive enhanced supervision when admitted to hospital; however, despite this patients are still falling and coming to harm
- Despite risk assessments there were still many instances where the correct care plan was not followed
- Those under supervision were often left alone at times, due to staffing needs or patient privacy concerns
- A higher proportion of male falls while under supervision were noted – reasons for this and influencing factors need to be explored
CPD reflective questions
- Why do you think that more male than female patients had falls when under supervision?
- What can be done to balance the need to uphold patient dignity and privacy with the need to ensure that patient safety is maintained at all times?
- How can patient supervision be improved to ensure greater safety?
- What areas of the ward or clinical area could be improved to decrease the likelihood of patients falling? How could patients' bedsides and toilets be improved to minimise the likelihood of harm?


