Age-related macular degeneration (AMD) is a major component of the workload of eye units across the UK. It also has significant physical and psychological effects on patients and places a huge burden on the healthcare system. The prevalence of wet AMD is currently estimated at around 679 000 cases, affecting 4.8% of patients aged 65 years and older and 12.2% of those aged 80 years and over (Owens et al, 2012). Older people need good vision to maintain their independence and quality of life and, with the increase in the UK's ageing population, treatment for AMD is vital.
Intravitreal injections for the treatment of AMD were introduced in 2012 and intravitreal anti-vascular endothelial growth factor (VEGF) medication is currently the only treatment for wet AMD; it is administered directly into the eye in the form of intravitreal injections. Patients treated with anti-VEGF medication for wet AMD may require a significant number of injections. In the experience of the ophthalmic unit at Great Western Hospitals, they require at least 17 injections over a 3-year period with some patients requiring more. Injections are initially given on a monthly basis, with their frequency then reduced thereafter to every 2 months or every 3 months. This was one of the recommendation of a benchmark clinical trial, which involved two studies in which patients were given 2-monthly intravitreal injections of aflibercept after an initial loading dose of monthly injections for 3 months (Heier et al, 2012).
With the large number of injections required per patient and the large numbers of patients requiring injections, there is a significant capacity issue within hospital eye services to treat patients with wet AMD. All patients also require regular optical coherence tomography (OCT) scans to image the retina and monitor the progress of the disease in relation to the treatment and an objective measurement of a patient's visual acuity. The use of intravitreal injection assistant devices reduces the time needed to deliver intravitreal injections and can help with the capacity issue facing almost all hospitals.
Other indications for treatment with anti-VEGF injections include retinal vein occlusion, which has an overall annual incidence in the UK of 0.5–2.0% in people aged over 50 years, and diabetic macular oedema, which has a prevalence of 2.8% in all patients with diabetes of all ages (Laouri et al, 2011). These patients usually require long-term treatment, hence the need for a safe, efficient and cost-effective way to deliver treatment.
A report from the Royal College of Ophthalmologists (RCOphth) (2017), The Way Forward, highlighted that two-thirds of ophthalmic departments in the UK have non-medical ophthalmic health professionals performing intravitreal injections. In the UK, ophthalmic nurse injectors perform more than 63% of intravitreal injections (RCOphth, 2017). However, training practitioners to achieve competence in delivering intravitreal injections independently can take a significant amount of time and resources. Due to the rise in the number of patients being diagnosed with wet AMD, and the subsequent increase in the number of intravitreal injections required, a majority of ophthalmology departments train ophthalmic nurse injectors to undertake the procedure (Michelotti et al, 2014), which was previously carried out solely by ophthalmologists.
In its report, the RCOphth (2017) recognised the importance of the role played by nurses in delivering high-quality ophthalmic care. Sixty-four percent of the units surveyed for the report depended on nurses to administer intravitreal injections, with an average of 12 injections performed by a practitioner per session, depending on the space and resources available. A systematic review of 31 303 intravitreal injections delivered by 16 ophthalmic nurse injectors found complication rates comparable with those for doctors: post-injection incidence of endophthalmitis (inflammation) ranged from 0% to 0.40% for nurses and 0% to 0.50% for doctors (DaCosta et al, 2014).
Rationale
The number of intravitreal injections required in the UK is set to increase by about 30% over the next 10 years, corresponding to an increase in the number of patients being diagnosed with wet AMD due to the increasing ageing population (Ruthford et al, 2012). The prevalence of diabetes is set to increase by 50%; this is relevant because maculopathy secondary to diabetes is the second most common indication for treatment with intravitreal injections (DaCosta et al, 2014).
Given the significant need for delivering an increasing number of intravitreal injections, in part by allied health professionals, the authors designed a 12-week educational programme at Great Western Hospitals NHS Trust to prepare nurses to become competent in administering intravitreal injections safely and efficiently, using an intravitreal assistant device (Precivia, FCI Ophthalmics).
Intravitreal assistant devices
The classical method of administering injections is to use a drape, speculum and callipers, which usually requires a trained doctor to perform the injection. Among the commercially available intravitreal injections assistant devices are the SP.eye intravitreal delivery guide (Salar Surgical) and the Malosa intravitreal injection guide (BVI), as well as the Precivia.
In a previous study (Hasan, 2018), the authors demonstrated a significant financial benefit from using the Precivia device (Figure 1). This study also illustrated the benefits that using the device has in training ophthalmic nurse injectors.

Training of nurse practitioners to perform intravitreal injections at Great Western Hospitals follows published guidelines (DaCosta et al, 2014) (Box 1), as well as being aligned with the RCOphth's Ophthalmic Common Clinical Competency Framework (RCOphth, 2019) curriculum. The Swindon training model (Figure 2) consists of the following components:
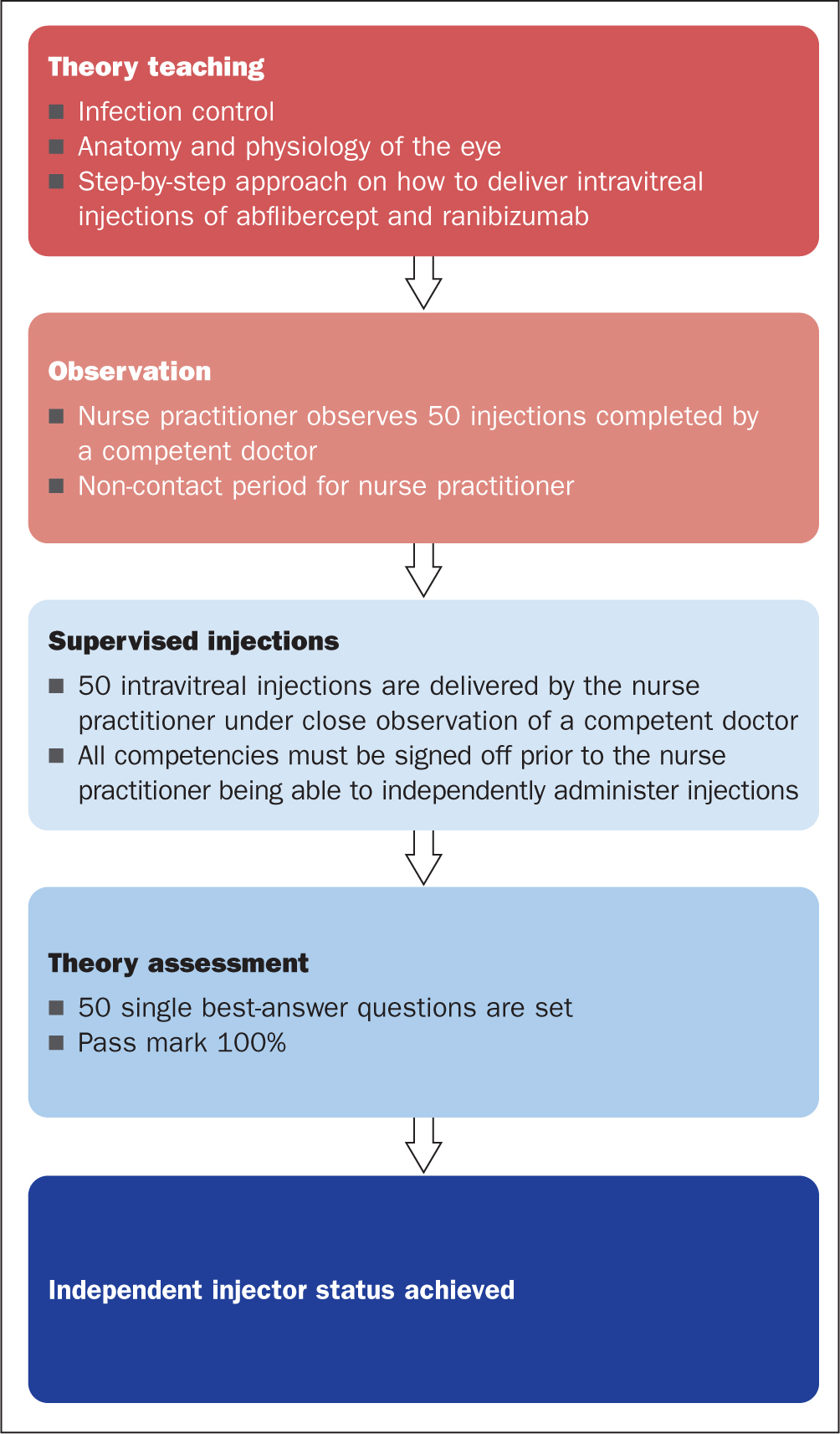
Figure 2 demonstrates the training path taken by nurses at Great Western Hospitals to become independent practitioners.
Since 2015, the Precivia assistant device has been used as standard at Great Western Hospitals. It is made from a transparent polycarbonate mould that fits around the cornea with a central window allowing for patient fixation. It includes a guide tube positioned at a 28° angle, through which the needle is passed to deliver the injection at a fixed distance of 3.5 mm from the corneal limbus. Use of this device enabled the service to reduce the cost of the consumables associated with administering intravitreal injections by 50%, and it also made the injection process significantly faster, enabling the service to safely increase the number of patients per injection list from an average of 13 to 17 (Hasan, 2018).
Local audit data from Medisoft (Electronic Patient Record) at Great Western Hospitals show that between 2014 and 2019 nurses performed more than 30 000 intravitreal injections using the Precivia device, with a complications rate in line with national data (Simcock et al, 2014).
The authors also distributed a questionnaire to ophthalmic nurses at the hospital who perform intravitreal injections independently using the device to obtain their views about it. The nurses strongly supported the use of the device because it provides a standardised way to administer the injections and incorporates a number of safety features.
Patient feedback
We interviewed 169 patients who were undergoing regular intravitreal injections performed by nurses to obtain feedback about their experiences. Of the total, 77% strongly agreed that their nurse was more friendly and sensitive to their needs compared with their previous experience of intravitreal injections performed by a doctor. Only 12.4% strongly agreed that a doctor would be more suitable to administer the injections. Seventy-five percent of patients stated that they were very happy with the care, with just 0.4% thinking that the nurse was unsafe to give the injections, although there were no complications (Hasan et al, 2017).
Setting up a successful nurse-led service (Swindon model)
In September 2019, the authors organised the region's first training course that provided a hands-on experience for nurses and doctors from across the country. The objective of the course was to use the Swindon training model (Figure 2) to provide delegates with an objective and structured approach to learning how to perform intravitreal injections safely. The course consisted of the following presentations:
The path for becoming a nurse injector and competency documentation
This topic was presented by a senior ophthalmic staff nurse who, at the time, had performed more than 6000 intravitreal injections. The presentation included an explanation of the training process and how to document the progress in training and the final assessment. It also highlighted the professional qualities necessary for a practitioner to deliver injections, such as being calm under pressure, and their personal qualities, such as empathy.
Introduction to Precivia, cost-effectiveness and patient feedback
The second presentation was delivered by a specialty doctor, which included a discussion on the benefits of the Precivia device, as well as an outline of the cost-effectiveness model, safety audit and patient feedback.
Tips for becoming a successful practitioner
One of the sisters presented her experience with administering injections in challenging situations and how to overcome these, for example, how to approach and manage nervous patients, or patients with small eyes and difficult positioning. Specifically, our team has some key clinical pearls that we feel nurse injectors could benefit from:
How to run a successful intravitreal injection service
An ophthalmology specialty trainee doctor presented a video course demonstrating how Swindon delivers an efficient intravitreal injection service, including the role of co-ordinators and virtual clinics. A version of the presentation is available on YouTube (https://youtu.be/as197vKldAI).
Injections clinics at Great Western Hospitals are based on the Swindon's fixed-dose treatment regimen in which patients start with a monthly intravitreal injection of aflibercept for 3 months (loading dose), followed by 2-monthly injections to complete 1 year. This allows the injections clinics to run independently from doctors' assessment clinics (two-stop method). Patients have an OCT scan of the macula and see a doctor or have their notes reviewed virtually on alternate visits.
The training course also included a number of video demonstrations of the use of the Precivia device, the injections process and an overview of the facilities and resources needed to set up the service.
The main theme of the course was to keep the sessions interactive by asking participants to vote on various topics and questions discussed during the course lectures, such as whether participants thought it would be easy to use injection assistant devices or not, using interactive polling software, as well as through interactive discussions lead by a consultant ophthalmologist.
Participants' feedback
There was a total of 22 participants in the course, the majority of whom were nurses, with the remainder made up of doctors and managers. Most participants (86%) were female. Participants responded to questions on current intravitreal injection practices in their units (Figure 3 and Figure 4) that came up throughout the course. The vast majority of participants had not performed intravitreal injections, so most of them were coming to learn the process for the first time.
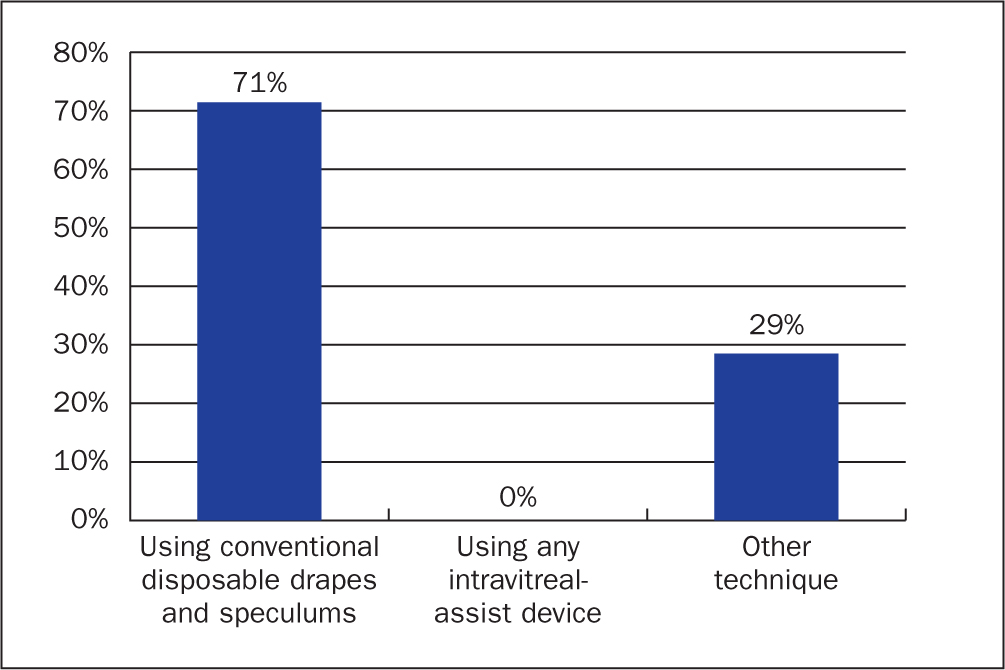
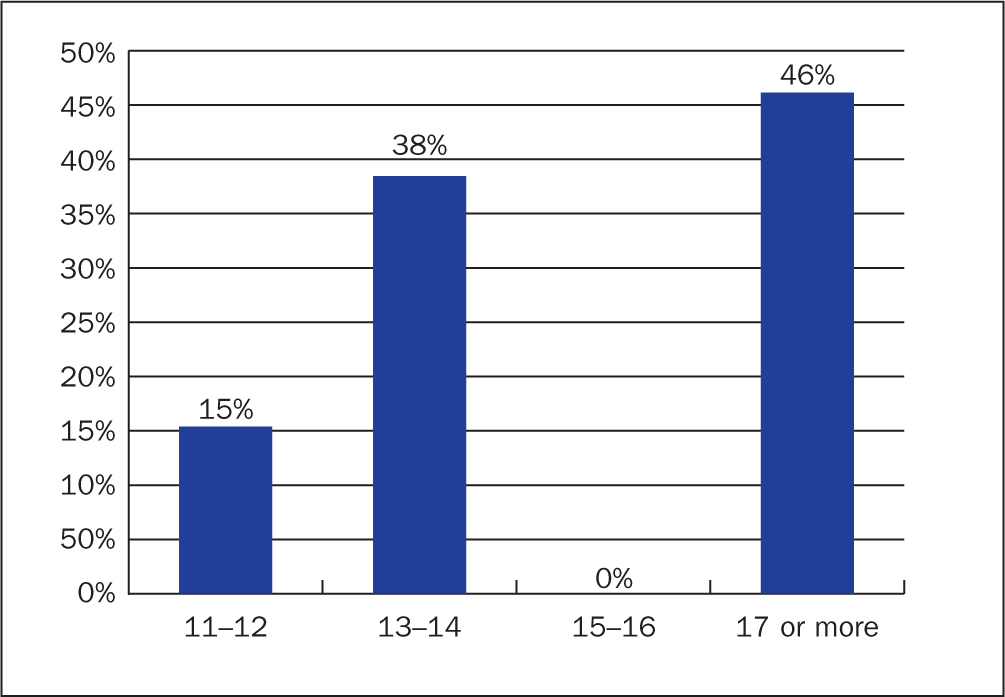
In units where injections were performed, 71% of these used disposable drapes and speculums; in the remaining 29% other methods were used, such as reusable speculums, but none reported experience of using Precivia or alternative assistant devices (Figure 3). At the time the course took place, the number of injections performed per session in each of the participant's clinics was as follows: 17 or more injections, 46%, less than 17, 54%, and the eye clinics were doctor or nurse led. At Great Western Hospitals the average number of injections performed by nurses was, and continues to stand at, 17-18 injections per nurse per session (Figure 4).
The most common types of anaesthetic used in the units in which the participants worked were: proxymetacaine (77% of responses), tetracaine (18%) and oxybuprocaine (6%).
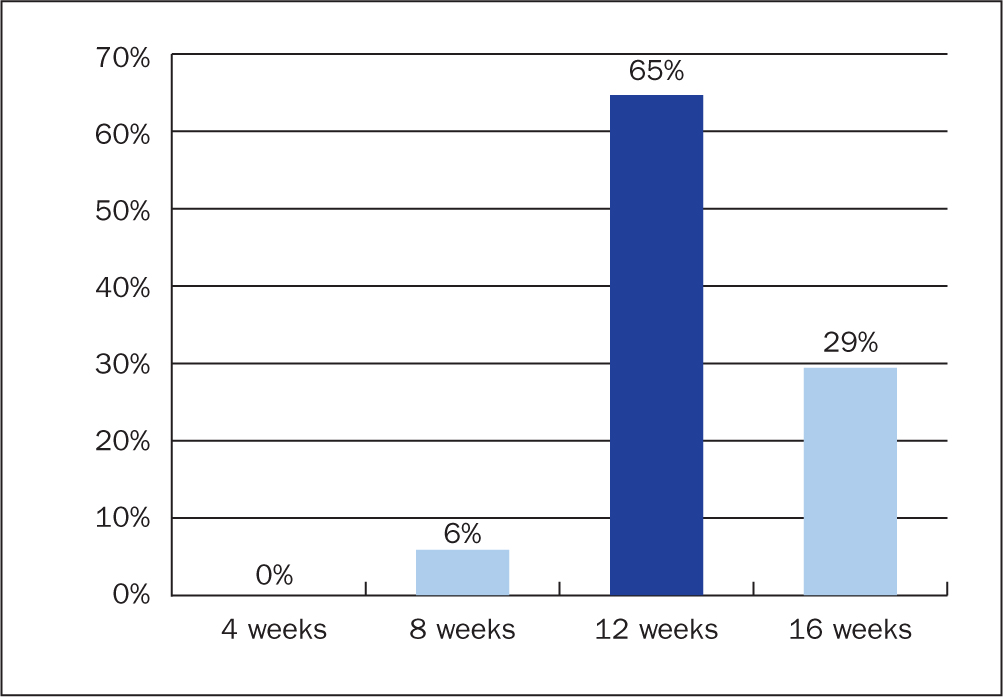
The authors also asked delegates to tell us how long they thought it would take to train an ophthalmic nurse practitioner to perform injections independently: 6% of those who responded said 8 weeks, 29% responded 16 weeks, with the majority (65%) saying 12 weeks (Figure 5). The length of the structured training process at the Great Western Hospital is 12 weeks.
During a lecture on cost analysis, 90% of the delegates agreed that the use of intravitreal assistant devices reduces the cost of injections. In addition, 100% of delegates reported that using intravitreal assistant devices did not increase the risk of developing endophthalmitis.
At Great Western Hospitals, iodine is the standard disinfectant, used, which is the standard method of disinfecting the eye surface prior to an invasive procedure, and 100% of course participants reported similar practice in their units.
Feedback
After participants had had the chance to practice administering intravitreal injections using the Precivia device on manikin eyes, the authors obtained feedback about their experience. This aimed to reflect the quick learning curve for using the device and the link between the theoretical and practical parts of the course, which mesh together to provide the practitioner with the confidence needed to perform this skill.
Course participants gave an overall rating of 8.9 out of 10 for the quality of the presentations, with 75% rating the course content as ‘excellent’. On the course overall, 75% gave it an ‘excellent’ overall rating (Table 1). The course aimed to enrich the participants' experience by including sessions on dealing with technically challenging patients, such as wheelchair users or patients with dementia, and the tips and tricks for becoming a successful injector.
| Item | Not useful | Somewhat useful | Very useful | Excellent |
|---|---|---|---|---|
| Overall rating of the course | 0% | 0% | 25% | 75% |
| Content of the course | 0% | 0% | 45% | 55% |
| Information about Precivia | 0% | 5% | 20% | 75% |
The overall quality of presentations was also given a high score, with an average rating of 8.9 out of 10. The authors included a presentation about the design and properties of the Precivia device to highlight its advantages—that is, the features that enable us to use it successfully. The feedback showed that 75% of participants rated this information as ‘very interesting’, and 20% as ‘somewhat interesting’. In terms of being valuable in their work in future, the feedback showed that:
| Item | Not likely at all | Somewhat likely | Very likely |
|---|---|---|---|
| How likely are you to use Precivia in your practice? | 5% | 40% | 55% |
| How likely are you to recommend this course to colleagues? | 0% | 15% | 85% |
Discussion
The safety of a nurse-led intravitreal injections service has been established, and it is now an integral part of the health system in the UK, with the level of skills complexity equivalent to doctor-led services (Bolme et al, 2019). Advanced nursing practice is one of the ways in which the NHS has evolved to meet increasing demand in many areas, including intravitreal injections. Assistant devices have revolutionised the training of nurses to perform intravitreal injections safely, with confidence, enabling them to also provide ophthalmology units with the much-needed capacity and cost-effectiveness.
A randomised-controlled trial by Bolme et al (2019) found that nurse-led injections services are ‘non-inferior’ to those that are doctor-led, with many ophthalmic units across the UK and Europe either already relying on nurses to deliver injections or in the process of training nurses to do so.
The course at Great Western Hospitals is the first in the region to have offered such training to its nurses and other non-medical practitioners, garnering an impressive amount of interest in the service, with delegates coming from across the UK to take part in the course. The eye unit at Great Western Hospitals has been pioneering the training of nurse practitioners to perform intravitreal injections safely and efficiently using the Precivia device in the region and 90% of injections at the hospital are now being successfully administered by nurses.
Among the positive ramifications of our training programme, the most important is that it has offered nurses the opportunity to take on more responsibility, to be more involved with a patient's treatment and to develop new clinical skills.
There were a number of challenges at the initial setting up of the service. Finding the time to provide training is the biggest issue and this cannot be emphasised enough. Time must be set aside in order to give the best quality training to ophthalmic nurse practitioners because, if we do not do this, we cannot expect them to deliver the best quality care. In addition, support from management is essential; at Great Western Hospitals, management has supported the initiative with additional funding in terms of higher salaries for nurse practitioners undertaking intravitreal injections and ensuring that they have reduced clinical workloads when they are undertaking training sessions. We encourage any readers who want to set up a similar system in their hospital to work closely with managers and key stakeholders in order to achieve a successful training programme.
Conclusion
We have primarily organised this training course for nurse practitioners looking to become competent in delivering intravitreal injections; however, it is also suitable for junior doctors and doctors in training to become consultant ophthalmologists. At the Great Western, we have demonstrated that the Swindon model provides a safe, efficient and cost-effective method of establishing a nurse-led intravitreal injections service using an intravitreal assistant device. The course was organised to share our experiences with nurse practitioners from across the country and we have since received encouraging feedback.
To the best of our knowledge, this is the first course that uses an intravitreal injections assistant device to train nurse practitioners in delivering intravitreal injections. The unit had plans to run another course this year, however due to the current COVID-19 pandemic, these plans have been postponed until September next year.

