Creation of an ostomy in the abdominal area is a commonly performed general surgical practice. The consequence, however, can be life-changing for the patient and, despite careful pre-operative planning, postoperative complications are likely to occur (Shabbir and Britton, 2010; Malik et al, 2018). Peristomal skin complications (PSCs) are some of the most frequently reported complications and the latest evidence has shown that up to 88% of people with an ostomy suffer from PSCs (Fellows et al, 2021). The Ostomy Skin Tool (OST) was developed in 2008 and validated as a standardised instrument for assessing both the extent and severity of changes in the peristomal skin condition of people living with an ostomy (Martins et al, 2008; Jemec et al, 2011). The OST is primarily based on clinician-reported outcomes and used to document the visual signs of the peristomal skin. Specifically, this tool focuses on changes in three domains: discolouration (D), erosion (E), and tissue overgrowth (T), summarised in a DET score (Martins et al, 2010). The three domains are scored according to the percentage of area under the adhesive that is impacted and the severity of the symptoms such as bleeding, itching, pain, burning and moisture. The composite DET score is defined on a scale from 0 to 15, and subjects are subsequently assigned to one of the four severity categories: ‘normal skin’ (DET=0), ‘mild’ (DET=2-3), ‘moderate’ (DET=4-6), or ‘severe’ (DET=7-15) (Jemec et al, 2011). Thus, the OST has been used for many years as a validated instrument for health professionals to perform standardised evaluation and treatment of PSCs.
However, one major limitation of the OST is that it is dependent on the presence of some level of discolouration in the peristomal area. In the absence of discolouration, the DET score will be zero, and the peristomal skin will be assessed as ‘normal skin’ without any complications (Jemec et al, 2011). From a recent multinational survey of people with an ostomy, it was reported that 75% of participants without peristomal discolouration still experienced other symptoms of PSC (eg pain, itching and burning sensations) (Fellows et al, 2021). Therefore, people with an ostomy experiencing symptoms of PSC in the absence of discolouration are at risk of being incorrectly categorised as having healthy and unaffected skin when using the DET score as a metric.
With these limitations in mind, the aim of this study was to develop a new tool, OST 2.0, including a patient-reported outcome (PRO) questionnaire, to allow for the capture of a more sensitive range of non-visible PSC symptoms alongside visible complications and an objective assessment of the area of discoloured peristomal skin.
To demonstrate the applicability of the new tool, a data set from the Ostomy Life Study (Fellows et al, 2021), including more than 4000 participants living with an ostomy, was used as an example to illustrate self-assessed severity levels of PSCs in the general population of people living with an ostomy.
Methods
Study design
The study was based on qualitative interviews with people with an ostomy experiencing PSCs and health professionals who managed or treated PSCs. The study was non-interventional; no medical products or devices were administered to participants as part of the study, and participation in the study did not impact the participants' routine or medical care in any way. Health professionals were required to be an ostomy care nurse, a dermatologist, or a surgeon with experience of working with PSCs. The study was carried out by a team of external consultants, specialising in clinician and PRO research. Partner recruitment agencies in the USA and the UK were responsible for recruiting participants via a database of respondents on a patient panel. Written informed consent was obtained prior to any research activities being conducted and before the health professional shared any medical information about the subject. All participants provided written informed consent for the interview to be audio-recorded and transcribed verbatim. Health professionals were recruited via a third-party recruitment agency or through the global Coloplast Ostomy Forum (COF) and an established Coloplast skin expert panel. Health professionals were asked to complete a screening form to collect further details about their demographics and professional history, to better determine eligibility for the study.
Ethical approval
Ethical approval was obtained from an international institutional review board, Salus (Protocol Number CB8067A), before any study-related interview activities.
Qualitative interviews
A semi-structured interview guide was developed to help facilitate discussions between the participant (person with an ostomy) and interviewer, and to ensure consistency between the interviews. The interview guide was in three sections: ‘Introduction to study’ (5 minutes), ‘Concept elicitation’ (CE) (40 minutes), and ‘The OST assessment’ (15 minutes).
Similarly, a semi-structured health professional interview guide was developed to help facilitate discussion between the health professional and interviewer, and to ensure consistency between interviews. The interview guide was broken down into two sections: ‘Introduction’ (5 minutes) and ‘Concept elicitation interview’ (30 minutes).
The qualitative interviews were conducted in two rounds. This two-step approach allowed for the interview guide to be updated based on findings from the first round of interviews. Additionally, conducting the interviews in two rounds allowed for development of the OST 2.0 to be adapted between the rounds and the changes to be tested with the health professionals in the second round of interviews.
Interviews of people with an ostomy
The interviews lasted approximately 1 hour and were conducted via telephone or Skype. The aim of the concept elicitation interview was to explore the participants' experience of PSCs associated with an ostomy, in an open-ended and unbiased manner, fully exploring all concepts of interest. Initial discussions comprised a series of broad open-ended questions designed to spontaneously elicit information regarding the subjects' experience of PSCs. Following this, subjects were asked more focused questions designed to probe issues that they may not have mentioned or that may have been insufficiently explored. This information was important for ensuring that all study objectives were met and that all study questions were answered. Based on this, it was possible to identify the concepts that were most important to the subjects. The last section of the interview guide specifically focused on the concepts included in the OST without showing the actual tool.
Health professional interviews
The health professional interviews lasted approximately 35 minutes and were conducted via telephone or Skype. The aim of the concept elicitation interview was to further understand the diagnosis, treatment and management of PSCs in an open-ended and unbiased manner. Following this, health professionals were asked more focused questions designed to evaluate issues they may not have mentioned spontaneously and to ensure all concepts of interest were discussed in detail. Following the first round of interviews, the health professional interview guide was adjusted to ensure that all concepts of interest were explored for the second round of interviews.
Coloplast skin expert panel
The expert panel was established, and members selected based on their clinical expertise within ostomy care and their professional background. The panel encompassed two dermatologists and three ostomy care nurses with each of the members having more than 30 years' experience within the field of ostomy skin care and treatment of PSCs. Collectively, this panel enabled a highly relevant reference for development of the OST 2.0.
Consensus on content of the PRO questionnaire
Following analysis of all the conducted interviews, the findings were compared to identify the most important complications associated with PSCs. Findings from the interviews were then discussed in a series of meetings with the engaged external consultancy team, the Coloplast project team, and the skin expert panel. Based on these meetings, a consensus on modifications to the OST was reached, and the PRO questionnaire was developed and included in the OST 2.0.
Image analysis: automated assessment of discolouration of the peristomal skin
The assessment of the discolouration of the peristomal skin area was performed using a recently developed algorithm based on artificial intelligence (Andersen et al, 2020). This image analysis technique was applied to peristomal skin photographs, which were taken by subjects themselves, after each ostomy product change. Based on this, it was possible to objectively quantify the total area of discoloured skin in the peristomal area.
Decision tree model: establishing a combined score
To define a combined score based on the outcome from the PRO questionnaire and assessment of discoloured peristomal skin area, a decision tree (DT) methodology was applied. The combined score (hereafter called the DT score) was translated into severity categories, which were established in collaboration with the Coloplast skin expert panel who provided input to the proposed scoring thresholds and confirmed the hierarchical nature of the concepts covered. This ensured that categories were both relevant and made sense to the health professionals. Following this, online workshops were held where the severity categories were reviewed by global and national COF boards. The board members provided feedback on the severity categories by answering a questionnaire, and the categories established in collaboration with the Coloplast skin expert panel were thereby verified.
Data set to demonstrate applicability of the model
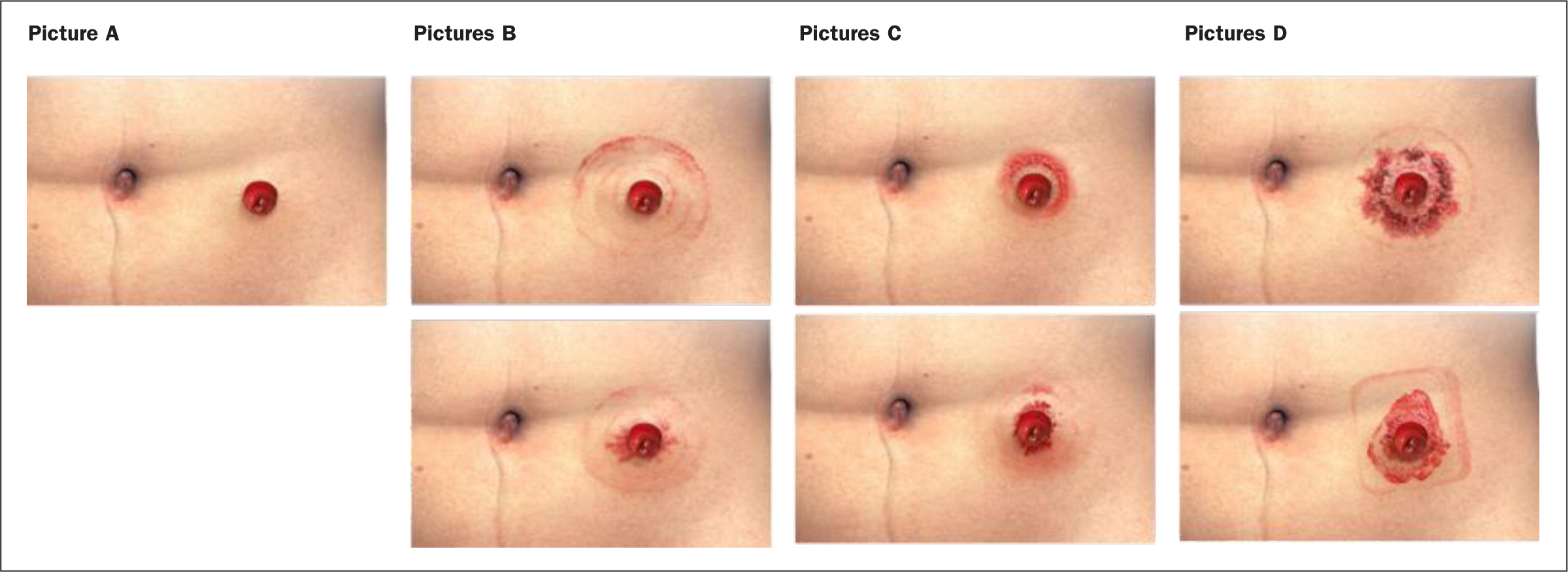
To demonstrate the applicability and sensitivity of the OST 2.0 DT model, a subset of data from a large, multinational survey was used, namely the Ostomy Life Study (Fellows et al, 2021), including 4209 eligible subjects. The survey included the PRO questions from the OST 2.0. However, as it was not possible to ask participants to take pictures of their peristomal skin area and use the automated assessment of discolouration, they were asked to select between illustrations of various levels of discolouration, as shown in Figure 1.
Results
Study sample
Ten people with an ostomy were recruited for the qualitative concept elicitation interviews. They were required to have experienced PSCs associated with an ostomy and were recruited from the UK and the USA. A total of 14 health professionals from the UK, USA, and Europe—nine ostomy care nurses, four dermatologists, and one surgeon—were recruited for the interviews as well. All health professionals were fully informed about the study and provided full written informed consent to participate.
Demographics of study sample
The demographic characteristics of the participating subjects for the qualitative concept elicitation interviews are outlined in Table 1 and Table 2. The mean age of the people with an ostomy was 48.4 years, and there was an over-representation of females compared with males. There was an even distribution of subjects being employed (40%) and being unable to work due to their medical condition (40%). The majority of participants had an ileostomy (60%). Finally, the cause of an ostomy was primarily inflammatory bowel diseases including ulcerative colitis and Crohn's disease, or cancer (Table 1).
Table 1. Demographic characteristics of people with an ostomy participating in qualitative concept elicitation interviews
| Demographic | Total (n=10) | Demographic | Total (n=10) |
|---|---|---|---|
| Age (years) | Type of ostomy, n (%) | ||
| Mean | 48.4 | Ileostomy | 6 (60) |
| Minimum, maximum | 37, 70 | Colostomy | 3 (30) |
| Sex, n (%) | Urostomy | 2 (20) | |
| Female | 7 (70) | NB: 1 participant had both an ileostomy and a urostomy | |
| Male | 3 (30) | ||
| Location, n (%) | Cause of ostomy, n (%) | ||
| UK | 6 (60) | Ulcerative colitis | 3 (30) |
| USA | 4 (40) | Crohn's disease | 2 (20) |
| Work status, n (%) | Cancer | 2 (20) | |
| Working full/part time | 4 (40) | Hysterectomy accident | 1 (10) |
| Not working due to medical condition | 4 (40) | Chronic urinary incontinence | 1 (10) |
| Retired | 2 (20) |
Table 2. Demographic characteristics of health professionals participating in qualitative concept elicitation interviews
| Demographic | Ostomy nurses (n=9) | Dermatologists (n=4) | Surgeon (n=1) |
|---|---|---|---|
| Years of experience | |||
| Mean | 21.2 | 10 | 21 |
| Range | 8–35 | 8–13 | N/A |
| Country, n (%) | |||
| UK | 3 (33) | 4 (100) | 1 (100) |
| USA | 2 (22) | 0 (0) | 0 (0) |
| Canada | 2 (22) | 0 (0) | 0 (0) |
| Denmark | 1 (11) | 0 (0) | 0 (0) |
| Belgium | 1 (11) | 0 (0) | 0 (0) |
| Work setting, n (%) | |||
| Hospital | 7 (78) | 4 (100) | 1 (100) |
| Community setting | 1 (11) | 0 (0) | 0 (0) |
| Outpatients clinic | 1 (11) | 0 (0) | 0 (0) |
| Average % of time spent working with each type of ostomy patient, mean (range %) | |||
| Ileostomy | 43 (10–70) | 20 (1–45) | 30 |
| Colostomy | 33 (10–60) | 28 (3–60) | 20 |
| Urostomy | 11 (2–20) | 16 (5–45) | 10 |
| Other (gastrostomy; fistula) | 2 (30; 5) | 0 | 0 |
For the ostomy care nurse population, the average years of experience within the ostomy care field was 21.2 years (range: 8-35 years), for the dermatologist population 10 years (range: 8-13 years) and for the surgeon interviewed 21 years (Table 2). The most frequently reported work setting was within a hospital (n=7/9 ostomy care nurses; n=4/4 dermatologists; and n=1/1 surgeon). One ostomy care nurse worked within a community setting and one nurse worked within an outpatient clinic. Most of the health professionals spent more time working with ileostomy patients than individuals with any other ostomy type.
PSC symptoms identified
Based on the concept elicitation interviews, a detailed overview of the spontaneously and probed symptoms of PSCs was summarised for both interviewed groups. Figure 2 shows the responses from the 10 people with an ostomy, where there was a mix of visible symptoms (eg, redness) and non-visible symptoms (eg, pain). The most frequently reported symptom included redness (n=10), painful/sore/sensitive skin (n=10), itching (n=9) and irritation (n=9).
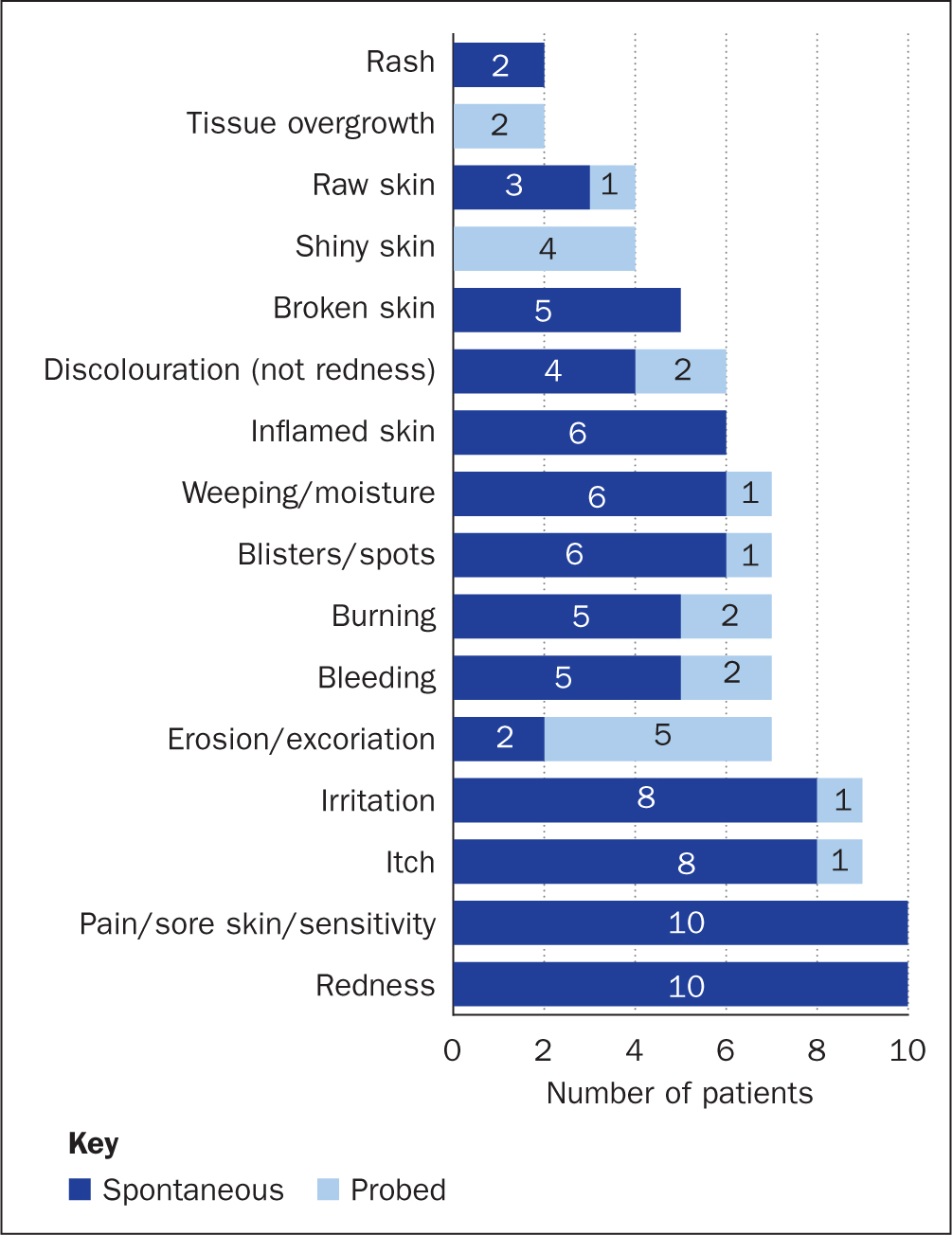
Figure 3 shows the responses from the health professional interviews, which again are a mix of visible signs and non-visible symptoms. The visible signs most frequently reported by the 14 health professionals were: infection (n=11), redness (n=11), erosion (n=8), ulcers (n=7), moist/wet skin (n=7), dry skin (n=5), inflamed skin (n=5) and weeping skin (n=5). The non-visible symptoms most frequently reported by the health professionals were: pain/sore skin/sensitivity (n=12), itch (n=10), and a burning sensation (n=7).
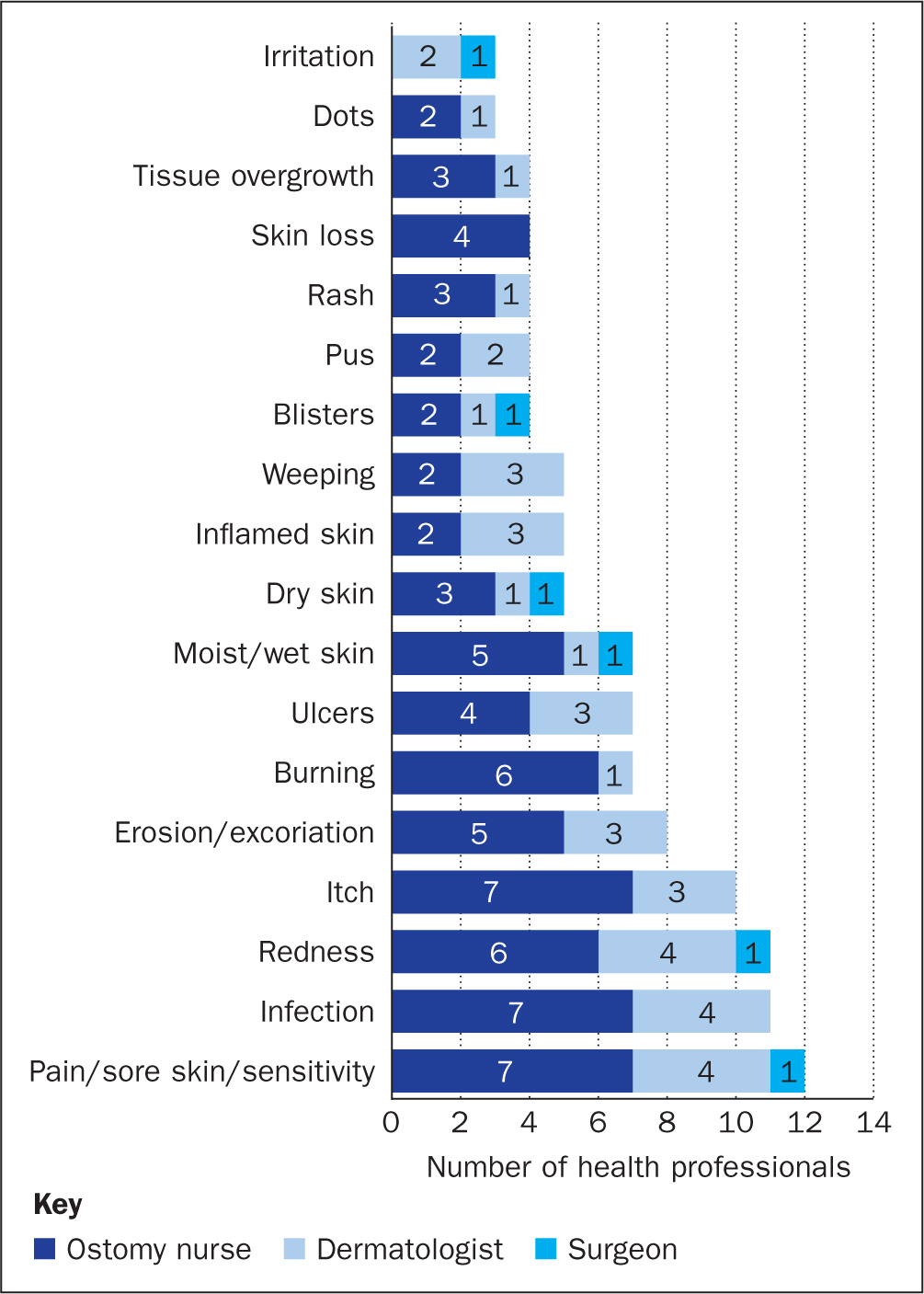
Table 3 outlines the top nine most frequently reported PSCs with indication of symptoms identified by both populations. Specifically, redness, pain, itching, erosion, burning, and weeping/moist skin were among the top nine symptoms reported by both groups and considered important complications associated with having skin issues in the peristomal area. In addition to this, irritation, bleeding, and blisters/spots were only reported by people with an ostomy, whereas infection, ulcers and dry skin were reported solely by health professionals.
Table 3. Top nine most reported PSC symptoms for people with an ostomy and health professionals
| People with an ostomy* | Health professionals* |
|---|---|
| Redness | Pain/sore skin |
| Pain/sore skin/sensitive | Infection |
| Itch | Redness |
| Irritation | Itch |
| Erosion | Erosion |
| Bleeding | Burning |
| Burning | Ulcers |
| Blisters/spots | Moist/wet skin |
| Weeping/moisture | Dry skin |
Outline of the PRO questionnaire
The resulting OST 2.0 PRO questionnaire is summarised in Table 4. All questions are asked just after a change of an ostomy baseplate. Questions 1-3 focus on the symptoms of bleeding, weeping and ulcers/sores (visual symptoms of eroded compromised skin). This was asked on a dichotomous response scale (experiencing/not experiencing). Questions 4-6 focus on symptoms of itching, pain and burning (non-visible/sensation symptoms). For each symptom, the subject was asked to recall the severity of the symptom at its worst since the last ostomy product change on a scale from 0 (no symptoms at all) to 10 (worst possible level of symptoms).
Table 4. Patient-reported outcomes questionnaire
| Question | Response options |
|---|---|
| 1. Do you experience any bleeding from the skin around your stoma right now when changing your product? | Experiencing/not experiencing |
| 2. Once you have cleaned and dried the skin, do you still experience any weeping or moisture on the skin around your stoma right now when changing your product? | Experiencing/not experiencing |
| 3. Are you experiencing any ulcers or sores around your stoma right now when changing your product? | Experiencing/not experiencing |
| 4. Please rate on a scale from 0–10 how itchy the skin around your stoma has been at its worst since you last changed your product | 0–100=none, 1=very mild, 10=worst possible |
| 5. Please rate on a scale from 0–10 how painful the skin around your stoma has been at its worst since you last changed your product | 0–100=none, 1=very mild, 10=worst possible |
| 6. Please rate on a scale from 0–10 any burning feelings from the skin around your stoma at its worst since you last changed your product | 0–100=none, 1=very mild, 10=worst possible |
Decision tree score
The PRO and image analysis data were combined in a DT score to enable an overall assessment of the peristomal skin for each participant. The score on a scale of 0-3 was defined by the external consultants. The DT model provides a hierarchy of the scores and assigns a skin severity level to each subject based on the observed combination of these variables (PSC symptoms identified in the PRO and image analysis), as detailed in Figure 4. Overall, the PSC symptoms were divided into three groups: ‘compromised broken skin’ (ulcers, bleeding, weeping skin), ‘sensation symptoms’ (pain, itching, burning) and ‘discolouration without broken skin or sensation symptoms’. The flow chart outlined in Figure 4 dictates how a patient will fall into one of the four health states of treatment categories depending on the combination/level of PSC symptoms: ‘no treatment required’ (DT=0), ‘mild’ PSC (DT=1), ‘moderate’ PSC (DT=2) and ‘severe’ PSC (DT=3). For instance, if a person presents with peristomal ulcers or bleeding, this person will fall into the ‘severe’ category. In contrast, the maximum value of either pain, itching or burning can bring a person into either a ‘mild’, ‘moderate’ or ‘severe’ category depending on the severity level of this sensation symptom. Finally, people presenting with peristomal discolouration alone will be categorised as either having ‘mild’ PSC (>10 cm2 discoloured skin) or ‘No treatment required’ PSC (≤10 cm2 discoloured skin).

Applicability of the OST 2.0
The peristomal skin condition was self-assessed by 4209 people with an ostomy participating in the Ostomy Life Survey (Fellows et al, 2021). All subjects answered the PRO questionnaire from OST 2.0 at a cross-sectional time point, and to accommodate the unavailability of pictures of the peristomal skin the participants were asked to choose between seven illustrations resembling different levels of discolouration (Figure 1).
Figure 5 shows the distribution of the 4209 participants' own assessment of their peristomal skin condition and respective levels of severity; 754 participants assessed that they had ulcerated/sore peristomal skin area (‘severe’ PSC), 324 had weeping/moist skin of whom 69 also had either pain, itching or burning skin sensations scoring 7 or more (on the 0-10 points scale). Based on the tool, 997 participants had a ‘mild’ PSC due to either pain, itching or burning sensations scoring 1-3, whereas 345 participants rated pain, itching or burning sensations to be at the level between 4 and 6 (‘moderate’ PSC), and 185 participants rated these symptoms to be at the highest severity level of 7-10 (severe PSC). Of those with a PSC, 127 had discoloured skin without any other visible signs or sensation symptoms and, out of the 127 participants with discoloured skin, 90 were assessed to be ‘no treatment required’ due to a discolouration area of 10 cm2 or less. Finally, 503 assessed their peristomal skin to be normal (without any PSC) corresponding to 12% of the 4209 participants.

Discussion
The most common postoperative complication after surgical formation of an ostomy is PSCs (Persson et al, 2010; Shabbir and Britton, 2010; Malik et al, 2018). The degree of peristomal skin irritation may range from a mild peristomal dermatitis to full-thickness skin necrosis and ulceration. To avoid severe complications, it is important that people with an ostomy check their peristomal skin condition on a regular basis and seek professional help and advice in a timely manner. Nevertheless, access to health professionals may not always be available on a regular basis with face-to-face consultations. Thus, it is important to find alternative ways to monitor the condition of peristomal skin and methods to facilitate a constructive dialogue between a patient and the health professional that ultimately can suggest the right treatment and/or advice to prevent PSCs. One solution is to provide a simple and validated assessment tool with a common language that is easily understood by both parties.
This study presents the development of OST 2.0 as an assessment tool to be used both by people with an ostomy to evaluate their peristomal skin condition on a regular basis and by health professionals in their daily practice. The OST 2.0 also includes a combined DT score (0-3) and a simplified way to communicate different severity levels of PSCs presented as four so-called disease health states: ‘no treatment required’, ‘mild’, ‘moderate’ and ‘severe’. The combined score of 0-3 can also be used to assess average scores for a cohort of subjects as in clinical trials when exploring the significance of different interventions.
The use of hierarchy scores is a well-established method also used in other disease areas such as acute coronary syndrome (Li et al, 2019), psoriasis (Monks et al, 2021), and care of hard-to-heal wounds (Letourneau and Jensen, 1998). The simplified use of severity categories for PSCs was inspired by the original OST, including four health states (normal skin, mild, moderate and severe). The validation of these health states was based on visual assessments of photos of peristomal skin by nurses and compared with a golden standard defined by an expert panel of dermatologists and highly experienced ostomy care nurses (Martins et al, 2010). This simplified representation of health states has been used to define treatment strategies and develop a health economic model to determine the health economic burden of PSCs (Meisner et al, 2012). The Skin Moisture Alert Reporting Tool (SMART) developed by Medicareplus (UK) is based on a similar simplified framework to be used by nurses to report moisture-associated skin damage at three severity levels: ‘mild’, ‘moderate’ and ‘severe’. Although the tool has not been validated, it was endorsed by the National Institute of Health and Care Excellence in December 2019 (Parnham et al, 2020).
The original OST is used by health professionals to assess the peristomal skin and, to a large extent, is based on visible complications—discolouration, erosion and tissue overgrowth.
In contrast, the advantage of OST 2.0 is that it also includes symptoms that, to a larger extent, are linked to the severity levels of PSCs and can be present without any visible signs. From the cross-sectional data set including 4209 participants assessing their peristomal skin using a modified version of the OST 2.0, 3706 had PSCs. Of those with a PSC, 1527 (41%) had sensation symptoms (pain, itching or burning) without any kind of visible signs such as broken compromised skin or discolouration; 185 had sensation symptoms to a level reported as severe (between 7 and 10). These numbers highlight the importance of being aware of any kind of PSC, visible or non-visible, as it may have important implications for how to treat or prevent PSCs going forward.
The data presented here were assessed with a modified version of the OST 2.0 tool using illustrations with different levels of discolouration, instead of the discolouration area being determined by the automated artificial intelligence method using pictures of the peristomal skin area. However, only 127 out of the 3706 self-reported PSCs ended up in the categories of having ‘only’ discoloured peristomal skin without broken skin or sensation symptoms. Of these, 90 had a discoloured area ≤10 cm2 categorised in the model as ‘no treatment required’. Based on these numbers from a large multinational survey, it is reasonable to suggest a modified use of the OST 2.0 if pictures of the peristomal skin are unavailable.
Conclusion
PSCs continue to be highly common conditions for people living with an ostomy. The OST 2.0 captures both visible and non-visible PSCs and is based on a PRO questionnaire and an objective method to assess the area of discolouration. For this reason, the tool can also be used by people with an ostomy to follow their peristomal skin condition closely and provide a common language to be used in dialogues with their health professional. This will enable a better opportunity for early interventions to prevent severe PSC.
KEY POINTS
- Not all peristomal skin complications (PSCs) are visible; it is equally important to assess and treat symptoms such as pain, itching and burning sensations
- The Ostomy Skin Tool 2.0 (OST 2.0) includes a patient-reported outcome questionnaire on symptoms and objective assessment of discolouration
- OST 2.0 provides a combined score that defines different severity levels of problems with peristomal skin
- The new tool enables changes in the peristomal skin to be followed on a regular basis
CPD reflective questions
- Do you find it challenging to capture changes in your patients' peristomal skin between consultations?
- Do you assess improvement in symptoms such as pain, itching and burning sensations?
- Do you assess the severity of problems with patients' peristomal skin?
- Would the use of the OST 2.0 impact on your treatment practice?


