Creation of an ostomy can be life saving for people with conditions such as colorectal cancer, bladder cancer, gynaecological cancer, inflammatory bowel disease, and diverticulitis (Burch et al, 2021). An ostomy is surgically created from the gastrointestinal or the urogenital tract to either temporarily or permanently exteriorise the colon or ileum to the skin and, in this way, provide a diversion for stool or urine (Colwell et al, 2019).
From a total population of approximately 27 million inhabitants in Denmark, Finland, Norway and Sweden (Nordic Co-operation, 2021) around 86 000 or 0.3% are estimated to live with an ostomy, and this number has increased gradually over at least the preceding decade (NORILCO, 2015; Blixt et al, 2017; Krogsgaard, 2020). In these countries, qualified stoma care nurses play a central role in promoting and supporting self-care among people with an ostomy.
The management of an ostomy involves the use of a product to collect output and consists of a baseplate adhering to the peristomal skin with a collecting bag attached. Most people with an ostomy have experienced leakage of output underneath the baseplate and on to the skin (Porrett et al, 2011; Claessens et al, 2015; Maydick-Youngberg, 2017; Jeppesen et al, 2022). Leakage and worry about it happening have severe emotional effects, as well as an impact on daily and social activities, such as the ability to work and participate in leisure activities, and it also affects motivation to leave home (Claessens et al, 2015; Nafees et al, 2018; Hedegaard et al, 2020; Jeppesen et al, 2022). Furthermore, when output comes in contact with the skin, peristomal skin complications may develop, which can be distressing for the individual (Fellows et al, 2021).
Improper fitting between the ostomy and the ostomy product(s) is one of the main reasons for leakage (James-Reid et al, 2019). People with an ostomy have very different peristomal body profiles, which may change during a lifetime (Colwell et al, 2019). This requires ostomy products designed to meet these different needs. In 2019, consensus-based best practice guidelines for standardising peristomal body profile assessment to enable quick and individualised solutions to improve quality of life of people living with an ostomy were developed with 2000 nurses (Colwell et al, 2019; James-Reid et al, 2019). As evident from the articles, where the guidelines are cited as ‘Consensus guidelines – standardising peristomal body profile assessment to enable quick and individualised solutions to improve quality of life', these focus on standardising peristomal body profile assessment in order to enable the quick and appropriate choice of optimal ostomy product(s). The use of the best-fitting ostomy product(s) is expected to reduce, or even prevent, the number of leakages, thereby increasing quality of life (Colwell et al, 2019; James-Reid et al, 2019; Hansen et al, 2022; Tonks et al, 2022).
The Peristomal Body Profile Assessment Tool (Body Assessment Tool) was developed by Coloplast in association with stoma care nurses from different countries across the world. It guides the selection of ostomy product(s) based on individual peristomal body profile (Colwell et al, 2019; James-Reid et al, 2019).
The aim of the study reported in this article was twofold: first, to investigate the clinical usability of the Body Assessment Tool among stoma care nurses, and, second, to evaluate whether a change to the best fitting ostomy product(s) had an impact on the number of leakages and related quality of life among individuals with an ostomy.
Methods
Study design
The study consisted of self-reported questionnaires conducted among stoma care nurses and individuals living with an ostomy It was carried out over 4–5 weeks and required that participants visited their stoma care clinic at the beginning of the study and that they returned questionnaires at start and end points of the study. Telephone calls to the stoma care nurses during the study period were optional and depended on the need for support.
Study populations
Nurse participants
In total, there were 22 respondents out of 43 invited stoma care nurses from Denmark, Finland, Norway and Sweden who had agreed to participate. Invitations were sent to stoma care nurses randomly selected from among those working in relatively large stoma care clinics. They were invited by the respective national Coloplast affiliate in each of the four countries.
Participants living with an ostomy
Between October 2020 and January 2022, individuals who reported leakage problems during regular follow-up at the stoma care clinic or who had contacted the clinic about leakage problems were informed about the study and asked whether they would like to take part. Individuals who were enrolled in the study signed an informed consent form after receiving verbal and written information about it. They were offered the option to say ‘no’ or to withdraw at any time during the study, without any effect on their care. Participants had to be at least 18 years old, living with an ostomy for at least 3 months and requiring re-evaluation of the ostomy product(s) in a stoma care clinic due to leakage issues. Individuals were excluded if they required a carer to change the ostomy product(s) or if they lacked mental capacity or physical ability to participate in the study. Women who were pregnant or lactating were also excluded as this may change body profile. Based on these criteria, 99 people were enrolled. However, data were withdrawn for 31 individuals due to missing data (12) and drop-out (19). The remaining 68 individuals (69% of those initially enrolled) constituted the study population.
Peristomal body profile assessment using the tool
At the initial visit to the stoma care clinic, the stoma care nurse performed a body profile assessment using the Body Assessment Tool developed by Coloplast with each participant. Assessment using the tool includes recording the form and texture of the peristomal area, as well as the position of the ostomy opening. The procedure was divided into six validated steps as described in the consensus guidelines (James-Reid et al, 2019):
- Step 1. Assess whether the shape of the area around the ostomy is regular, inward or outward
- Step 2. Assess whether shape around the ostomy is uniform or variable
- Step 3. Assess whether the area around the ostomy is soft or firm
- Step 4. Assess whether the skin around the ostomy has superficial creases or deep folds
- Step 5. Assess whether the ostomy is located above, at or below the bending line
- Step 6. Assess the position of the ostomy opening and the height of the ostomy.
Based on the results, the nurse selected the best-fitting ostomy product(s) for each participant, and they were instructed to use these devices throughout the entire study period. The study did not focus on specific brands, but on the type of ostomy product, such as pre-fixed or with bag attached to the baseplate (one-piece and two-piece products) and also the shape of the baseplate (flat, convex and concave). The nurse participants were trained by experienced stoma care nurses at workshops or webinars in the use of the tool before initiation of the study and they always had the option of contacting the teaching stoma care nurses for support. To increase the availability of the Body Assessment Tool, it is open access, not copyrighted, and no permission is needed to use it.
Evaluation of the tool
Nurses' feedback
The stoma care nurses evaluated the clinical usability of the Body Assessment Tool, which included answering the following questions:
- Does the tool offer value in clinical practice?
- Does it provide a good starting point when choosing ostomy product(s)?
- Does it help raise the quality of care?
Participants provided their responses on a 6 point-scale (1–6), where 1 indicated the lowest satisfaction and 6 the greatest satisfaction with the tool. The nurses were also asked to indicate whether they would recommend the use of the Body Assessment Tool to other stoma care nurses.
Responses of individuals living with an ostomy
Participants completed a questionnaire, which included eliciting demographics (age, sex, and country), ostomy type (colostomy, ileostomy, and urostomy), years since ostomy creation, and number of leakages in the preceding 7 days. Moreover, participants evaluated the impact and fear of having leakages on their everyday life using the Ostomy Leak Impact (OLI) tool. The OLI tool is a validated patient-reported tool used to assess the impact of leakage on quality of life among people with an ostomy, which is available to use free of charge (Nafees et al, 2018).
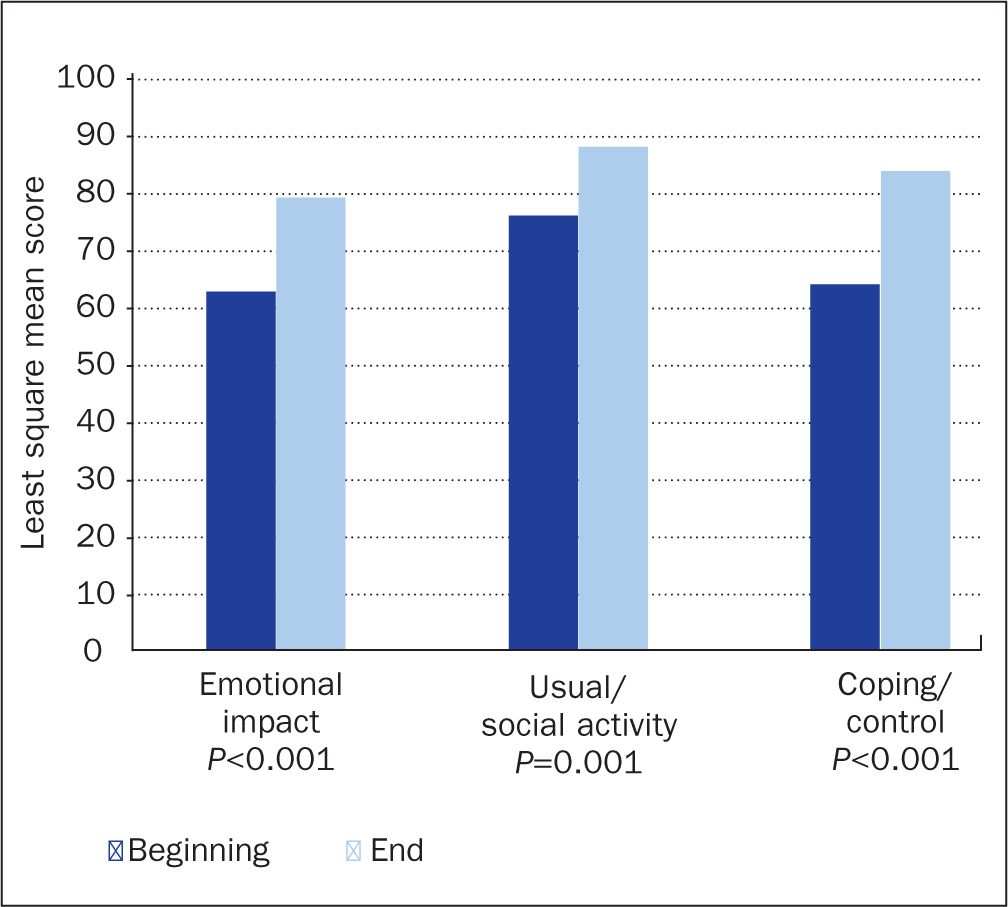
The OLI tool consists of 22 questions and generates scores within three domains:
- Emotional impact (10 questions)
- Usual and social activities (8 questions)
- Coping and control (4 questions).
The response to each question is rated on a 4-point Likert scale: ‘all of the time’, ‘often’, ‘sometimes’, and ‘rarely or never’. Because the domains contain a different number of questions, the score for each was transformed to the range of 0-100 to enable comparison across the three domains; the higher the score, the better level of leakage-related quality of life. The scores of the different domains cannot be calculated into a total score. At the end of the study, participants once again reported the number of leakages over the preceding 7 days and completed the OLI tool. Subgroups were created based on body profile, type of ostomy, sex and change of type of baseplate.
Statistics
The nurses' evaluation of the Body Assessment Tool was presented using descriptive statistical methods (mean and standard deviation (SD)). Categorical variables regarding baseline characteristics, results obtained using the tool, and type of ostomy product were described as absolute numbers and percentages of the study population. Domain scores and number of leakages were presented as least square (LS) means through the use of a mixed model, with ‘visit’ as fixed effect and ‘subject’ as random effect. A P value of <0.05 was considered statistically significant.
Ethics
All participating clinics and stoma care nurses signed a contract, and all participating individuals living with an ostomy signed an informed consent form after having received verbal and written information about the study. Ethical approvals were obtained from Finland and Norway, and correspondence with regulatory authorities in Sweden and Denmark revealed that ethical applications were not needed.
Results
Nurses' evaluation of the tool
Each nurse evaluated an average of four people living with an ostomy, ranging from one to nine: 5 nurses had 1-2 participants and 17 nurses had 3-8 participants. Overall, 21 out of the 22 nurses recommended the use of the Body Assessment Tool. The scores of the three statements regarding the usability of the tool in clinical practice were each close to or above 5 (Table 1).
Table 1. Evaluation of the clinical use of the Body Assessment Tool among the participating stoma care nurses (n=22)
| Number of participants with ostomy per nurse, mean (SD) | n=4.1 (2.3) |
| Evaluation of Body Assessment Tool | Mean (SD)* |
|---|---|
| Value in clinical practice | 4.6 (1.1) |
| Good as a starting point when choosing ostomy product(s) | 5.1 (0.8) |
| Helps raise quality of care | 4.7 (1.3) |
| Recommendation of the tool | |
| Yes | 21 (95.5%) |
Baseline characteristics of those living with an ostomy
The baseline characteristics of participants are presented in Table 2. The mean age was 67.8 years, and there was a female to male ratio of 60.6% to 39.4%; 47.8% had a colostomy, 37.3% an ileostomy and 14.9% a urostomy. The ostomy surgery had been performed on average 4.8 years prior to the study.
Table 2. Baseline characteristics of participants with an ostomy
| n (%) | |
|---|---|
| Age in years (n=58), mean (SD) | 67.8 (12.1) |
| Years since surgery (n=65), mean (SD) | 4.8 (10.5) |
| Country (n=68) | |
| Denmark | 29 (42.6%) |
| Finland | 12 (17.6%) |
| Norway | 19 (27.9%) |
| Sweden | 8 (11.8%) |
| Gender (n=66) | |
| Female | 40 (60.6%) |
| Male | 26 (39.4%) |
| Type of ostomy (n=67) | |
| Colostomy | 32 (47.8%) |
| Ileostomy | 25 (37.3%) |
| Urostomy | 10 (14.9%) |
| Consistency of output (n=64) | |
| Thick stool | 25 (39.1%) |
| Liquid stool | 29 (45.3%) |
| Urine | 10 (15.6%) |
SD=standard deviation
NB Missing data are not included in the calculation of proportions
Peristomal body profile
More than half the participants (50.8%) had a regular peristomal area (that is, level with the abdomen, although the skin surface may be uneven) (Table 3). About one quarter of participants (23.1%) had an inward peristomal area that sank into the abdomen creating a hollow, with about one quarter (26.2%) having an outward peristomal area that rose from the abdomen creating a peak.
Table 3. Body profile of participants at the beginning of the study
| Form of the area around the ostomy (n=65) | |
|---|---|
| Inward | 15 (23.1%) |
| Outward | 17 (26.2%) |
| Regular | 33 (50.8%) |
| Form being uniform or variable (n=66) | |
| Uniform | 30 (45.5%) |
| Variable | 36 (54.5%) |
| Form of the area around the ostomy and being uniform or variable (n=65) | |
| Inward uniform | 3 (4.6%) |
| Inward variable | 13 (20.0%) |
| Outward uniform | 11 (16.9%) |
| Outward variable | 5 (7.7%) |
| Regular uniform | 16 (24.6%) |
| Regular variable | 17 (26.2%) |
| Soft or firm abdomen (n=67) | |
| Firm | 14 (20.9%) |
| Soft | 53 (79.1%) |
| Superficial creases or deep folds (n=59) | |
| Deep folds | 13 (22.0%) |
| Superficial creases | 46 (78.0%) |
| Location of the ostomy (n=65) | |
| Above bending line | 9 (13.8%) |
| At bending line | 10 (15.4%) |
| Below bending line | 46 (70.8%) |
| Position of the ostomy opening (n=66) | |
| Above skin surface | 38 (57.6%) |
| Below skin surface | 6 (9.1%) |
| In level with skin surface | 22 (33.3%) |
NB Missing data are not included in the calculation of proportions
Furthermore, the consistency of the peristomal area was divided almost equally among participants, with 45.5% having a uniform area (consistent across the ostomy area) and the remainder had a variable area (not consistent across the ostomy area). Most had a soft abdomen (79.1%) as opposed to a firm abdomen. Deep folds of loose skin or excess fat in the ostomy area were reported for 22.0% of individuals, with the remainder having superficial creases, with lined, furrowed or wrinkled skin. Most participants had an ostomy located below the bending line (70.8%); 57.6% had the ostomy opening placed above the skin surface, 33.3% were level with the skin surface and 9.1% were below.
Ostomy product(s)
By the end of the study, the proportion of individuals who used a one-piece product increased from 53.0% to 70.1%, while the proportion of those using two-piece products fell from 47.0% to 29.9% (Table 4). Regarding the shape of baseplate, the proportion using a convex baseplate rose from 41.5% to 65.7%. This change was primarily due to less use of flat baseplates, which fell from 50.8% to 13.4%. The frequency of changes for one-piece and two-piece products decreased during the study: the percentage of individuals who changed their one-piece product every day increased from 44.4% to 66.7% (Table 4). However, the percentage of individuals who changed their one-piece product daily or less frequently rose from 55.6% to 80.0%. In the case of those using two-piece products, the percentage of those who changed the appliance every other day or less frequently increased from 58.6% to 70.6%.
Table 4. Type of ostomy product(s) used by participants at the beginning and the end of the study
| Beginning, n (%) | End, n (%) | |
|---|---|---|
| Pouching system | ||
| 1-piece product | 35 (53.0%) | 47 (70.1%) |
| 2-piece product | 31 (47.0%) | 20 (29.9%) |
| Shape of baseplate | ||
| Concave | 5 (7.7%) | 13 (19.4%) |
| Convex | 27 (41.5%) | 44 (65.7%) |
| Flat | 33 (50.8%) | 9 (13.4%) |
| Other | 0 (0.0%) | 1 (1.5%) |
| Frequency of change (1-piece) | ||
| Every other day | 4 (11.1%) | 6 (13.3%) |
| Every day | 16 (44.4%) | 30 (66.7%) |
| Twice a day | 8 (22.2%) | 4 (8.9%) |
| More than twice a day | 8 (22.2%) | 5 (11.1%) |
| Frequency of base plate change (2-piece) | ||
| Every other day or less | 17 (58.6%) | 12 (70.6%) |
| Every day | 5 (17.2%) | 4 (23.5%) |
| Twice a day | 6 (20.7%) | 0 (0.0%) |
| More than twice a day | 1 (3.4%) | 1 (5.9%) |
Missing data are not included in the calculation of proportions
Leakage and OLI score
The number of leakages declined significantly by 4.1 (mean difference) from 5.9 to 1.8 (LS mean at the beginning and end of the study) (Figure 1) across all populations of individuals living with an ostomy Concomitantly, the OLI score increased significantly by 17.9 (from 62.1 to 80.0 for emotional impact, 10.7 (78.5 to 89.2) for usual and social activities, and 16.2 (from 67.3 to 83.5) for coping and control.
All subgroups of individuals living with an ostomy (body profile, type of ostomy, type of baseplate, and sex) showed an identical pattern (Table 5). Of special interest were individuals with an inward body profile, and those who changed from using a flat to a convex baseplate.
Those with an inward body profile reported a high number of leakages in the 7 days preceding the start of the study, but there was a significant decrease of leakages during the study period, by a mean difference of 6.7. Concomitantly, the domains of the OLI tool, emotional impact and coping and control, increased significantly by a mean difference of 19.8 and 18.9 respectively, while usual and social activities increased non-significantly by 4.4.
Participants who changed from a flat baseplate to a convex appliance experienced many leakages and low OLI scores at the beginning of the study. However, substantial changes occurred during the period of the study: the number of leakages decreased significantly by a mean difference of 7.0 and the related OLI scores significantly increased for emotional impact, usual and social activity, and coping and control by 30.8, 17.5 and 28.8 respectively (Table 5).
Table 5. Leakages occurring in the preceding 7 days and OLI scores (0–100) at the start and end of the study for population subgroups
| Beginning LS mean | End LS mean | Mean difference | P value | |
|---|---|---|---|---|
| Body profile | ||||
| Regular body profile (n=34) | ||||
| Number of leakages | 5.5 | 2.4 | -3.1 | <0.001 |
| Emotional impact | 63.2 | 81.8 | 18.6 | <0.001 |
| Usual/social activity | 76.4 | 88.4 | 12.1 | 0.010 |
| Coping/control | 63.8 | 83.3 | 20.0 | <0.001 |
| Outward body profile (n=17) | ||||
| Number of leakages | 5.4 | 1.1 | -4.3 | <0.001 |
| Emotional impact | 64.5 | 80.4 | 15.9 | 0.010 |
| Usual/social activity | 75.3 | 84.6 | 9.2 | 0.173 |
| Coping/control | 74.5 | 83.3 | 8.8 | 0.273 |
| Inward body profile (n=15) | ||||
| Number of leakages | 8.3 | 1.6 | -6.7 | 0.001 |
| Emotional impact | 53.1 | 72.9 | 19.8 | 0.008 |
| Usual/social activity | 86.2 | 90.6 | 4.4 | 0.434 |
| Coping/control | 62.2 | 81.1 | 18.9 | 0.001 |
| Type of ostomy | ||||
| Colostomy (n=32) | ||||
| Number of leakages | 4.8 | 1.5 | -3.3 | <0.001 |
| Emotional impact | 69.7 | 86.8 | 17.1 | <0.001 |
| Usual/social activity | 79.8 | 91.9 | 12.1 | 0.033 |
| Coping/control | 75.8 | 93.2 | 17.4 | <0.001 |
| Ileostomy (n=26) | ||||
| Number of leakages | 6.7 | 2.5 | -4.2 | <0.001 |
| Emotional impact | 52.4 | 67.9 | 15.5 | 0.003 |
| Usual/social activity | 77.9 | 83.9 | 6.0 | 0.142 |
| Coping/control | 56.3 | 69.9 | 13.6 | 0.009 |
| Urostomy (n=10) | ||||
| Number of leakages | 7.4 | 0.9 | -6.5 | 0.019 |
| Emotional impact | 62.7 | 90.0 | 27.3 | 0.006 |
| Usual/social activity | 76.6 | 98.3 | 21.7 | 0.046 |
| Coping/control | 68.3 | 87.5 | 19.2 | 0.173 |
| Sex | ||||
| Female (n=39) | ||||
| Number of leakages | 5.8 | 2.1 | -3.7 | <0.001 |
| Emotional impact | 66.9 | 80.8 | 13.9 | <0.001 |
| Usual/social activity | 81.9 | 89.4 | 7.5 | 0.023 |
| Coping/control | 73.1 | 81.4 | 8.3 | 0.054 |
| Male (n=26) | ||||
| Number of leakages | 6.2 | 1.5 | -4.7 | <0.001 |
| Emotional impact | 55.5 | 79.7 | 24.2 | <0.001 |
| Usual/social activity | 76.4 | 91.5 | 15.1 | 0.019 |
| Coping/control | 59.9 | 86.9 | 27.0 | <0.001 |
| Type of baseplate | ||||
| Flat to convex (n=20) | ||||
| Number of leakages | 8.1 | 1.1 | -7.0 | <0.001 |
| Emotional impact | 58.2 | 89.0 | 30.8 | <0.001 |
| Usual/social activity | 75.5 | 93.0 | 17.5 | 0.011 |
| Coping/control | 60.4 | 89.2 | 28.8 | <0.001 |
| Any other pathway (n=48) | ||||
| Number of leakages | 5.0 | 2.1 | -2.9 | <0.001 |
| Emotional impact | 63.9 | 76.1 | 12.2 | <0.001 |
| Usual/social activity | 80.3 | 87.3 | 7.0 | 0.043 |
| Coping/control | 70.3 | 81.1 | 10.8 | 0.004 |
LS=least square; OLI=Ostomy Leak Impact tool
Discussion
The findings of this study have demonstrated a high degree of usability of the Body Assessment Tool in daily clinical practice in assisting the evaluation of the peristomal body profile of people with ostomy-related leakage issues, thereby providing guidance on the selection of the best-fitting ostomy product(s). The transition to using a more appropriate product with the aid of the tool resulted in significantly fewer leakages and an increase in leakage-related quality of life. This pattern was observed across body profile, type of ostomy, sex and with the change to using a different type of baseplate.
Motivated by the consensus practice guidelines on how to assess peristomal body profile (Colwell et al, 2019; James-Reid et al, 2019), a recent study highlighted the need for validated assessment tools (Martins et al, 2022). The Body Assessment Tool would appear to meet this requirement: 21 out of 22 nurses in this study recommended its use as a starting point when choosing ostomy product(s).
Leakage of stomal output has repeatedly been shown to be one of the most severe challenges for people with an ostomy (Richbourg et al, 2007; Claessens et al, 2015; Jansen et al, 2015). The Ostomy Life Study, which has been ongoing since 2015 and started with 4000 participants living with an ostomy in 11 countries (Claessens et al, 2015), expanded to 5000 participants across 17 countries in 2019 (Jeppesen et al, 2022). The studies found that worry about leakages remained consistently high over the years: in 2014, 91% of individuals living with an ostomy expressed concerns about this (Claessens et al, 2015), while in 2019 the figure was 92% (Jeppesen et al, 2022). Further results from the 2019 Ostomy Life Study illustrated that participants with daily leakage rated the OLI emotional impact domain at around 50, usual and social activities at 70, and coping and control at almost 60 (Jeppesen et al, 2022), indicating a low leakage-related quality of life. In contrast, when individuals experienced fewer leakages, domain scores increased significantly, terminating at never experiencing leakages with an emotional impact score above 80, usual and social activity of almost 90, and coping and control around 70, which indicated improved quality of life (Jeppesen et al, 2022).
Our study confirmed the level of domain scores in relation to frequency of leakages, as well as the increasing linear trend of leakage-related quality of life with decreasing frequency of leakages.
In addition to the psychological and social consequences of leakages, where stomal output is in contact with peristomal skin, there can be skin complications (Erwin-Toth et al, 2012; Colwell et al, 2022); this in turn will have a negative impact on a person's quality of life (Simmons et al, 2007; Nybaek and Jemec 2010; Porrett et al, 2011; Erwin-Toth et al, 2012; Colwell et al, 2019; Nichols et al, 2019). It is important that peristomal skin complications are treated, otherwise they may interfere with the adhesive on the baseplate, causing further leakage, which again leads to intractable peristomal skin complications (Nybaek and Jemec 2010). Thus, a primary guiding principle of stoma care is to achieve a secure adherence of the baseplate to reduce or eliminate the number of leakage-induced peristomal skin complications (Colwell et al, 2022; Hoeflok et al, 2013).
A recent study demonstrated that the risk of having output under the baseplate was significantly greater in respondents with creases and folds in the ostomy area (Martins et al, 2022). The study described in this article confirmed that deep creases and folds were indeed reasons for re-evaluation of an individual's ostomy product(s). The use of convex baseplates has been cited as the preferred technique to compensate for creases and deep folds around the ostomy because these baseplates have the ability to flatten folds and creases and facilitate ostomy protrusion above the skin, thereby allowing output into the collecting bag without contact with skin (Hoeflok et al, 2013; Carlsson et al, 2016; Perrin et al, 2021; Colwell et al, 2022). In one clinical trial (Kruse and Størling, 2015), a convex baseplate was shown to significantly reduce leakage incidents and also provided individuals with an increased feeling of security compared with a flat baseplate. The results of the study reported in this article are in agreement with these findings, with the largest improvements in the number of leakages and OLI scores occurring when participants switched from using a flat to a convex baseplate.
It has previously been shown that in individuals with an inward peristomal body profile there is a higher risk of leakage compared with individuals who have a regular peristomal body profile (Martins et al, 2022). There was a relatively high representation of participants with an inward peristomal body profile in our study (23.1%) compared with that in the Martins et al study (2022), in which 13% of participants had an inward peristomal body profile. In the study reported in this article, both the number of leakages and related quality of life improved with the right fitting ostomy product(s) for participants with an inward peristomal body profile.
If the ostomy product(s) do not fit well, individuals living with an ostomy will often mitigate the risk of leakage and peristomal skin complications by, for example, changing or adding ostomy products (Meisner et al, 2012; Nichols et al, 2019; Jeppesen et al, 2022). Our results confirmed this, because participants had previously changed their ostomy product(s) more often before they changed to an optimally fitting solution. Similarly, more than half the participants in the Ostomy Life Study who worried about leakage changed their appliance often and/or used more supporting products, such as powder, rings, seals, paste, tape and belt, compared with participants who did not worry about leakage (Jeppesen et al, 2022).
Without a peristomal body assessment tool, the identification of the best ostomy product(s) for a particular individual might be done following many iterations, which will require several visits with a stoma care nurse (Martins et al, 2012; Meisner et al, 2012; Tonks et al, 2022). Thus, choosing ostomy product(s) that are the best fit to an individual's peristomal body profile not only benefits them, but is also cost-effective (Martins et al, 2012; Meisner et al, 2012; Taneja et al, 2017; Taneja et al, 2019; Tonks et al, 2022). This is in the context of the fact that 37% of participants in Martins et al's (2022) study had never consulted their stoma care nurse regarding choice of ostomy product(s), and 22% of people with ostomy across five European countries were unaware of the possibility to consult a stoma care nurse (Krogsgaard et al, 2022). There seems to be a need to increase the awareness of the possibility to consult a stoma care nurse. Furthermore, contours around the ostomy transform as users age or body weight changes (Colwell et al, 2019), which highlights a vast need to regularly re-evaluate the current ostomy product(s) based on assessment of the peristomal body profile. This is supported by our results, which illustrated that following a visit to the stoma care nurse and an assessment of peristomal body profile, several individuals were able to change their ostomy products to those with a better fitting, resulting in significantly fewer leakages and a significant improvement in quality of life.
An important strength of the authors' study is that the analyses were based on outcomes reported by those living with an ostomy themselves, providing a direct insight into their experiences, and that a validated tool (OLI) was used in the self-reported questionnaires.
Limitations
A methodological limitation of the study was the fact that 19 of the 99 individuals living with an ostomy initially enrolled dropped out during the course of the study. Data on reasons for this were not collected, so it is not possible to establish whether there was any selection bias. Due to the COVID-19 pandemic it was not possible to enrol 160 participants as had originally been planned. However, it seems unlikely that this would have changed the results substantially. Information regarding the use of supporting ostomy products was not part of the study although it could have contributed to nuance the findings.
Analyses of the findings of the nurses' responses may have been more robust had they had been weighted towards nurses with greater caseloads, ie towards median caseload, who would have had more interactions with patients. Nonetheless, the authors consider that the results of the study are still valid.
It is worth noting that because the study took place during the pandemic the small nursing caseloads would be attributable to this fact.
Conclusion
This study supported the use of the Body Assessment Tool, devised by Coloplast, in clinical practice as a starting point for nurses to make an objective assessment of an individual's peristomal body profile. This supports nurses in selecting the best ostomy product(s) for particular individuals experiencing leakage issues. Moreover, the study showed that the best-fitting ostomy product(s) led to a significant reduction in the number of leakages and an improvement in quality of life.
Peristomal body profile changes over a person's lifetime, so the next step could be to undertake an evaluation of whether the tool could be useful as an integral part of regular follow-up visits at stoma care clinics. This would ensure that the current ostomy product(s) selected for an individual are always an optimal fitting appliance.
KEY POINTS
- People with an ostomy have very different peristomal body profiles and an improper fitting between the ostomy area and the ostomy product(s) is one reason for leakage
- Stoma care nurses who took part in the study highly recommended the Body Assessment Tool as an objectively measure of peristomal body profile that offers a first step toward choosing the best-fitting ostomy product(s)
- Optimally fitting of ostomy product(s) reduced the number of leakages and increased the leakage-related quality of life
CPD reflective questions
- How do you currently select the most appropriate ostomy product(s) for your patients?
- Reflect on the strengths and weaknesses of using a tool to measure a patient's peristomal body profile objectively in order to guide the choice of ostomy product(s)
- Why do you think it is beneficial to regularly check the fitting between the ostomy area and the ostomy product(s)?


