The human body is made of elements including hydrogen, oxygen, carbon, calcium and phosphorus. These elements are found within all cells in the human body (Feather et al, 2020). The human body contains trillions of cells, these cells are the body's smallest functional components and are a fundamental unit of life (Peate, 2020). When cells are grouped together, tissues are formed, each with a specific function, such as blood and muscle. When different tissues are combined, organs are formed, for example, heart and brain. Organs are grouped together to form systems that support the function of the human body (Waugh and Grant, 2018). An example would be the integumentary system, which consists of the skin, hair, nails, and exocrine glands. The integumentary system is the largest organ of the human body and forms a physical barrier between the external environment and the internal environment that it serves to protect and maintain (Tortora and Derrickson, 2017).
However, the above arrangement of cells and tissues to form complex bodily systems owe their existence to a single cell, called the zygote. The zygote results from the synthesis of the female egg cell (ovum) and the male sex cell (spermatozoon). Cell division then follows, the foetus grows, and cells with different structural and functional specialisations then develop, all with the same genetic make-up as the zygote (Colbert et al, 2019).
The cell: structure and function
This article outlines the basic structure and functions of cells and tissues; it is not intended to replace a biology textbook, which will provide more detail. Figure 1 illustrates a simple cell.
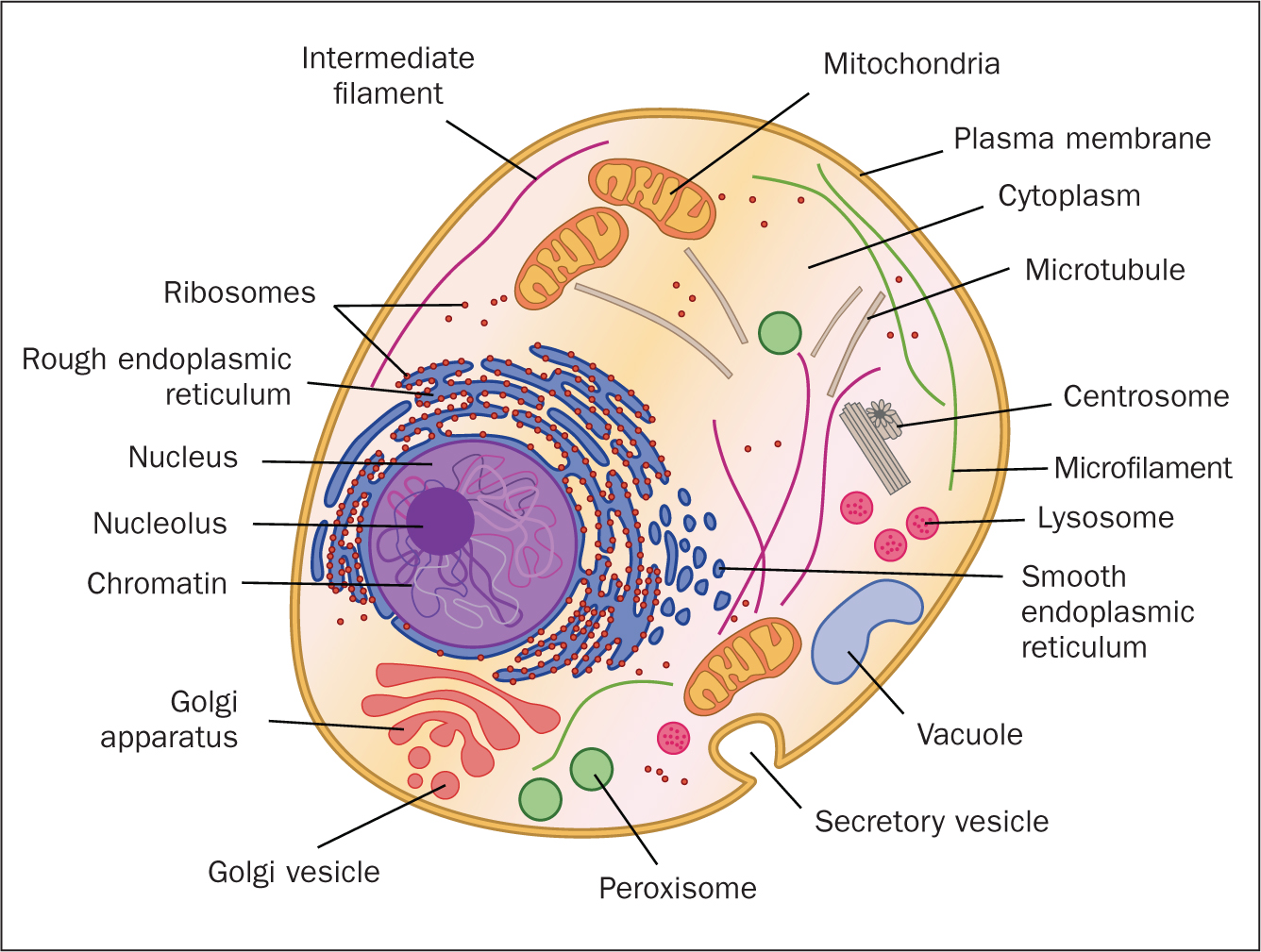
Plasma membrane
Plasma membranes control the passage of substances into and out of cells and therefore the structure and function of the membrane and is vital for cell survival (Waugh and Grant, 2018). The membrane is made up of a bilayer of phospholipids, which are surrounded by proteins and sugars. The phospholipids have a hydrophilic (water-loving) head and hydrophobic (water-hating) tails. The phospholipid bilayer is constructed in such a way that the hydrophilic heads are aligned on the outer surface of the plasma membrane and the hydrophobic tails on the inside (Peate, 2020).
This structure enables the movement of water-soluble materials (oxygen and carbon dioxide, glucose), lipid-soluble materials (sodium, potassium, calcium) and other substances (including amino acids) across the membrane via passive transport, diffusion, and active transport (Colbert et al, 2019).
Cytoplasm
The plasma membrane surrounds the cytoplasm. The cytoplasm consists of cytosol, which is a viscous fluid that fills the inside of the cell. Organelles (see Figure 1) are suspended within in the cytosol, each of which have specialised functions; they include the nucleus, mitochondria, ribosomes, endoplasmic reticulum, golgi apparatus, lysosomes and cytoskeleton (Tortora and Derrickson, 2017).
Nucleus
The nucleus contains chromosomes made of deoxyribonucleic acid (DNA), which is the body's genetic material. Each chromosome consists of many genes. The nucleus protects these genes and controls cellular activity within the cell (Peate, 2020).
Mitochondria
The mitochondria are the ‘powerhouse’ of the cell. They are fundamental to aerobic respiration, the process by which chemical energy in the form of adenosine triphosphate (ATP) is made available. ATP fuels the cell and is involved in other cellular processes, such as cell division, growth and cell death (Colbert et al, 2019; Peate, 2020).
Ribosomes
Ribosomes are small granules made up of ribonucleic acid (RNA) and protein. Ribosomes are essential in the synthesis of amino acids. Ribosomes also make proteins for use within the cell and produce enzymes that support metabolic activity within the cell (Tortora and Derrickson, 2017; Waugh and Grant, 2018).
The cell cycle
The growth and function of cells (interphase) are closely regulated to ensure a balance between cell growth and cell death (apoptosis). Cell division or mitosis is imperative for growth and tissue repair. When cells increase in number through mitotic division this is referred to as cell proliferation (Cook et al, 2019). When proliferating cells (dividing cells) are transformed into specialised cell types, this is referred to as cell differentiation. Both cell proliferation and cell differentiation are regulated by growth factors that maintain the balance between replacing damaged cells and inhibiting the growth of undesirable cells (McCance and Huether, 2018). Flaws in this process can initiate the proliferation of new cells that can be benign or malignant tumours (neoplasia).
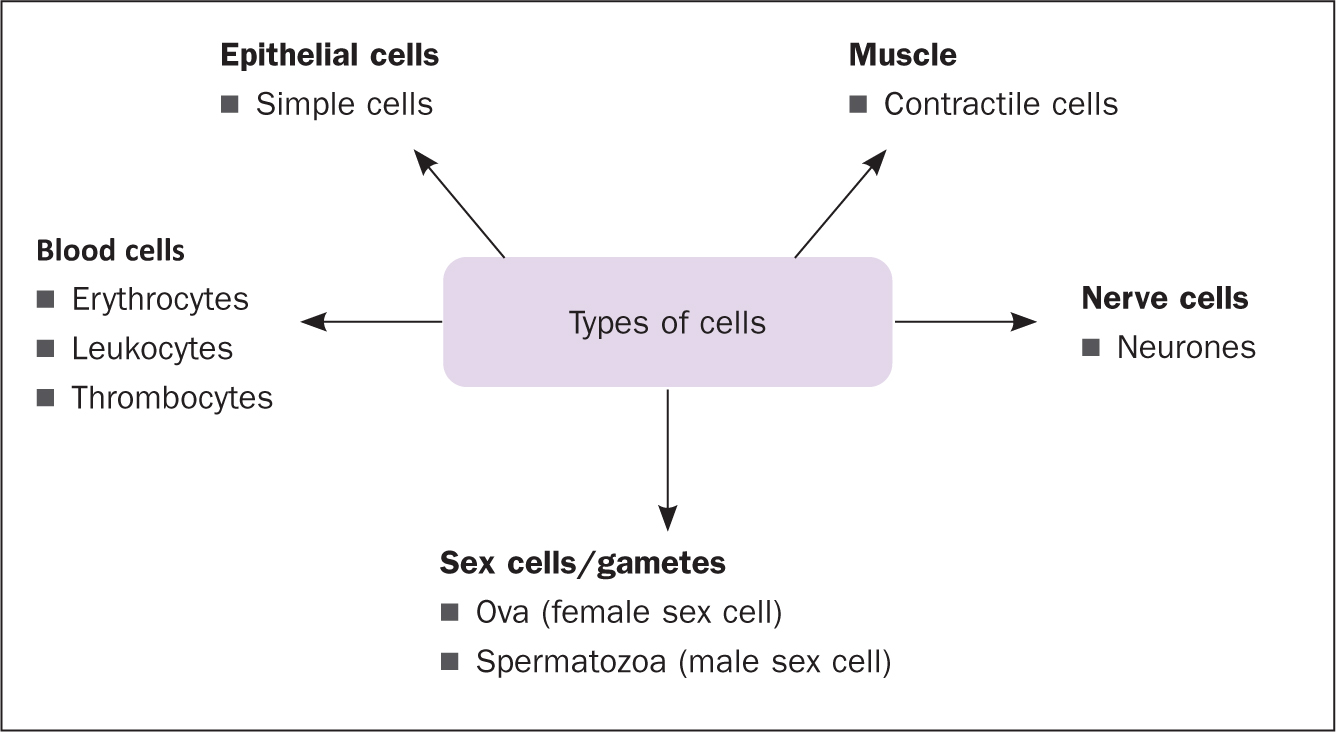
Mitosis is a continuous process involving four distinct stages: prophase, metaphase, anaphase and telophase. Human cells with nuclei have 46 chromosomes; the process of mitosis divides these chromosomes into two new genetically identical daughter cells (Colbert et al, 2019). This process should not be confused with meiosis, which forms gametes (sex cells), ie ova and spermatozoa (Waugh and Grant, 2018). See Figure 2 for the types of cells found in the human body.
Tissues
Tissues are composed of many of the same type of cells and are identified according to their size, shape, and function (Carlson, 2019). There are four main types of tissue, each with a specialised structure and function, as outlined in Figure 3 and Table 1.
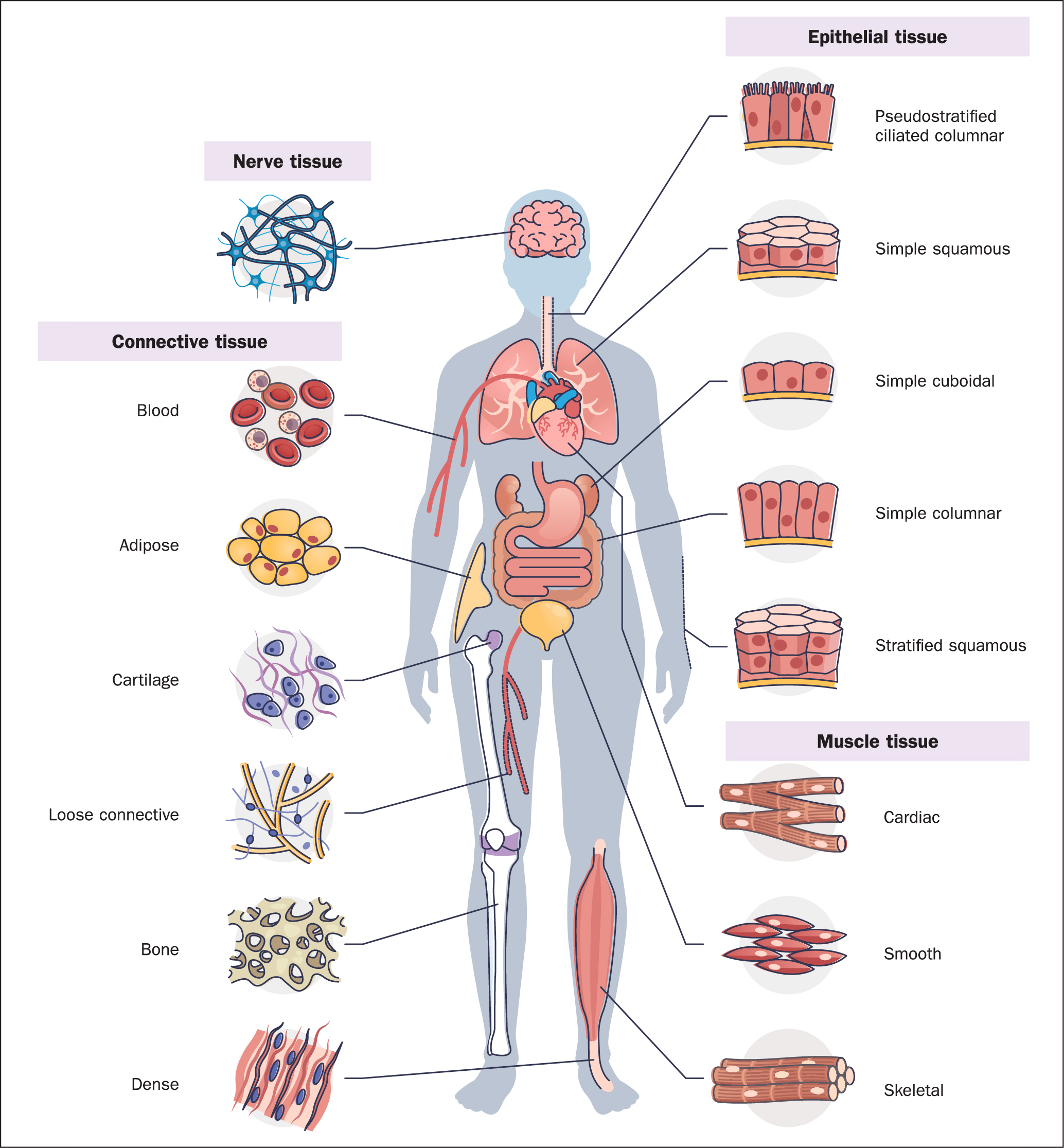
Table 1. Tissue types
| Type of tissue | Structure | Function |
|---|---|---|
Epithelial
|
Simple – single layer of cellsStratified – several layers of cells | Covers the body and form the lining of cavities. Supports protection, secretion, absorption |
Muscle
|
Skeletal – striated and voluntarySmooth – non-striated, visceral – involuntaryCardiac – only found in heart wall – involuntary, cross stripes (striations) | Able to contract and relax, providing movement of the human body |
Connective
|
Connective tissues consist of cells and a matrix, which contains fibres and ground substance |
|
Nervous
|
Neurones – nerve cells consist of a cell body, one axon and multiple dendritesNeuroglia – a connective tissue that supports neurones | Generate and transmit nerve impulses (action potentials) |
Cell and body tissue pathophysiology
Variation in cell size and quantity
It is important to appraise how normal cell and tissue physiology can be affected by physiological and/or pathological deviations (Cook et al, 2019). Examples of this include hypertrophy, atrophy, and hyperplasia.
Hypertrophy, or enlargement of cells, can be a result of physical exercise, whereby the tone or bulk of muscle tissues is increased. Atrophy occurs when there is a decrease in the number of cells, leading to a decrease in the size of an organ or bodily structure. Atrophy can happen if muscle fibres are not engaged, which leads to reduced muscle mass (Satori et al, 2021). Mutations in the cell's DNA can also cause atrophy, preventing cells from functioning normally (Schwartz et al, 2019). Causes of atrophy may include:
- Genetic mutations within cells that prevent normal activity
- Reduced mobility, for example, from a physical accident
- Lack of nutritional supply
- Reduced blood supply
- Altered endocrine stimulation
- Denervation, which is an altered nerve supply to the organ concerned.
Hyperplasia is where cell division occurs too rapidly and cell quantity increases within the tissue or organ. This is a normal process in the physiology of the glandular milk-producing tissue of the breast, which enlarges during pregnancy and breastfeeding (Waugh and Grant, 2018). Abnormal hyperplasia due to pathophysiological changes can lead to the development of ‘new growths’ or neoplasms, which can be benign or malignant (Cook et al, 2019; Dehn and Asprey, 2020).
Cell death
Apoptosis or cell death is the normal process of death at the end of the cell cycle for an ageing cell. The cell shrinks and the process of phagocytosis eliminates the cell to maintain tissue homeostasis.
Necrosis is the death of cells due to a lack of oxygen (hypoxia), either from an accident or a pathological development such as infectious agents or extreme environmental conditions (Krysko et al, 2008). Treatment for necrosis caused by a microorganism is normally via antibiotics and surgery, although larval therapy has been found to be successful in the management of necrotic wounds (Cutterridge and Bera, 2021). Classifying the microorganism is important to identify the antibiotic required to eradicate the microorganism (Tortora and Derrickson, 2017). Surgery can involve the draining of an abscess or the debridement of dead, damaged, infected tissue. In severe cases, amputation may be required (Cook et al, 2019).
Neoplasms (tumorigenesis)
When tissues grow in an uncoordinated way and faster than normal, and the stimulus to stop growth has been interrupted, this can lead to a tumour (neoplasm). Tumours are defined as either benign or malignant, see Table 2.
Table 2. Tumour classification
| Characteristics | Benign | Malignant |
|---|---|---|
| Structure | Structure is typical of origin | Structure is often atypical |
| Growth | Growth does not affect normal tissue and is normally slow | Growth is often rapid and not confined. Expansion often penetrates surrounding tissues |
| Metastasis | Never | Generally, yes – if not treated |
Aetiology of neoplasms
Chemical carcinogens
Scenario 1:
Gary is a 68-year-old male who has been complaining of shortness of breath, haemoptysis (coughing blood), weight loss and fatigue. He has smoked 30-40 cigarettes a day since he was 16 years old and has no intention of giving up.
Chemical carcinogens are diverse in structure and function and include both natural and synthetic substances (Bradley et al, 2021). Carcinogens can permanently damage the DNA of cells or alter cellular metabolism – this interferes with biological processes within the cell. Uncontrolled mitosis leads to malignant cellular division and the proliferation of tumours (Klaunig, 2020).
The amount of a carcinogen required to do this is not easily quantifiable, however, it is suggested that exposure to a carcinogen that is repeated over time could have a cumulative effect, leading to malignancy (Calabrese et al, 2021). Examples of carcinogens include aniline dyes, asbestosis, radon and – as in the case of Gary – cigarette smoke. For a full list of potential carcinogens see the website of the American Cancer Society (2019).
Smoking tobacco accounts for more than 8 million deaths each year and is the single greatest cause of preventable death globally (World Health Organization, 2022a). Tobacco smoke contains more than 70 chemicals that can cause cancer. Furthermore, smoking leads to diseases of the heart, liver, and lungs. Smoking increases the risk of pneumonia, myocardial infarcts, strokes, and peripheral disease (Jha and Peto, 2014). Smoking causes irreversible damage of the lungs as seen in patients who have chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema (NHS website, 2019).
Gary is showing signs and symptoms of a progressive disease. It is likely that he has lung cancer, and that it is advanced due to the weight loss and fatigue. Haemoptysis related to malignancy is common. Gary's signs and symptoms should be investigated under the 2-week rule for suspected lung cancer or pleural cancer because he meets one of the two criteria defined by the National Institute for Health and Care Excellence (NICE) (2021a; 2021b):
- Have chest X-ray findings that suggest lung cancer
- Are aged 40 years and over, with unexplained haemoptysis.
Ionising radiation
Scenario 2:
Martha is a 36-year-old female who runs a successful sunbed business. She admits to using the sunbeds herself at least three times a week. Martha has reported to her GP with a pigmented nodule on her back that has increased in size. She tells her GP that the lesion has been present for over 3 months, but she has been too scared to visit her GP.
Exposure to ionising radiation can lead to malignant changes in some cells and can even directly kill cells (radiotherapy). It is during mitosis that cells are affected, with cells that undergo frequent division being most susceptible, for example:
- Skin
- Bone marrow
- Sex cells – ovaries/testes.
A common example as seen in scenario 2 is repeated exposure to ultraviolet (UV) rays due to sunburn or sunbeds. It is possible that Martha has developed skin cancer. As explained by Cancer Research UK (2020), there are two main types of skin cancer: non-melanoma skin cancer (including basal cell and squamous-skin cancer) and melanoma skin cancer. Melanomas start in the skin cells called melanocytes, which between the epidermis and basal cell layer. Melanocytes produce the skin pigment called melanin, which is responsible for protecting the body from UV radiation. UV radiation can cause sunburn; constant exposure to unnecessary amounts of UV radiation can over time damage DNA in the skin cells and lead to cancer.
Martha should be reviewed by a specialist under the ‘2-week rule’ because her lesion is suggestive of malignant melanoma ie it is nodular and is pigmented in appearance (NICE, 2017; 2021a). The clinical knowledge summary available on the NICE website discusses in more detail the management of suspected melanoma (https://tinyurl.com/2p99pb6m).
Oncogenic viruses
Scenario 3:
Jana is a 40-year-old research scientist living in London. She has attended her GP as she has found a lump in her right breast. Breast cancer is very common in her family. Jana also has a complaint of pain during sex and has lower back (pelvic) pain. She has been attending her GP for frequent urinary infections. Her medical history also includes a diagnosis of human papilloma virus (HPV), which has not been monitored since diagnosis 15 years ago. Jana gets a good amount of exercise, eats healthy foods and has never smoked.
Some malignancies can be caused by viruses that invade and inject their DNA or RNA into the genetic material of the host cell. This can cause a mutation and subsequent malignancy. Such viruses include the hepatitis B virus, which can cause liver cancer, or HPV, which is linked to 90% of cervical cancer cases (Krump and You, 2018).
Jana's GP suggests a mammogram for suspected breast cancer. Jana admits that there is a history of breast cancer in the family. However, the GP also has concerns regarding the symptoms of pelvic pain and painful intercourse, alongside her age group and diagnosis of HPV. The GP notes that Jana has not had a cervical screen since diagnosis of the HPV 15 years previously and suspects cervical cancer (NICE, 2021a; 2022).
Early detection and removal of abnormal tissue is imperative before it becomes malignant (Waugh and Grant, 2018). Cervical cancer develops over a period of 15–20 years in women with a normal immune system (WHO, 2022b). According to Cancer Research UK (2021) the peak age of cervical cancer incidence in women in the UK is 30-34 years.
The extent of cervical cancer is classified in stages (Waugh and Grant, 2018):
- Stage I represents disease that is confined to the cervix
- Stages II–IV represent increased spread, involvement of bladder, rectum, and tissues outside of the pelvis. In the late stages, metastases can be found in liver, bones and lungs.
Similarly to Gary and Martha's scenarios, Jana also meets the criteria for investigation under the 2-week rule for breast/cervical cancer (NICE, 2022).
Host factors
Scenario 3 highlighted that breast cancer is common in Jana's family, and this is relevant to the finding of a lump in her breast. It is possible that Jana's individual characteristics – her inherited genetic factors – could have predisposed her to developing breast cancer. This is referred to as a host factor, a category that also includes a person's race and increasing age. Some of these host factors can be modified by the individual's behaviour, leading to proliferation of neoplastic cells, such as cigarette smoke or repeated episodes of UV exposure as seen in Gary's and Martha's scenarios (Waugh and Grant, 2018; American Cancer Society, 2019; Cook et al, 2019).
Conclusion
The human body contains trillions of cells – the cells are the body's smallest functional components and are the fundamental unit of life. Cells group together to form tissues and organs within complex bodily systems. The cell cycle is both complex and essential to life, however, mutations in cell genesis can lead to the proliferation of cancer cells and, ultimately, the demise of the host. It is important to have an awareness of the aetiology and the clinical scenarios outlined in the article provide context for the signs and symptoms of tumorigenesis.
KEY POINTS
- When cells are grouped together, tissues are formed, each with a specified function (eg blood or muscle). When different tissues are combined, organs are formed (eg heart or brain). Organs are grouped together to form systems that support the function of the human body
- The growth and function of cells are closely regulated to ensure a balance between cell growth and cell death. Cell division or mitosis is imperative for growth and tissue repair, but uncontrolled growth can lead to neoplasms (tumours)
- Neoplasms can be caused by chemical carcinogens, oncogenic viruses, ionising radiation, and host factors, which includes genetics and health behaviours
CPD reflective questions
- What is the main structural difference between a tissue and an organ?
- What is the difference between hypertrophy and atrophy?
- Can you name at least one example of these four potential causes of neoplasms: chemical carcinogenic, ionising radiation, oncogenic virus, host factors


