Cardiorespiratory arrest is uncommon in children and therefore nurses are unlikely to be involved in the practice of paediatric basic life support (BLS) (Bardai et al, 2011; Maconochie et al, 2015). Nonetheless, knowledge and skills in providing paediatric BLS remain essential, particularly given that the Nursing and Midwifery Council (NMC) standards of proficiency state:
‘All registered nurses must demonstrate the knowledge, skills and confidence to provide first aid procedures and basic life support.’
This article has used the Resuscitation Council UK (RCUK, 2015) evidence-based guidelines to discuss the practice of paediatric BLS as a way of updating practitioners.
The majority of cardiorespiratory arrests in children and infants are a result of respiratory insufficiency rather than cardiac problems (Cocks, 2006). Children and infants are at risk of becoming respiratory compromised and experiencing subsequent hypoxia for a number of reasons including birth asphyxia, inhalation of foreign bodies, bronchiolitis, asthma, convulsions, or neurological damage. Therefore, the order of delivering resuscitation differs between paediatrics and adults. In unresponsive adults, chest compressions should be performed before rescue breaths. In infants and children, respiratory insufficiency will subsequently cause cardiac arrest. Therefore, it is imperative that air, or where possible oxygen, is administered immediately through assisted breathing. The sequence for paediatric BLS follows a systematic approach: airway (A), breathing (B) and circulation (C).
It is important to note that different approaches are required between infants and children when delivering BLS. When providing BLS, an infant is a baby under 1 year of age and a child is 1 year of age until puberty (RCUK, 2015). Once a child visibly appears to reach the stage of puberty then the rescuer must follow the adult BLS sequence as described by Barker (2019). The RCUK (2015) recognise that rescuers may only know the adult algorithm and advise that using this sequence is better than not performing any cardiopulmonary resuscitation (CPR). However, nurses who practise according to the NMC Code (2018b) must follow best practice guidelines and age-specific BLS. Recognising a paediatric emergency is crucial; however, recognising and preventing deterioration is paramount to prevent death (Pearson, 2008) and will be discussed in future articles.
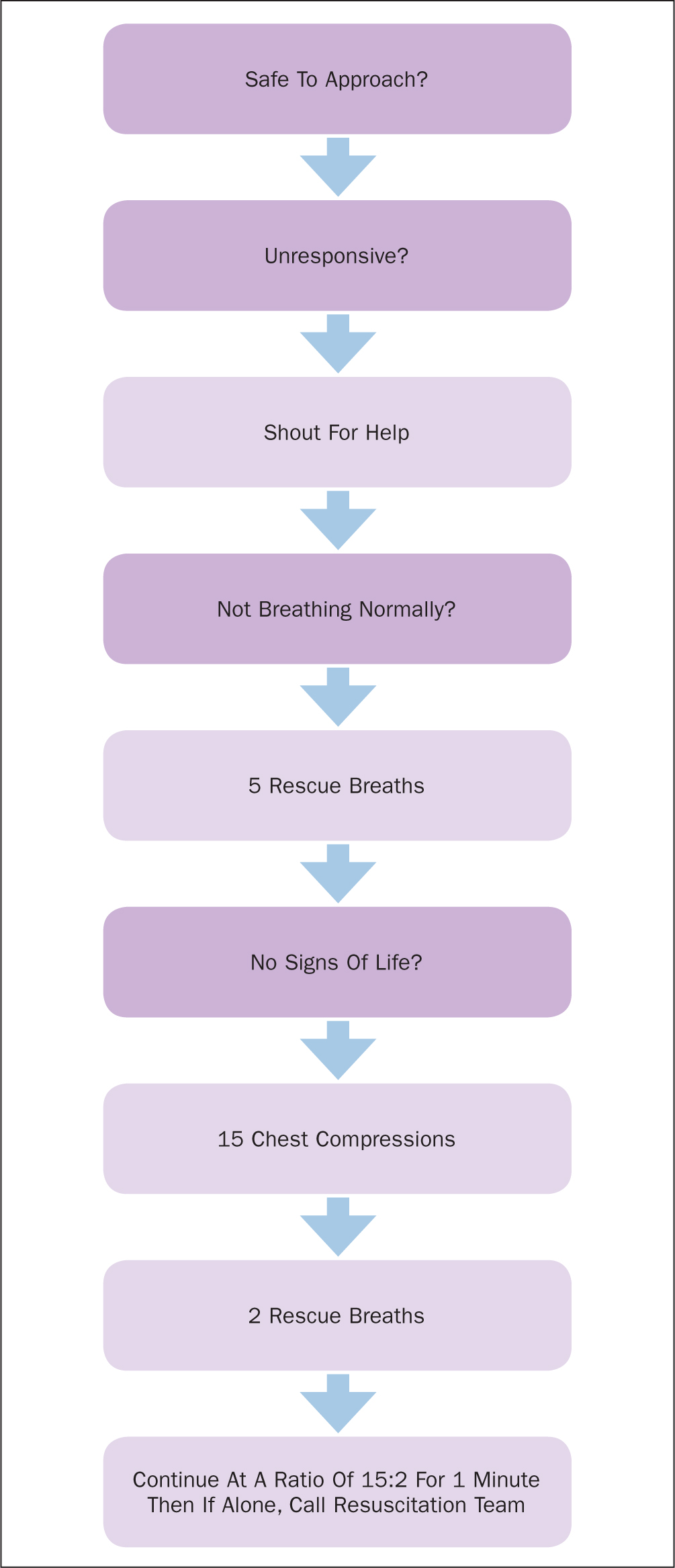
SAFE approach
Within an emergency, the rescuer must use the SAFE approach: Shout for help, Approach with care, check if the area is Free from danger, and then Evaluate the patient using ABC (Cocks, 2006). Following the SAFE approach, an initial assessment of responsiveness and a check for signs of life is required. To ascertain this, the rescuer should talk loudly to the child/infant to assess responsiveness, followed by gently stimulating the child/infant—shaking a shoulder for a child or tickling a foot for an infant. Signs of life may be assessed through considering if there is any movement, coughing or normal breathing but should not include abnormal gasps or infrequent, irregular breaths (RCUK, 2015).
If the child/infant is responsive, this demonstrates that they do not require CPR. If the cause of the collapse is unknown, or the injury requires further treatment, the rescuer should leave them in the position they found them and remain with them. Until help arrives the rescuer should regularly reassess the child/infant's condition. If the child/infant is unresponsive, the rescuer should again shout for help and begin the ABC approach. In a hospital emergency, the paediatric resuscitation team should be called and, in the community, rescuers should call 999.
Airway
Before the rescuer can assess the child/infant's breathing, they must first ensure the airway is open. The child/infant should be on their back and the rescuer should ensure an open airway. One hand should be placed on the child/infant's forehead while the fingertips of the other hand are placed under the point of the child/infants' chin and the head should be gently tilted and the chin lifted at the same time. This manoeuvre is referred to as the head tilt-chin lift, its purpose is to prevent the tongue obstructing the upper airway. At this point, the rescuer must visually check the patency of the airway; airway obstruction may be the primary problem. If an obstruction is visible and it is possible to remove this without passing the teeth/gum line, then the rescuer should do so. The rescuer should not blindly sweep their fingers inside the mouth in search of an obstruction.
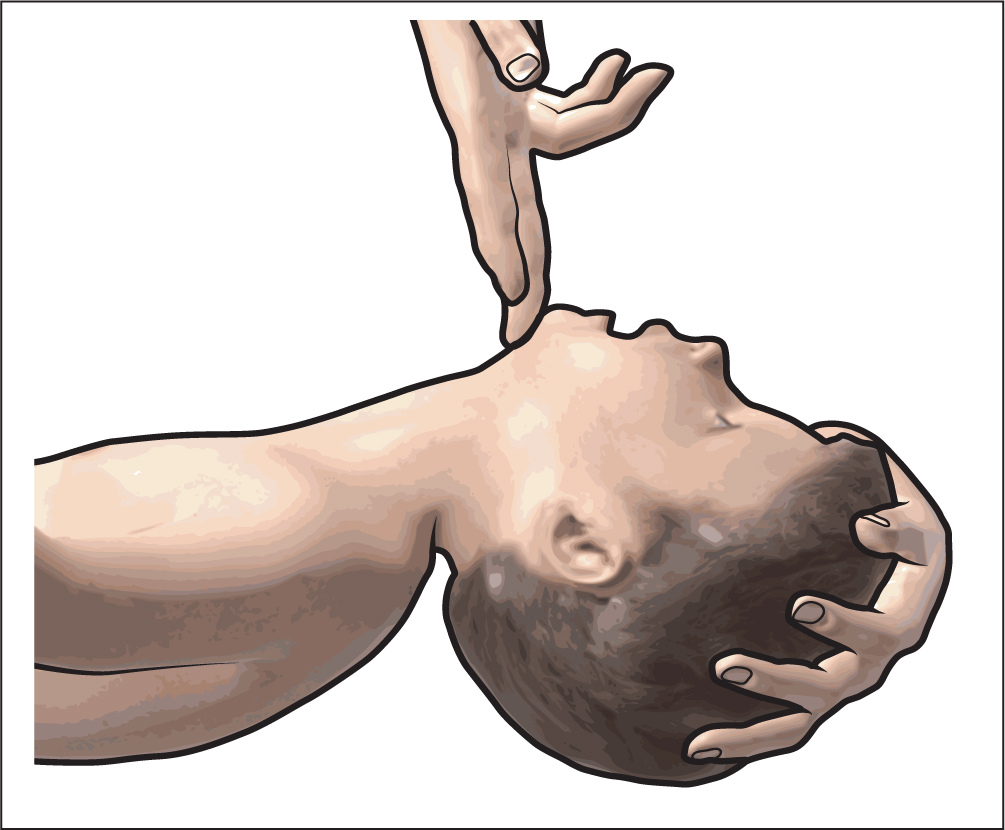
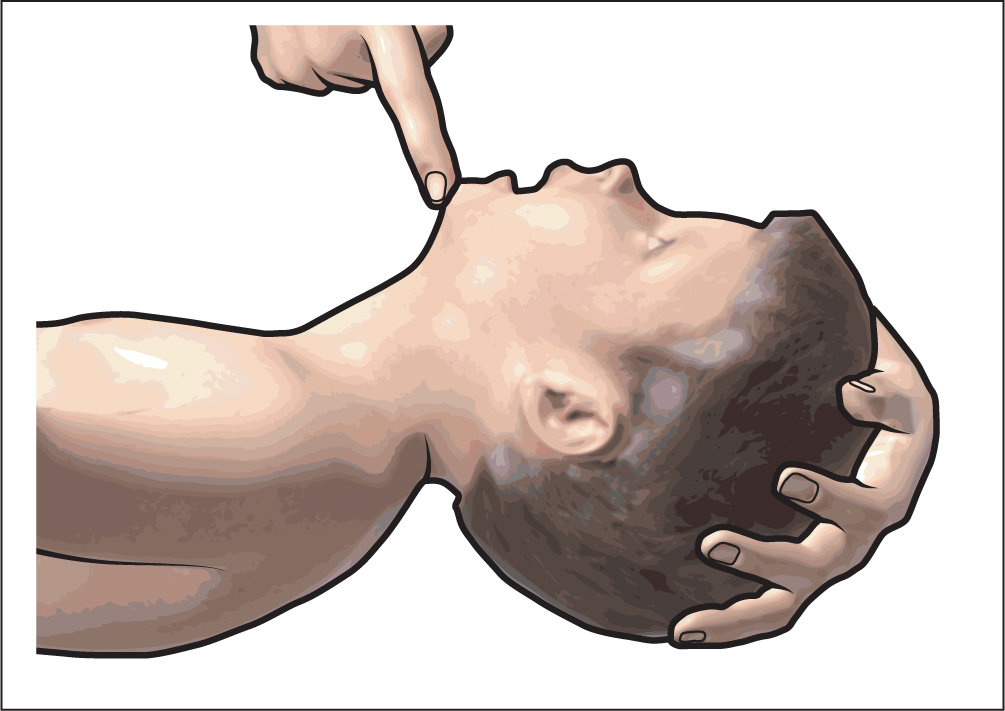
In children the position for opening an airway is sometimes referred to as ‘sniffing the morning air’ (Figure 1), where the nose is pointed up as if the child were sniffing. This position is used as the anatomy of a child requires that the three axes—oral, pharyngeal and tracheal—are in this position to maximise airway patency (Greenland et al, 2008). In infants, the head needs to be in a ‘neutral’ position (Figure 2) to achieve airway patency, whereby the infant is looking directly forwards. Over extension of the infant's neck will lead to excessive flexion due to the presence of a prominent occiput and will therefore obstruct the airway (Cocks, 2006).
If a child/infant has a suspected neck injury, it is possible to open the airway using the jaw thrust method to prevent further damage to the neck. This is achieved by placing the first two fingers of each hand behind each side of the child's jaw and pushing the jaw forwards (Figure 3).

Breathing
Once the child or infant's airway is open the rescuer should look, listen and feel for signs of breathing by placing their face close to the child/infant's chest and looking down the chest. The rescuer should look for respiratory activity while listening for noise from the mouth or nose and feeling for breath on their cheek. Assessment of breathing should take 10 seconds. If the child/infant is breathing normally, they should be placed in the recovery position until help arrives, ensuring that the airway is patent (Figure 4). Regular assessment for deterioration must be undertaken. If the child/infant is not breathing normally, five initial rescue breaths should be delivered.

Rescue breaths in children are delivered by pinching the soft part of the nose closed, taking a breath and then placing the lips around the child's mouth to form a seal and blowing steadily into the mouth over the course of one second to make the chest rise (Figure 5). The rescuer should remove their mouth from the child's mouth and watch the chest fall, before repeating the process four more times.

In infants, rescue breaths are delivered through the rescuer placing their mouth over the infant's nose and mouth, ensuring a good seal (Figure 6). Rescue breaths are administered by blowing steadily into the infant's mouth and nose over the course of one second while watching the chest rise. The rescuer should remove their mouth from the infant's mouth and watch the chest fall, before repeating the process four more times.

Infants will preferentially breathe through their nose; in part due to the size and position of the tongue, consequently rescue breaths are delivered over both the nose and the mouth in infants (Hoo, 2004). Infants have underdeveloped diaphragmatic muscles, which results in the increased use of abdominal muscles to breathe. Therefore, the rescuer should observe both chest and abdominal movement when assessing breathing. Infants and children have lower respiratory reserves due to small lung volume and lower numbers of alveoli, which facilitate gaseous exchange; therefore initial rescue breaths and more frequent breaths are required (Randall, 2005).
Circulation
Once the rescuer has delivered five rescue breaths, they should assess for signs of life for no longer than 10 seconds as described earlier. In rescuers who are trained to check for a pulse, this can be done through feeling for a carotid pulse in children and a brachial pulse in infants for 10 seconds. It is important to recognise that studies have found that diagnosis of cardiac arrest by palpation of the pulse alone is unreliable as it takes at least 30 seconds to accomplish and speed and accuracy of diagnosis correlate to clinical experience (Tibballs and Weeranatna, 2010). Due to this, assessment for signs of life is much more widely advised than the checking of pulses to assess circulation.
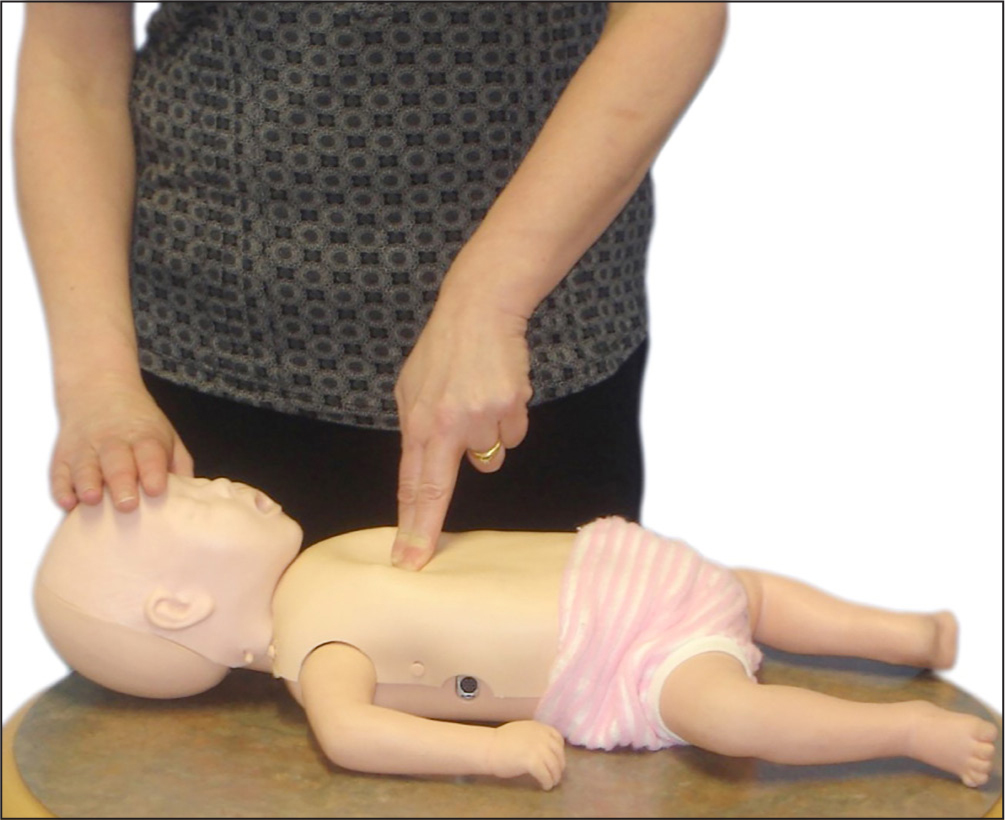
If there are no signs of life or the pulse is below 60 beats per minute then the rescuer will commence chest compressions at a rate of 100-120 beats per minute (RCUK, 2015). Bradycardia is associated with reduced cardiac output and, unless treated, bradycardia will cause hypoxia. In children and infants, the chest is compressed by locating the xiphisternum (the angle where the lowest ribs join in the middle), then compressing one finger's breadth above this point (Figure 7).

In children, the rescuer should place the heel of one hand over the sternum, lifting the fingers so the pressure is not applied over the ribs. The rescuer should then compress the sternum to at least one-third of the depth of the chest, approximately 5 cm, and repeat this 15 times at a rate of 100-120 compressions a minute (RCUK, 2015).
In infants, the rescuer should compress the sternum, using the tips of two fingers, to at least one-third of the depth of the chest, approximately 4 cm and repeat this 15 times at a rate of 100-120 compressions per minute (RCUK, 2015). The encircling technique is an alternative approach for infant compressions, whereby the rescuer places both of their thumbs flat, side by side on the infant's sternum with the tips pointing towards the infant's chin and presses down with their thumbs on the infant's sternum (Figure 8). Following chest compressions, the rescuer should deliver two breaths before continuing the cycle at a rate of 15 compressions to every two breaths.
Although infants and children have different shaped chests to adults, they have smaller hearts, which lie more horizontally and higher in the mediastinal cavity than adult hearts and this supports delivering chest compressions to one third of the depth of the chest (Novak, 2004). It is important to ensure that the depth and release of chest compressions allow the ventricles of the heart to expand and contract fully, which can be achieved by compressing the lower half of the sternum and ensuring full chest wall recoil before the next compression starts (Rossano and Naim, 2013).
Continuing resuscitation
If a rescuer is alone and no help has arrived following their shout, they should undertake 1 minute or 5 cycles of BLS before seeking further help. If the rescuer is delivering BLS to an infant or small child, it may be possible for them to carry them to get help, in order to minimise the delay in delivering BLS. If two or more rescuers are present, they should continue to deliver BLS at the 15:2 ratio until the child shows signs of life, qualified help arrives or the rescuers become exhausted.
Automated external defibrillator usage
Automated external defibrillators (AEDs) are found in many public areas across the UK and although these have been designed for use with adults, there are paediatric pads available, which adjust the energy level used to suit paediatric patients. Rescuers who have access to an AED will find instructions for the positioning of the pads in the AED box and will be guided by visual and verbal prompts from the AED and informed whether a shock is recommended and should be delivered (St John Ambulance, 2015). The rescuer must know to stop delivering chest compressions while the AED is assessing the heart rhythm and to ensure that they and others step away when a shock is delivered (St John Ambulance, 2015).
Points for good practice
Lee et al (2018) carried out a manikin study that showed that counting inflation breaths aloud improved the speed of rescuers resuming chest compressions during two-person paediatric cardiopulmonary resuscitation.
Studies have shown that when administering chest compressions to infants and children, rescuers frequently do not compress the chest as deep as the recommended depth or compress quick enough to meet the recommended rate of compressions (Everett and Weiner, 2012; Gregson et al, 2017).
Parents and carers of the child or infant will undoubtedly be in shock, therefore it is important to ensure that appropriate and timely information is shared. They will understand the urgency, and can often help if included and receive simple instructions (Stewart, 2019).
Conclusion
This article has identified the knowledge and skills necessary to deliver basic life support to infants and children following RCUK guidelines as summarised in Figure 9. Healthcare professionals responsible for caring for infants and children should familiarise themselves with this process as they are required to demonstrate that they have the knowledge, skills and confidence to provide basic life support if necessary (NMC, 2018a).