Body dysmorphic disorder (BDD) is a mental health condition, on the obsessive-compulsive spectrum (Schneider et al, 2017a). BDD is understood as an obsessive disorder associated with an intense preoccupation with perceived or imagined flaws in appearance (American Psychiatric Association, 2013). Obsession with flaws in appearance causes compulsive checking of these flaws, which leads to functional impairment, increased desire to have cosmetic surgery and comorbidities such as depression (Krebs et al, 2017a). Several studies have suggested that more severe cases of BDD in adults are associated with abuse and trauma, bullying and negative social experiences during childhood (Webb et al, 2015; Krebs et al, 2017a). The symptoms of BDD, such as obsessive mirror checking, can lead to toxic stress and numerous studies have identified the negative psychological impacts of BDD in adolescence (Schneider et al, 2017b). Research also suggests that the earlier the age of onset, the higher the probability of negative developmental impact and comorbidities; including a higher likelihood of suicide (Bjornsson et al, 2013; Schneider et al, 2019). Throughout this article the period of development will be referred to as adolescence and the population will be referred to as young people/person.
Prevalence of BDD
BDD is an increasingly prevalent condition (Himanshu et al, 2020) with psychological and functional impacts, so recognition and treatment is essential. Furthermore, suicide rates in the UK among 10-24-year-olds have increased significantly in recent years (Office for National Statistics, 2019; 2020) and BDD's association with high suicide rates makes this condition pressingly relevant (Bjornsson et al, 2013; Schneider et al, 2019).
BDD is most prevalent in adolescence, at around 1-2% (Schneider et al, 2017b; Enander et al, 2018). Phillips et al (2006) suggested symptoms of BDD occur from age 13 and age of onset is age 16. This was supported by a later study by Bjornsson et al (2013), who suggested symptoms occur from age 12-13 years. Schneider et al (2019) found BDD was more common in the 15-18 age range, rather than 12-14, but agreed with Bjornsson et al (2013) that symptoms begin occurring at these ages. However, these studies have limitations because symptoms can occur long before diagnosis, so it is difficult to assess the exact age of onset. In line with the research, it can be concluded that occurrence of BDD symptoms start during younger adolescence, but diagnosis is more common in older adolescence.
Few studies have examined gender differences in BDD and Schneider et al (2017b) suggested there are no significant gender differences. Another study by Veale et al (2016) suggested it is difficult to conclude whether there are gender differences in BDD occurrence. However, Enander et al (2018) suggested there is a higher prevalence of symptoms in females and similar studies agreed with this (Mayville et al, 1999; Schneider et al, 2018).
Brain development
The brain's prefrontal cortex (Figure 1) is responsible for decision making and develops continuously during adolescence and into adulthood (Steinberg, 2008). Young people are more likely to engage with risk-taking behaviours and impulse responses because their ‘decision-making’ brain is still developing, and they use emotions to respond to situations, which are controlled by the amygdala (Steinberg, 2008). On the other hand, adults make decisions based on their past experiences, using their prefrontal cortex (Steinberg, 2008). Peer inclusion and acceptance is of high importance to young people and social comparisons are much more common (Blakemore, 2018). A study by Somerville et al (2013) found that young people's emotional arousal and levels of perspiration increased when they thought they were being watched by peers whereas in adults and children this was not the case. The participants were not actually being observed but the young people's anticipation they were being watched was enough to cause increases in emotional arousal and stress. In accordance with this, Tatangelo and Ricciardelli (2017) found that children aged 8-10 (pre-adolescence) were unaware they were making social comparisons so negative peer comparisons did not affect them. Somerville et al (2013) found that young people used the medial prefrontal cortex more than both children and adults; this is significant because this part of the brain is responsible for reflecting on oneself.
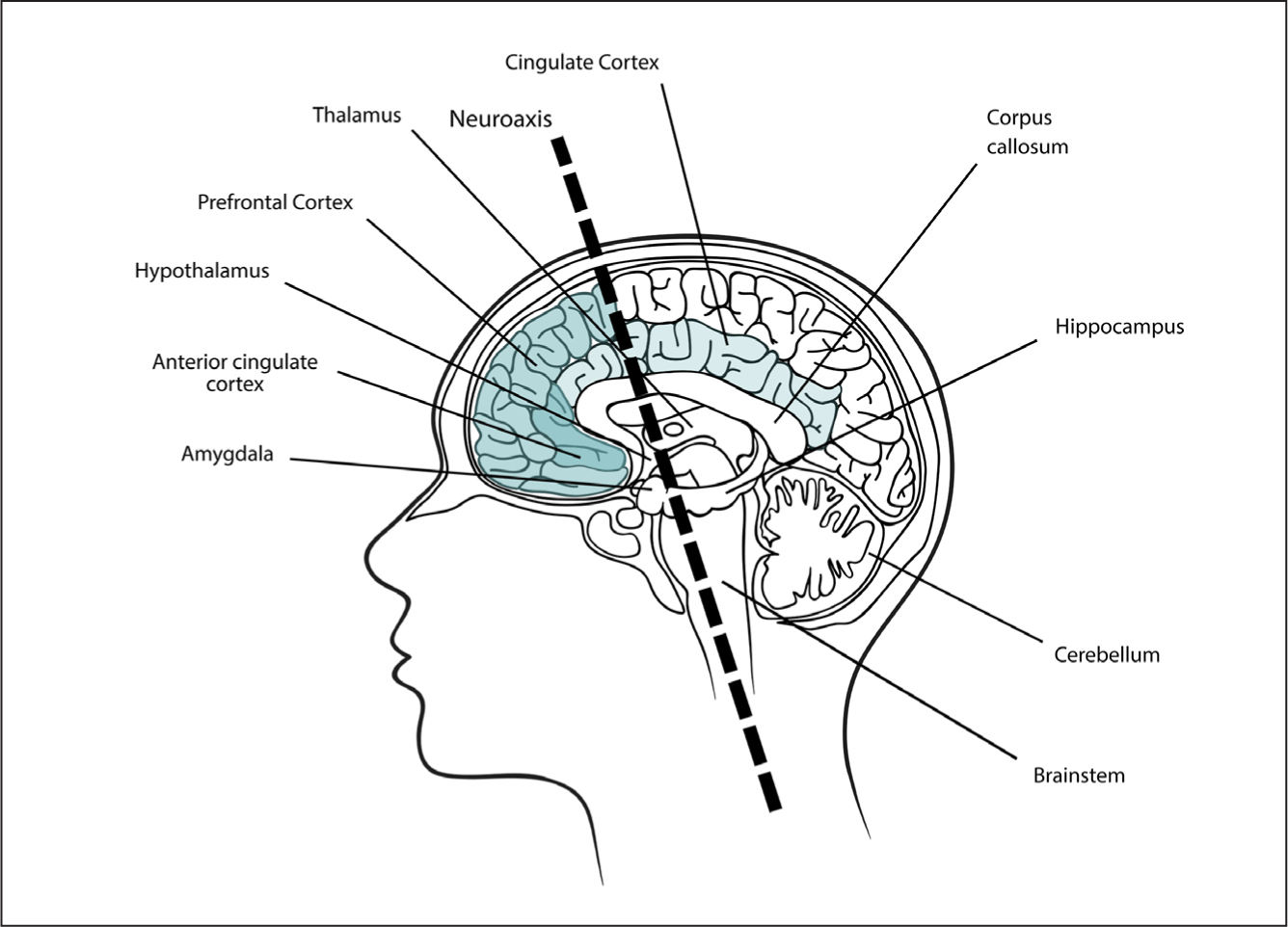
Adults use their ventrolateral prefrontal cortex to cope with negative evaluations from peers; when they use this area, they report low levels of distress from peer evaluations. When young people use this area, they also report lower levels of distress (Sebastian et al, 2011) but young people have a reduced ability to cope with emotions and distress because the prefrontal cortex is underdeveloped (Mills et al, 2014). It can be concluded that due to young people's inclination to desire peer approval they are affected more profoundly by negative evaluations and exclusion by peers than children or adults. Young people understand the significance of peer evaluation and understand when peer comparisons are taking place (Blakemore, 2018), whereas children do not understand when they are being evaluated so negative evaluations do not impact them (Tatangelo and Ricciardelli, 2017). Similarly, adults understand the impact of peer comparisons but are more able to cope with peer evaluations because their prefrontal cortex is developed. During adolescence this is still developing, which is why young people struggle to cope with negative evaluations (Sebastian et al, 2011).
Causes of BDD in young people
Fang and Hofmann (2010) suggested that symptoms of social anxiety can increase the risk of BDD developing, which supports the National Institute for Health and Care Excellence (NICE) (2005) BDD guidelines. Lavell et al (2014) found that when young people were teased based on their appearance, they experienced heightened BDD symptoms and anxiety. Similarly, Webb et al (2015) highlighted that the symptoms only worsened when the teasing was based on their appearance and not when teasing was general. Young people who experience teasing or bullying are likely to have low self-esteem (Blakemore, 2018) and BDD is linked to low self-esteem (Krebs et al, 2017b). Conclusions can be drawn that bullying and peer teasing can have a profound effect on young people's perceptions of themselves and may encourage them to make changes so they can be accepted by peers. This is significant because numerous studies have concluded that negative social experiences and fear of negative peers' evaluations can increase symptoms of BDD and increase the likelihood of a diagnosis (Dyl et al, 2006; Webb et al, 2015). Young people can learn preoccupations about their appearance from negative comments from peers (Grusec, 1992).
High media consumption in young people and children has been linked to body image dissatisfaction in numerous studies (Gallagher et al, 2015). Social media allows young people to communicate with each other, but it can become a platform where social learning takes place due to peer comparisons and bullying (Grusec, 1992). Bell and Dittmar (2011) concluded that the media exposes young people to unrealistic expectations of so-called perfect body types and ways in which everyone should look. Media images contain both subliminal and apparent propaganda, which can cause young people to absorb the content and become indoctrinated with false appearance ideologies (Himanshu et al, 2020), potentially leading to poor body image. Consequently, due to BDD's obsessive nature, young people become more obsessed with their perceived flaws (Himanshu et al, 2020). Conclusions can be drawn that influence of peers, peer comparisons, bullying and high social media use can significantly impact on BDD and BDD symptoms in adolescence.
Nevertheless, media can also positively impact on adolescents' mental health. Clifton et al (2013) found young people often sought mental health support online and via peers, so exposure to positive mental health support delivered online and peer support could improve the mental health of young people. This conclusion also supports Himanshu et al (2020), who suggested that online education is a good way to promote positive body image and in turn BDD symptoms. Online treatment is being developed as this would allow faster access to treatment and primary studies have shown this has significantly reduced symptoms (Hong et al, 2018).
Body integrity identity disorder
Another aspect of BDD involves a desire to amputate a healthy limb or to become paralysed, also known as body integrity identity disorder. Patients feel the affected limb is alien to them or should not be there (Müller, 2009). There is little research on the prevalence of this form of BDD in young people but some research has concluded onset is in early childhood (Blom et al, 2012). Individuals with BIID can present to healthcare services electively or in an emergency; patients may seek cosmetic surgery to amputate their ‘alien limb’ or attempt self-mutilation in order to achieve their desired disability (Chan et al, 2011). There is much controversy surrounding the perceived causes of BIID, some research suggests it is probable that BIID is a neuropsychological disturbance (Müller, 2009). Patients presenting with BIID are likely to have suffered childhood trauma similar to BDD patients or have increased exposure to amputees (Blom et al, 2012). Thus, it could be suggested that similarly to BDD, BIID patients desire to become disabled accumulates from exposure to amputees and self-formed ideologies of the perfect body, BIID patients may seek amputation to fit in with their desired society. More recent research concluded that BIID is not a body image disorder as patients retain sensory function of the affected limbs, thus more research is required to identify its causes (Stone et al, 2020).
Support and treatment
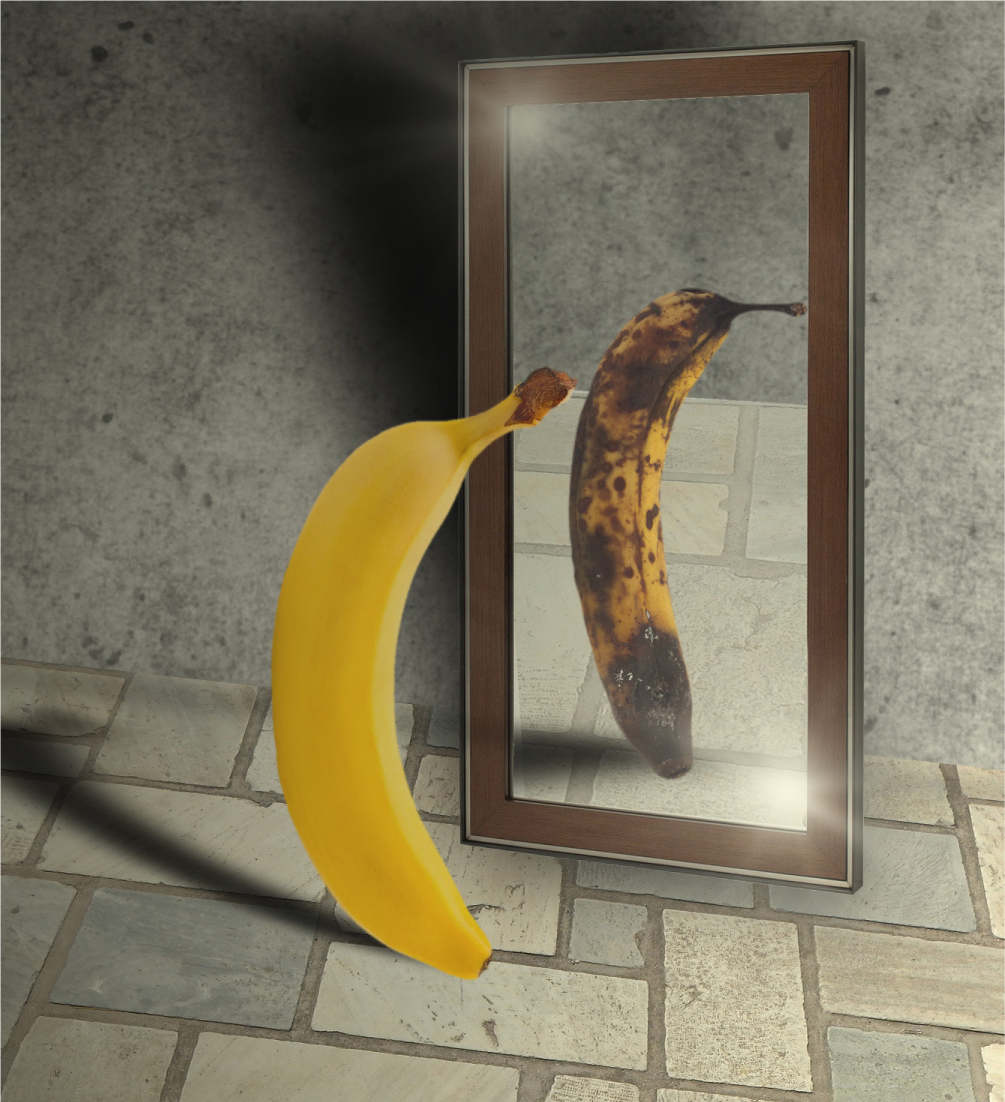
There is a clear link between poor body image and BDD and providing young people with education about the superficiality of images has been shown to be beneficial in safeguarding them from negative exposure to media and unachievable ideologies of body image (Himanshu et al, 2020). BDD is characterised by having delusional flaws in appearance and having looked at the literature it could be suggested that these delusions can be worsened by media exposure, if media exposure is negatively impacting on body image. Krebs et al (2019) concluded that ‘self-orientated perfectionism’ increased symptoms of BDD and young people had a desire to perfect themselves. This ties in with Somerville et al's (2013) research, showing increased brain activity in the area of the brain that reflects on oneself is an indication of why young people are most prone to BDD. Furthermore, this literature suggests that reducing young people's desire for self-perfection would reduce symptoms of BDD.
NICE (2005) recommends that the primary treatment option for BDD in adolescence should be cognitive behavioural therapy (CBT). A study by Krebs et al (2017b) concluded that CBT is an effective way to manage BDD and CBT participants had significantly reduced symptoms. NICE (2005) and Krebs et al (2017b) found CBT based on developmental stage was the most effective form of treatment. Himanshu et al (2020) found educating young people on the reality of fake ideologies improved BDD symptoms and they encouraged professionals to promote positive body image. This supports Hong et al (2018) who concluded that treatment should focus on changing patients' mindsets and understanding of themselves and move away from damaging superficialities, and would support Krebs et al's (2019) findings that CBT that focused on reducing desire for self-perfection effectively reduced BDD symptoms.
Numerous studies have identified that BDD is associated with high rates of suicide (Bjornsson et al, 2013; Schneider et al, 2017b) so screening for suicidal risk and suicidal thoughts should be included in initial assessments to reduce risks (NICE, 2005). Considering the types of treatment offered to young people is important, for example, selective serotonin reuptake inhibitors can have side effects such as suicidal thoughts, and monitoring is essential when prescribing them (NICE, 2005).
It is paramount to engage young people in their treatment, ensuring they are part of all decision making and where appropriate their consent is sought. Gillick competence allows young people under 16 to make their own decisions about their healthcare, if they are deemed competent (Norman, 2018). This may involve refusing psychiatric treatment such as CBT. However, people can be treated without consent, should they be at risk or unable to make informed decisions for themselves due to mental illness (Cave, 2013). Consent can also be an issue for individuals seeking aesthetic interventions, rather than psychiatric treatment—consent may not be informed if a severe mental illness is impacting on the adolescent's decision making (Nejadsarvari and Ebrahimi, 2014). These legalities are important to consider because BDD involves delusional flaws, which may cause denial and treatment refusal.
Himanshu et al (2020) found that young people are at risk of seeking surgical interventions in order to correct perceived flaws. BDD patients seeking interventions do not typically need them, because their perceived flaws are delusional. Therefore, professionals have an ethical dilemma about whether they should treat or not treat these patients (Higgins and Wysong, 2018). Pavan et al (2008) concluded that even following surgical or dermatological interventions, patients' BDD symptoms were rarely ameliorated and it would be unethical to provide interventions that do not improve patients' symptoms.
Ethics is paramount in BIID; surgical amputation of a healthy limb could be considered unethical and illegal (Chan et al, 2011). The debate is whether failure to electively perform such procedures would increase the risk of self-mutilation, treatment can only be justified if the benefit for the patient would outweigh the harm (Chan et al, 2011).
Screening tools for BDD should be implemented into multiple areas, including surgical units, aesthetic services and general practice, to identify potential BDD patients (Higgins and Wysong, 2018). Following screening, multidisciplinary team (MDT) involvement in a comprehensive and thorough assessment and diagnosis is required, preventing unnecessary interventions occurring and enabling organisations to direct young people towards psychiatric support (NICE, 2005). The MDT involves specialist professionals with experience of BDD to come together and provide care adapted to different developmental stages (NICE, 2005) as treatment is more effective when tailored to developmental stage (Krebs et al, 2017b). MDT working also raises awareness and improves understanding of other mental health disorders (NICE, 2005).
Conclusion
The nurse's role is essential in recognising and supporting young people with BDD (Thompson et al, 2012). Nurses who effectively develop therapeutic relationships can connect with patients on a holistic level; young people are more likely to seek support when they have a therapeutic bond with professionals (Norman, 2018). Concordance is preferred when working with young people and enables more positive outcomes, which can be achieved through effective therapeutic relationships (NICE, 2005). Professionals working with patients with BDD or potential patients can have a positive impact by promoting positive self-image/body image and providing education on false ideologies. Early intervention is associated with improved outcomes and reduced risks of unnecessary aesthetic procedures (Hong et al, 2018). Furthermore, safeguarding vulnerable young people is paramount therefore nurses must have secure knowledge of mental health conditions and the legislation.

